Translate this page into:
Sagittal Normal Limits of Lumbosacral Spine in a Large Adult Population: A Quantitative Magnetic Resonance Imaging Analysis
Address for correspondence: Dr. Antonio Pierro, Department of Radiology, Fondazione di Ricerca e Cura “Giovanni Paolo II”, Università Cattolica del Sacro Cuore, Campobasso, Italy. E-mail: apierrojonico@libero.it
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
The objective of this study was to determine, using magnetic resonance imaging (MRI) of the lumbosacral spine from L1 to S1, the values of the normal sagittal diameter of the spinal canal (SCD), sagittal diameter of the dural sac (DSD), and the normal values of dural sac ratio (DSR) in a large nonsymptomatic adult population and to discriminate whether a vertebral canal is pathological or nonpathological for dural ectasia and/or stenosis.
Materials and Methods:
Six hundred and four patients were prospectively enrolled. All measurements were performed on MRI sagittal T1- and T2-weighted images. The 95% confidence interval (95% CI), defined as mean ± 1.96 standard deviation, was determined for each metric. The upper limit of 95% CI was considered the cutoff value for the normal DSR; the lower limit of 95% CI was considered the cutoff value for the normal SCD.
Results:
SCD cutoff values from L1 to S1 ranged from 14.5–10.1 mm (males) to 15.0–9.9 mm (females). DSD ratios at S1 and L4 level show a significant difference in male and female groups: 11% of S1/L4 values exceeded 1 in male group while only 4% of S1/L4 values exceeded 1 in female group. Mean DSR at each level was significantly higher in female patients than in male patients (P < 0.001), ranging from 0.70 to 0.56 (male) and from 0.82 to 0.63 (female).
Conclusions:
We determined the cutoff values for the normal DSR and for the normal SCD. Our findings show the relevant discrepancies with respect to literature data for diagnosis of lumbar stenosis and/or dural ectasia.
Keywords
Dural ectasia
lumbar stenosis
Marfan syndrome
spine

INTRODUCTION
Magnetic resonance imaging (MRI) is currently considered the best imaging method to investigate back pain.[123] Various conditions may be responsible for back pain such as disk degeneration, central canal stenosis, metastases, spinal compression fractures, and others.[1]
The lumbar spinal stenosis is characterized by the narrowing of the spinal canal and foramina, with consequent compression of lumbosacral nerve roots or the cauda equina.[4] Neurogenic claudication and radiculopathy with or without intermittent radicular nerve pain are major symptoms; it is commonly classified into primary (congenital) stenosis and secondary (acquired) stenosis, respectively, due to congenital anomalies and degenerative process, trauma, infection, surgery, bony overgrowth, or metabolic and endocrine disorders.[456]
The recognition of secondary stenosis is not very difficult for the radiologist on MRI. On the other hand, it can be very difficult to define the presence of spinal canal stenosis in patients with no acquired disorder. The vertebrae of patients with congenital lumbar stenosis is characterized by thick and short pedicles,[7] causing a reduced sagittal diameter of the spinal canal.
The aim of this paper was to measure, in the sagittal plane of MRI images, the diameter of the spinal canal diameter (SCD), the vertebral body diameter (VBD), and the dural sac diameter (DSD) from L1 to S1 level in a large population of 604 subjects free of known diseases, young adults not suffering from degenerative disease of the spine. The rigorous definition of the ranges of normal measurements of the lumbosacral spinal canal could allow to identify all conditions in which there is a significant reduction in the size of the vertebral canal and provide to clinicians a quantitative support to diagnose a lumbosacral stenosis in the presence of a clinical suspicion. In addition, the measurement of vertebral body and dural sac provided the values of dural sac ratio (DSR), particularly useful in assessing patients with dural ectasia.[8] This condition was defined as a major criterion to diagnose the Marfan syndrome.[9]
MATERIALS AND METHODS
Study population
In the period between January 2007 and July 2012, MRI scans obtained in 604 patients were selected over the entire adult population referred to our department for MRI of the lumbosacral spine. With the aim to obtain the normal sagittal diameters of the lumbar canal, these selected patients strictly followed the exclusion criteria shown in Table 1. We selected patients aged between 20 and 45 years to obtain a population with (i) a completed spinal development and (ii) absence of significant pathological conditions (e.g., degenerative arthrosis). Coincidentally on the total sample of 604 patients, 302 were male and 302 female. In this study, all analyzed subjects came from the same geographical area, i.e., from the regions of Central and Southern Italy. In addition, all subjects belong to the same Caucasian race. The body weight and height were evaluated in all patients to correlate such data with the results.

Magnetic resonance imaging
Spine imaging was performed using a 1.5-T MRI imaging system (GE Signa Excite HD, GE Medical Systems, Milwaukee, WI, USA). Measurements were performed on sagittal T1-weighted (repetition time ms/echo time ms, 420/8) and T2-weighted (repetition time ms/echo time ms, 2700/102) fast spin echo sequences. Slice thickness was 4 mm, spacing was 0.4 mm, the matrix was 384 × 224, and the field of view was 320 mm × 320 mm. The number of excitations was 4.
Measurements
All measurements were performed by three radiologists (AP, EC, and MC) with more than 10 years of experience in musculoskeletal radiology and neuroradiology. The simultaneous evaluation of both T1- and T2-weighted images allowed an increased accuracy in delineating all the anatomical structures under interest (the anterior epidural adipose tissue, the ventral surface of the dural sac, etc.).
Sagittal diameters of the lumbar spine (spinal canal, dural sac, and vertebral body) were assessed. The SCDs, DSD, and VBDs were obtained at each level of the lumbar vertebral column from L1 to the first sacral vertebra (S1) as shown in Figures 1 and 2. In detail, the anteroposterior SCD was obtained perpendicularly to the long axis of the spinal canal from the posterior wall of the vertebra at the midportion to the front edge of lamina. At the same level, the anteroposterior VBD of the corresponding vertebra and DSD were measured.

- Detailed scheme of the measurements made on the sagittal magnetic resonance images. (A) the sagittal diameter of the canal was drawn up by the middle third of the posterior wall of the vertebra until the front edge of the base of the spinous process, (B) at the same level, we measured the anteroposterior diameter of the dural sac, and (C) we measured the anteroposterior diameter of the soma of the corresponding vertebra.
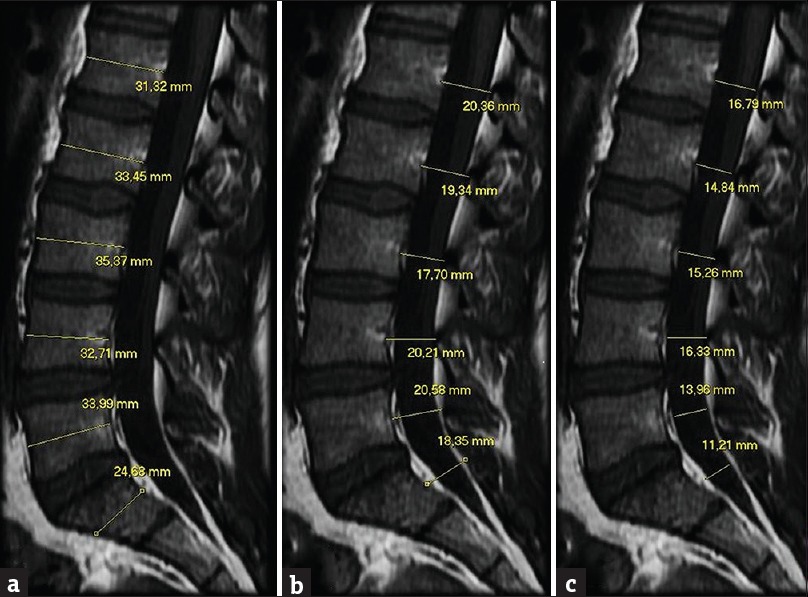
- A 30-year-old asymptomatic man. Magnetic resonance imaging (T1-weighted): Measurements were obtained on the sagittal images, in the stretch between L1 and S1: (a) anterior-posterior diameter of the vertebral body, (b) anteroposterior diameter of the spinal canal, and (c) anteroposterior diameter of the dural sac.
At each level, the DSR was calculated as the quotient of DSD to VBD.
Data analysis
The 95% confidence interval (CI), defined as mean ± 1.96 standard deviation (SD), was then determined for each metric. The upper limit of 95% CI was considered the cutoff value for the normal DSR. This means that patients exhibiting DSR values greater than cutoff value have to be considered for dural ectasia. On the other hand, the lower limit of 95% CI was considered the cutoff value for the normal SCD. This means that patients exhibiting SCD values lower than cutoff value have to be considered for stenosis.
In addition, we investigated the DSD ratio at S1 and L4 level. This evaluation was performed because a major criterion for dural ectasia is when the DSD at S1 is greater than at L4 (demonstrating that the dural sac is not tapering off).
All data are described in terms of mean and SDs for metric measurements and as percentages for counted data. A detailed analysis regarding differences between male and female patients was performed. Comparisons between groups are obtained by nonpaired Student's t-test; a P < 0.05 was considered to indicate significant differences. A normality test was performed for each distribution. Pearson correlation coefficient was used to examine the potential dependence of outcome parameters on weight and height. All statistical computations were performed using SPSS ver. 11.5 (SPSS, Chicago, IL, USA) software package.
RESULTS
The SCD values (mean and SD) from L1 to S1 are presented in Table 2. There was no significant differences between male and female subgroups at each level (P > 0.05), except at L5 (P = 0.031) and S1 (P < 0.001). In both groups, there was a decrease of SCD from L1 to L4, followed by an increase at L5 and a large decrease at S1 level. Cutoff values for L1 to S1 (95% CI) are also listed in Table 2.

The VBD values (mean and SD) from L1 to S1 are presented in Table 3. The mean VBD at each level was significantly higher in male patients than in female patients (P < 0.001). In both groups, there was an increase of VBD from L1 to L5, followed by a large decrease at S1 level.

The DSD values (mean and SD) from L1 to S1 are presented in Table 4. The mean DSD at each level was significantly higher in female patients than in male patients (P < 0.001), except at L5 and S1. In both groups, there was a monotonic decrease of DSD from L1 to S1.

Regarding the DSD ratio at S1 and L4 level, our analyses show a significant difference in male and female groups: 11% of S1/L4 values exceed 1 in male group while only 4% of S1/L4 values exceed 1 in female group. This is shown in Figure 3, showing cumulative percentage plots for DSD ratio at S1 and L4 level. Considering the 95% CI in normal subjects, normal values for the DSD ratio at S1 and L4 level resulted < 1 in female and < 1.2 in male.

- Cumulative percentage plots for dural sac diameter ratios at S1 and L4 level in male (solid line) and female (dotted line) groups.
Table 5 shows the DSR values at each level from L1 to S1. In both groups, there was a monotonic decrease of DSR from L1 to S1. The mean DSR at each level was significantly higher in female patients than in male patients (P < 0.001). Cutoff values from L1 to S1 (95% CI) are listed in Table 5. Figure 4 shows the differences between the cumulative percentage plots for DSR values at L1 in male (solid line) and female (dotted line) groups.


- Cumulative percentage plots for dural sac ratio values at L1 in male (solid line) and female (dotted line) groups.
No correlation was found between all obtained metrics and the weight and height of the patients. In particular, SCD, DSD, and DSR were not correlated with weight and height at any vertebral level from L1 to S1 (the Pearson correlation indexes were found: R2 < 0.1 at all levels).
As an example, in Figure 5, we show the comparison between two young patients of the same age, one asymptomatic and the other with the typical symptomatology of the spinal canal stenosis, i.e., chronic low back pain and clinical signs of neurogenic claudication associated to early degenerative change of the lumbar column. In this last case, we show that the stenotic segment involves only the stretch from L1 and L4, in which the amplitude measurements of the spinal canal were found to be below our cutoff (L1: 12.1, L2: 9.5, L3: 9.7, and L4 9.2 mm). On the contrary, the results at L5 (12.7 mm) and S1 (10.4 mm) are within the normality ranges. This means that MRI metameric normal cutoff values must be evaluated and defined for each lumbosacral vertebra.
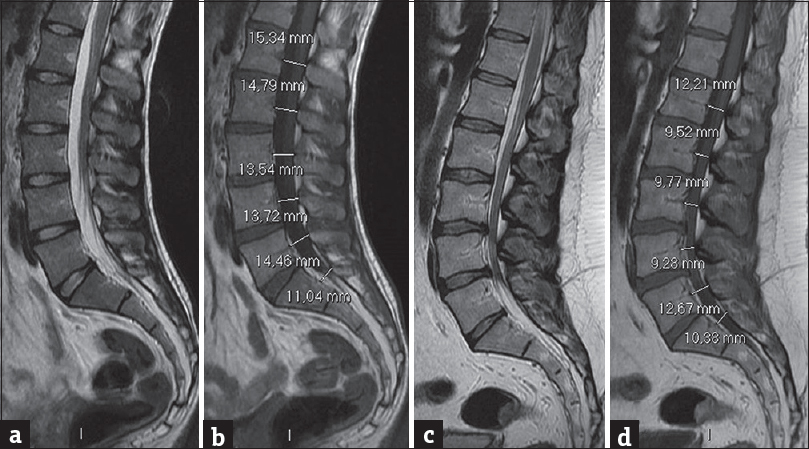
- Two 32-year-old patients, one asymptomatic (a and b) and the other (c and d) with chronic low back pain and clinical signs of neurogenic claudication. (a and b) Sagittal magnetic resonance images, T2- and T1-weighted, of a patient with normal values of the amplitude of the spinal canal. (c and d) Sagittal magnetic resonance images, T2- and T1-weighted, of a patient with congenital stenosis of the spinal canal, early degenerative changes, with chronic low back pain and clinical signs of neurogenic claudication. In the last case, all sagittal diameters, except at the level of L5 and S1, are markedly reduced and the severity of the stenosis can be quantitatively defined at each level between L1 and L4.
DISCUSSION
We evaluated the values of the normal sagittal diameter of the spinal canal, sagittal DSD, and the DSR in a large asymptomatic adult population, to discriminate whether a vertebral canal is pathological or nonpathological for dural ectasia and/or stenosis. To the best of our knowledge, there are no other studies in the literature based on such a large population of normal subjects which defined the cutoff values for normality of aforementioned morphological parameters. The aim was to provide robust and quantitative data to radiologists and clinicians community, to communicate a possible diagnosis through objective rather than qualitative criteria. In our opinion, it is important to quantify the stenosis rather than visual inspection.
In clinical practice, the accurate knowledge of the normal lumbar spinal canal measurements is of extreme importance since a reduction of its size predisposes to back pain and spinal canal stenosis. Many studies were carried out for this purpose, indicating a large variability of threshold values for the maximum and minimum diameter of the spinal canal in different populations.[10]
In congenital vertebral stenosis, the transverse diameter can be normal whereas the sagittal diameter is reduced because of thickening of the laminae and articular processes and sometimes because of short pedicles.[11] The authors of the Delphi Survey study[12] recommend the use of the anteroposterior diameter of vertebral canal in clinical practice and in clinical studies.
Many authors have carried out measurements of anatomical specimens, X-rays, and examination of computed tomography and MRI to identify normal and abnormal sagittal diameter of the spinal canal. According to these studies, the minimum sagittal diameter of the spinal canal was found ranging between 8 and 15 mm.[1213141516171819]
In clinical practice, a generic sagittal diameter of the spinal canal < 12 mm is considered the accepted definition of congenital stenosis.[12] However, our study revealed that for each vertebral level from L1 to S1, a specific MRI cutoff value can be associated to the narrowing of the spinal canal [Table 2 and Figure 5c, d].
In contrast to our choice in using the sagittal diameter of spinal canal, other clinicians prefer to use the dural sac cross-sectional area (DSCA) for lumbar spinal stenosis assessment. However, the DSCA measurement can be significantly affected by the slice orientation. Some authors[2021] have proposed a qualitative morphological classification to assess the severity of spinal stenosis; this classification shows significantly less variability on slice orientation than DSCA measurement and thus offers a more reliable means for assessing severity of stenosis. This qualitative grading system is based on the morphologic appearance of the dural sac as seen on T2-weighted axial images and on the cerebrospinal fluid/rootlet ratio. We believe that qualitative criterion is useful to evaluate the spinal canal stenosis suspicion, but it is a subjective method that does not rely on reproducible quantitative values; for this reason it is necessary to use well-established quantitative criteria for an appropriate assessment of the anteroposterior diameter of the osseous spinal canal. The other factor is the shape of the spinal canal which is not a constant parameter. The canal shape is not uniform along the lumbar vertebrae ranging from circular or rounded shape in the upper lumbar vertebrae to triangular in the midlumbar vertebrae to trefoil in the lower lumbar vertebrae.[22] Last, the anteroposterior diameter of the spinal canal was shown to statistically correlate with its cross-sectional area, justifying its use as metric of spinal canal size.[23]
An interesting result in the present paper is the large sagittal canal diameter cutoff values in females with respect to males. We believe that this result can be attributed to a fundamental difference in spinal lumbar shape between genders. In particular, the pregnancy is a condition needing new equilibriums. A recent study by Hay et al.,[24] aiming to revisit the nature of lumbar curve in males and females stated that the morphological characteristics of the female spine are probably developed to reduce stress on the vertebral elements and nerve roots during pregnancy. Hence, a wider spinal canal in women may be an evolutionary result aimed at increasing comfort and mobility during pregnancy.
It is well know that the DSR is a useful metric in the assessment of dural ectasia in patients with Marfan syndrome because its pathological increase implies a condition of dural ectasia. Dural ectasia was defined as one major criterion to diagnosis of the Marfan syndrome.
Oosterhof et al.,[8] using MRI of the lumbosacral spine, determined the DSR values in normal subjects defining the cutoff values for the normal DSR. DSR values greater than the cutoff value were considered abnormal and indicative of dural ectasia. The authors concluded that a DSR >0.57 at S1 or a DSR >0.47 at L3 was almost sufficient for diagnosing Marfan syndrome in young adults.
Our study shows values significantly greater than those reported by Oosterhof et al. [Table 6]. From the comparison of our results with the cutoff values of Oosterhof et al., study taken as reference, it can be deduced that the 30%, 36%, 49%, 34%, 30%, and 18% of our patients would be diagnosed as Marfan at the level of L1, L2, L3, L4, L5, and S1, respectively.

Therefore, this shows that the cutoff values proposed by Oosterhof et al., are in reality too small compared to the normal values resulted from the evaluation of a large population like ours. This consideration agrees with the study of Lundby et al.,[25] where they found the measurements meeting the criteria of in 12% subjects at the level of L1 and 19% subjects at the level of L5. Lundby et al., proposed at the level of S1 a cutoff of 0.59 which is still significantly smaller than our cutoff of normality at the same level (0.72). Using Oosterhof's method, the study of Weigang et al.,[26] reported that 94% of the patients with and 44% of the patients without Marfan syndrome fulfilled the criteria of dural ectasia, pointing out that these cutoffs were too small.
We want to underline that all these values are applicable only to adults because the DSR in healthy children is higher than in healthy adults. During growth, DSR decreases by approximately 10% every 3 years.[27]
Another important criterion for the dural ectasia has been proposed when the DSD at the level of S1 is greater than DSD at the level of L4,[28] showing that the dural sac is not tapering off. From our data on the DSD, we obtained that the average value at L4 was 13.3 mm while the average value at S1 was 9.9 mm. However, our data showed that there is a substantial number of normal patients in which the S1 diameter is greater than L4 diameter. On a gender differential basis, this happens in 4% of females and 11% of males. Therefore, with a 95% CI, S1/L4 ratio < 1 is the normal condition only for females, whereas for males, this ratio has to be considered normal if < 1.2. A similar result was reported by Lundby et al.,[25] who found that the maximum sagittal DSD at the level of S1 was greater than that at the level of L4 in 5% of cases in the control group.
It has been reported that spinal stenosis may be associated with a reduction in the amount of epidural fat around the stenotic area; on the other hand, excessive epidural fat may cause compression of dural sac.[29] In our study, no patients had any conditions which may result in alteration of the distribution and thickness of the epidural fat, such as kyphoscoliosis, lumbar spinal stenosis, long-term steroid therapy, or conditions characterized by endogenous steroid hypersecretion. For these reasons, we considered that the amount of epidural fat fell within the normal range and it was not considered as a parameter altering the measurements in our population.
We want to emphasize that the values obtained in our study are related to a homogeneous population of patients from the same geographical area. Our results may not be applicable in populations different from the Caucasian population; for example, it was observed that in Indian and Nepalese population, the pedicle dimensions differ significantly from those of caucasian populations.[3031]
CONCLUSIONS
The accurate and quantitative definition of the normality range for these metrics may allow the physician to obtain more accurate diagnoses, avoiding duplication of diagnostic tests, and speeding up the timing of the diagnosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/35/213882
REFERENCES
- Lumbar spine MRI for low back pain: Indications and yield. AJR Am J Roentgenol. 2010;195:550-9.
- [Google Scholar]
- Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-91.
- [Google Scholar]
- Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002;137:586-97.
- [Google Scholar]
- Congenital lumbar spinal stenosis: A prospective, control-matched, cohort radiographic analysis. Spine J. 2005;5:615-22.
- [Google Scholar]
- Quantitative assessment of dural ectasia as a marker for Marfan syndrome. Radiology. 2001;220:514-8.
- [Google Scholar]
- Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet. 1996;62:417-26.
- [Google Scholar]
- Uncertainties in the diagnosis of lumbar spinal stenosis. Radiology. 2011;261:681-4.
- [Google Scholar]
- Results of surgical treatment of idiopathic developmental stenosis of the lumbar vertebral canal. A review of twenty-seven years’ experience. J Bone Joint Surg Br. 1977;59:181-8.
- [Google Scholar]
- Radiologic criteria for the diagnosis of spinal stenosis: Results of a Delphi Survey. Radiology. 2012;264:174-9.
- [Google Scholar]
- The morphometry and pathological anatomy of the lumbar spine in South African negroes and caucasoids with specific reference to spinal stenosis. J Bone Joint Surg Br. 1977;59:173-80.
- [Google Scholar]
- Quantitative assessment of the lumbar spinal canal by computed tomography. Radiology. 1980;134:137-43.
- [Google Scholar]
- Electromyographic and magnetic resonance imaging to predict lumbar stenosis, low-back pain, and no back symptoms. J Bone Joint Surg Am. 2007;89:358-66.
- [Google Scholar]
- The significance and principles of computerized axial tomography in idiopathic developmental stenosis of the bony lumbar vertebral canal. Spine (Phila Pa 1976). 1979;4:369-78.
- [Google Scholar]
- Spinal stenosis prevalence and association with symptoms: The Framingham Study. Spine J. 2009;9:545-50.
- [Google Scholar]
- MRI criteria of developmental lumbar spinal stenosis revisited. Bull NYU Hosp Jt Dis. 2011;69:303-7.
- [Google Scholar]
- Assessment of lumbar spinal canal morphology with digital computed tomography. Ortop Traumatol Rehabil. 2009;11:156-63.
- [Google Scholar]
- Is spinal stenosis assessment dependent on slice orientation? A magnetic resonance imaging study. Eur Spine J. 2012;21(Suppl 6):S760-4.
- [Google Scholar]
- Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976). 2010;35:1919-24.
- [Google Scholar]
- Geometrical dimensions and morphological study of the lumbar spinal canal in the normal Egyptian population. Orthopedics. 2013;36:e229-34.
- [Google Scholar]
- Does the anteroposterior diameter of the bony spinal canal reflect its size. An anatomical study? Surg Radiol Anat. 1991;13:289-91.
- [Google Scholar]
- Dural ectasia in Marfan syndrome: A case control study. AJNR Am J Neuroradiol. 2009;30:1534-40.
- [Google Scholar]
- Evaluation of three different measurement methods for dural ectasia in Marfan syndrome. Clin Radiol. 2006;61:971-8.
- [Google Scholar]
- Normal values of the sagittal diameter of the lumbar spine (vertebral body and dural sac) in children measured by MRI. Pediatr Radiol. 2005;35:419-24.
- [Google Scholar]
- MR evaluation of dural ectasia in Marfan syndrome: Reassessment of the established criteria in children, adolescents, and young adults. Radiology. 2005;234:535-41.
- [Google Scholar]
- Clinical implications of epidural fat in the spinal canal. A scanning electron microscopic study. Acta Anaesthesiol Belg. 2009;60:7-17.
- [Google Scholar]
- Morphometric study of the lumbar pedicle in the indian population as related to pedicular screw fixation. Spine (Phila Pa 1976). 2002;27:453-9.
- [Google Scholar]
- A morphometric study of lumbar spine pedicles in Nepalese population. JCMS Nepal. 2014;10:12-7.
- [Google Scholar]






