Translate this page into:
Unicystic Ameloblastoma Masquerading as Huge Periapical Lesion, both Clinically and Histopathologically: Two Case Reports with Review of Literature
Address for correspondence: Dr. Samapika Routray, Department of Oral Pathology and Microbiology,Institute of Dental Sciences, Siksha O Anusandhan University, Bhubaneswar - 751 003, Odisha, India. E-mail: drroutray.samapika@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Unicystic ameloblastoma (UA) is one of the variants of ameloblastoma. It manifests as unilocular radiolucency in the mandible or maxilla on X-ray scans. In very rare cases, it can appear as a localized periradicular radiolucent area, imitating a periapical lesion. In this article, we present two cases of UA that were initially misdiagnosed as periapical lesions. Subsequently, surgical enucleation was performed and the diagnosis of UA was confirmed histopathologically.
Keywords
Ameloblastoma
periapical lesion
unicystic ameloblastoma
unilocular lesion
INTRODUCTION

Unicystic ameloblastoma (UA) was first described by Robinson and Martinez in 1977, later described by Gardner in 1983. They have the same origin as ameloblastomas and are a less encountered variant, with no sexual or racial predilection, appearing during 2nd or 3rd decade of life, encountered asymptomatically in the posterior region of the mandible.[1]
Leider et al., proposed three pathogenic mechanisms for this cystic entity.[2]
-
Reduced enamel epithelium, associated with developing tooth, undergoes ameloblastic transformation with subsequent cystic development
-
Ameloblastomas arise in dentigerous or other types of odontogenic cysts in which neoplastic ameloblastoma epithelium is preceded temporarily by nonneoplastic stratified squamous epithelial lining.
-
A solid ameloblastoma undergoes cystic degeneration of ameloblastic islands with subsequent fusion of multiple microcysts and develops into a unicystic lesion.
Later, in 1992 World Health Organization (WHO) added classification and subtypes of UA.
These are:[3]
-
Luminal UA
-
Luminal and intraluminal UA
-
Luminal intraluminal and intramural UA
-
Luminal and intramural UA
In recent literature, molecular alterations indicating the origin of pathogenesis were also observed in ameloblastomas, such as monoclonal neoplasia, overall low cellular proliferation index, association of higher MIB-1 labeling index and microsatellite alterations, telomerase activity associated with p16 loss, and dysregulation of sonic hedgehog/patched (SHH/PTCH) pathway but their significance is still not clear.[4]
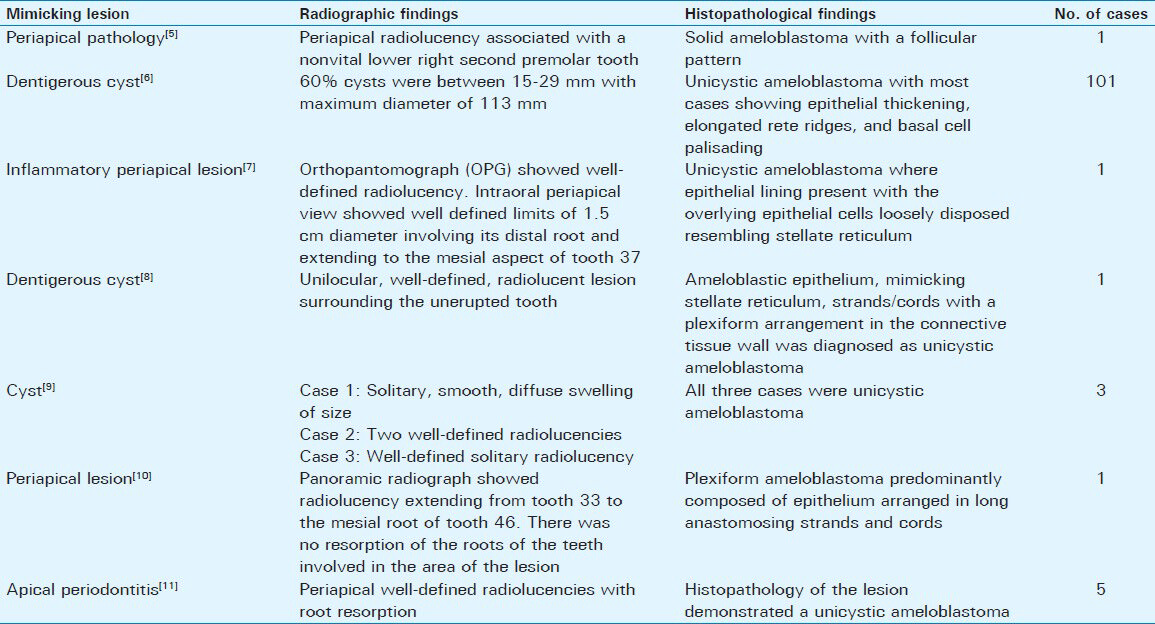
In our cases, the lesions were located in the upper posterior maxillary periradicular region. Further, the lesion was not associated with any unerupted tooth; but was located around carious or grossly decayed tooth with only root stumps. The occurrence of noninflammatory pathosis in the periradicular area was not considered as differential diagnosis initially in these cases. Most studies on periradicular lesions focus on radicular cysts and granulomas, as these lesions are highly prevalent and associated with pulpal necrosis and infection. When we searched for reports of lesions which initially presented as periapical pathology and later were confirmed to be of noninflammatory origin, especially ameloblastoma, we did come across a few as described in Table 1.[567891011]
RADIOLOGIC FEATURES
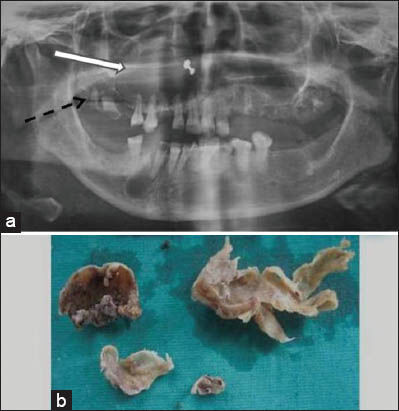
A 50-year-old female patient presented with a swelling in the upper left cheek region. On extraoral examination, we observed a single extraoral nontender swelling about 5 × 5 cm in size [Figure 1]. Intraoral swelling was approximately 5 × 6 cm, soft in consistency, and fluctuant in nature extending up to the midline of the palate medially and anteriorly up to tooth 23, posteriorly up to tooth 27, and involved the maxillary sinus. Hard tissue examination revealed a carious tooth present in position of tooth 27. Orthopantomograph (OPG) showed radiolucency of 5 × 5 cm size in relation to tooth 23 extending till tooth 27 in the periapex with thin radiolucent line [Figure 2a].

- Case 1. 50-year-old female with a huge swelling in the left cheek diagnosed with unicystic ameloblastoma. The extra-oral photograph shows swelling (white arrow) about 5 × 5 cm in size in the upper cheek.

- Case 1. 50-year-old female with a huge swelling in the left cheek diagnosed with unicystic ameloblastoma. a) Panoramic radiograph shows well-defined periradicular radiolucency (dashed arrow) in the left maxillary region in relation to carious tooth (root stump) 27 (white arrow). b) Postoperative view shows the area from where the cyst was enucleated. c) Photograph shows the excised tissues.
In a second case, a 34-year-old female patient presented to the outpatient department with complaints of pain and swelling in the back upper right tooth. The pain had increased gradually over 2 months. On clinical examination, we observed single extra-oral swelling about 5 × 5 cm in size, a hard and non-tender mass extending from lateral canthus of the eye to 3 cm away from tragus of ear anteroposteriorly, superiorly up to infraorbital margin, and inferiorly upto angle of mouth. Intra-orally the swelling was of approximately 7 × 7 cm in size, soft in consistency, and fluctuant in nature extending up to midline of the palate medially, anteriorly up to tooth 11, and posteriorly up to tooth 17 region. Buccally, it extended into vestibule in the tooth 14 to tooth 17 region resulting in obliteration. On hard tissue examination, there was a carious tooth in relation to tooth 17. Orthopantomograph (OPG) showed radiolucency of size 5 × 5 cm extending from tooth 11 to tooth 17 and to the periapical region giving a cystic appearance [Figure 3a].
- Case 2. 34-year-old female patient with complaints of pain and swelling in the back upper right tooth diagnosed with unicystic ameloblastoma. a) Panoramic radiograph shows well-defined periradicular radiolucency (white arrow) in the right maxillary region in relation to carious (root stump) 17 (dashed arrow). b) Photograph shows excised tissue.
PATHOLOGIC FEATURES
In both the cases our focus was on radicular cysts and granulomas, which are highly prevalent periapical lesions associated with carious tooth, pulpal necrosis, and infection. Other noninflammatory periapical lesions such as central giant cell granuloma, aneurysmal bone cyst, odontogenic keratocyst, and ameloblastoma were also considered in the differential diagnosis at a later stage. The patients were referred to the Department of Oral and Maxillofacial Surgery and surgical enucleation of the lesion under local anesthesia with adrenaline was performed. A full thickness flap was raised, and an encapsulated lesion was located between the enlarged buccal plates. After enlarging the bony access, the entire cyst was enucleated by performing curettage of the lesion in both the cases [Figure 2b]. The excised specimens were then submitted for histopathological examination [Figures 2c and 3b].
Histologically, in both the cases the cyst lining showed ameloblastic epithelium with tall columnar basal layer, subnuclear vacuoles, reverse nuclear polarity and thin layer of edematous, degenerate-appearing stellate cells [Figure 4]. In case 2, the cystic lining epithelium also demonstrated rete ridges in some areas with proliferation and archading epithelium mimicking a radicular cyst [Figure 5]. Focal areas within connective tissue demonstrate diffuse dense infiltration of chronic inflammatory cell infiltrate. Final diagnosis was made as UA with both being the luminal variant. Enucleation of the lesion was performed to completely extirpate the cystic lesion. Both patients had an uneventful postoperative recovery with no signs of recurrence during the 1-year follow-up examinations.

- Case 1. Hematoxylin and eosin stained section shows degenerating stellate cells (white arrow) along with ameloblastic epithelium (dashed arrow) (×40).

- Case 2. Hematoxylin and eosin stained section shows cystic lining epithelium with proliferation and archading epithelium (black arrow) (×40).
DISCUSSION
UA, a variant of ameloblastoma, refers to those cystic lesions that show clinical and radiologic characteristics of an odontogenic cyst like dentigerous, radicular, glandular odontogenic cyst, but in histologic examination show a typical ameloblastomatous epithelium lining part of the cyst cavity, with or without luminal and/or mural tumor proliferation.[3] This variant is believed to be less aggressive, tends to affect patients at a younger age and its response to enucleation or curettage is more favorable than the classic solid or multicystic ameloblastomas.
The diagnosis of UA is made only after microscopic examination of presumed cyst. Enucleation is the standard treatment protocol when the ameloblastic elements are confined to the lumen of the cyst, with or without intraluminal tumor extension. Local resection of area is indicated as a prophylactic measure if specimens show extension of tumor into fibrous cyst wall for any appreciable distance under radiographic observation. Recurrence rate of 10–20% has been reported after enucleation and curettage of UA. The age of the patient is another influencing factor related to the choice of treatment. As UA tends to affect young adolescent patients, the concern to minimize surgical trauma and permit jaw function and tooth development to proceed reasonably unimpaired should be one of the important aspects in tumor management. To obviate the problem of deformity, a simple enucleation was performed to remove the whole lesion after the completion of the tooth eruption in this region. While conservative surgery seems to have been justified in preference to mutilating radical surgery for these young patients, choice of treatment has to be considered in conjunction with other clinical and pathologic factors such as the size, location, and growth pattern of the tumor. Whatever surgical approach the surgeon decides to take, long-term follow-up is mandatory, to check for recurrence of UA.
CONCLUSION
A combination of radiological and histopathological examination is needed to provide definitive diagnosis of certain periapical lesions and is a must for diagnosis of ameloblastoma. Ameloblastoma is a benign epithelial neoplasm of odontogenic origin, and depending on the stage of development, it can mimic a periapical lesion and therefore should be considered during differential diagnosis.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/2/9/119156
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Ameloblastoma potential of follicular cyst. Oral Surg Oral Med Oral Pathol. 1965;20:206-8.
- [Google Scholar]
- Cystic Ameloblastoma: A clinicopathological analysis. Oral Surg Oral Med Oral Pathol. 1985;60:624-30.
- [Google Scholar]
- Odontogenic tumors and allied lesions. UK: Quintessence Publishing Co Ltd; 2005. p. :43-57.
- [Google Scholar]
- Review article: Current concepts of ameloblastoma pathogenesis. J Oral Pathol Med. 2010;39:585-91.
- [Google Scholar]
- Dentigerous cyst versus unicystic ameloblastoma-differential diagnosis in routine histology. J Oral Pathol Med. 2003;32:486-91.
- [Google Scholar]
- Unicystic ameloblastoma: A possible pitfall in periapical diagnosis. Int Endod J. 2005;38:334-40.
- [Google Scholar]
- Unicystic ameloblastoma in a child: A differential diagnosis from the dentigerous cyst and the inflammatory follicular cyst. J Dent Child. 2007;74:245-9.
- [Google Scholar]
- Unicystic ameloblastoma: Clinically a missed diagnostic entity-3 case reports. Ann Essen Dentistry. 2011;3:75-81.
- [Google Scholar]
- Plexiform ameloblastoma mimicking a periapical lesion: A diagnostic dilemma. J Conserv Dent. 2012;15:84-6.
- [Google Scholar]
- Unicystic ameloblastoma mimicking apical periodontitis: A case series. J Endod. 2013;39:145-8.
- [Google Scholar]






