Translate this page into:
The Use of Imaging in Management of Patients with Low Back Pain
Address for correspondence: Dr. Dinesh Rao, Department of Radiology, University of Florida College of Medicine, 655 West 8th Street, Jacksonville, Florida 32209, USA. E-mail: dinesh.rao@jax.ufl.edu
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Lower back pain (LBP) is one of the most common chief complaints encountered in primary care. Advanced imaging studies, including computerized tomography (CT) and magnetic resonance imaging (MRI), are frequently ordered in the setting of LBP. Structural abnormalities are commonly identified by CT and MRI in patients complaining of low back pain, however, these findings are also found in asymptomatic patients. In the past decade, multiple guidelines have been published to help providers identify patients in whom the use of advanced imaging is appropriate. In this article, we review common conditions associated with LBP that require advanced imaging along with their clinical and associated imaging findings.
Keywords
Computerized tomography
low back pain
magnetic resonance imaging

INTRODUCTION
Lower back pain (LBP) affects up to 80%–85% of the population during their lifetime.[1] More than 85% of patients will have nonspecific LBP, which usually improves within a few weeks. LBP is associated with substantial direct health care costs as well as indirect costs related to disability and loss of productivity.[2] A 2014 study by Schwartz et al., estimated that annual medicare spending on imaging for uncomplicated low back pain ranged from $82 million to $226 million, which does not include costs associated with follow-up testing and care due to the results.[3] Due to the fact that the plain radiographs are insensitive for spinal pathology, magnetic resonance imaging (MRI) and computerized tomography (CT) are increasingly being utilized for low back pain, however, much of the utilization occurs outside of appropriateness guidelines.[4]
Imaging findings, such as disk degeneration, facet arthropathy, and disk herniations, have been attributed as causative factors for LBP; however, these structural abnormalities are present in a large proportion of asymptomatic individuals and the incidence of these findings increases with age.[5678]
MRI is highly sensitive in detecting degenerative changes in the spine, however, several studies have shown degenerative changes to have no association with low back pain.[91011] Perhaps, more importantly, the prognostication of surgical outcomes based on imaging findings has not been established.[1213] One study found that patients undergoing early MRI in the workup of LBP were more likely to have prolonged disability, higher medical costs, and greater utilization of surgery.[14]
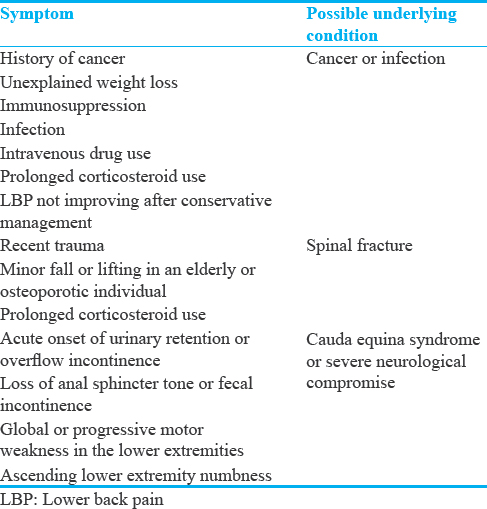
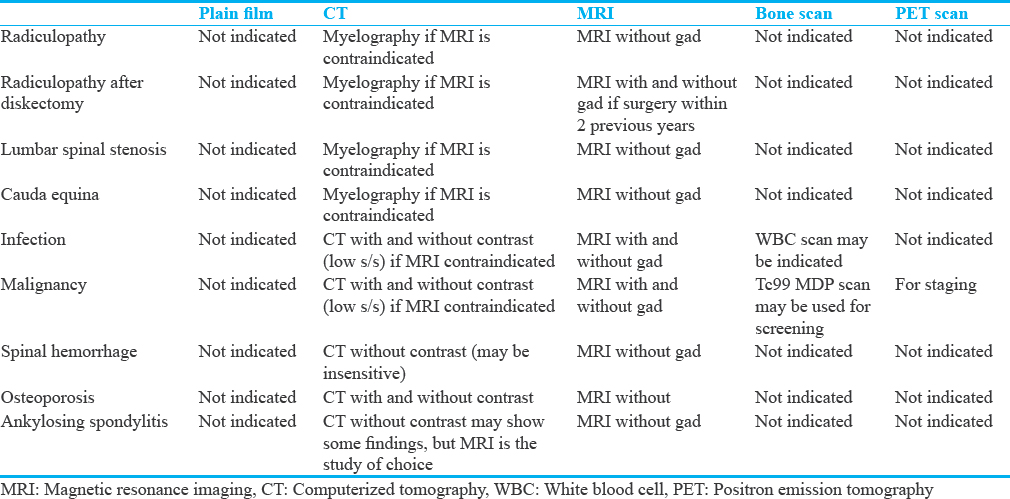
Concerns about the use of improper advanced imaging have led to the issuance of practice guidelines regarding the use of imaging in the diagnosis and treatment of LBP.[15] In 2012, the Board of Internal Medicine's Choosing Wisely campaign supported selective use MRI and CT imaging in patients with LBP.[16] The American Academy of Family Physicians recommends withholding imaging for low back pain within the first 6 weeks of symptom onset unless clinical “red flags” are present [Table 1]. The American Association of Neurological Surgeons and Congress of Neurological Surgeons recommend withholding all imaging of the spine in patients with nonspecific acute low back pain and without “red flags.” However, advanced imaging of the spine with MRI and/or CT is appropriate in several circumstances [Table 2], which will be reviewed.
RADICULOPATHY
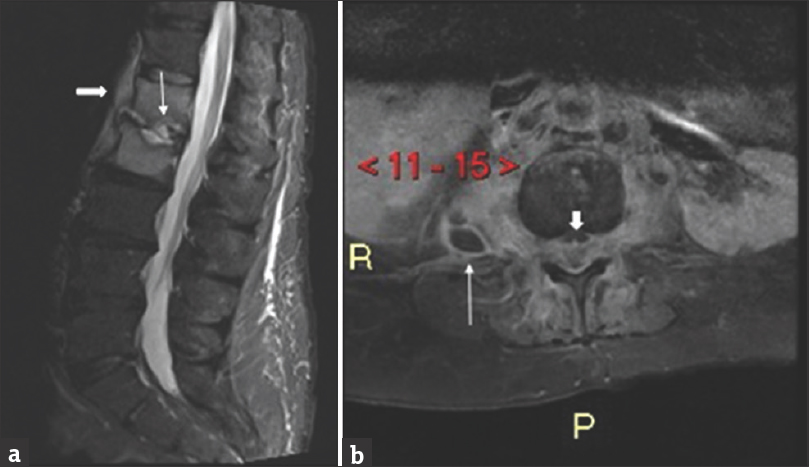
Uncomplicated LBP with or without radiculopathy is often a self-limiting benign condition in that does not warrant imaging studies in the first 4–6 weeks after symptom onset.[101718] The majority of disk herniations resorb, and patients usually become asymptomatic within 8 weeks after symptom onset.[19] Over 90% of patients with radiculopathy have symptoms in an L5 or S1 distribution.[20] MRI should be considered in patients with radiculopathy symptoms who do not responded to conservative management consisting of pain control, medical management and physical therapy after 4–6 weeks of symptom onset [Figure 1]. Alternatively, if motor weakness or muscle atrophy accompanies radiculopathy symptoms, emergent neurosurgical evaluation, and MRI should be obtained.

- A 45-year-old male who presented with low back pain radiating to the lower extremity. Sagittal T2-weighted magnetic resonance imaging of the lumbar spine demonstrates a disk herniation arising from the L3-4 level with cephalad migration posterior to the L3 vertebral body (white arrow).
RADICULOPATHY AFTER MICRODISKECTOMY
Within the first 6 months after microdiskectomy for the treatment of radiculopathy symptoms, postoperative granulation tissue can manifest clinically with recurrent or residual symptoms. Recurrent or residual disk herniations can also occur.[19] The clinical symptoms of residual or recurrent disk herniation and postoperative scarring may be identical. MRI of the lumbar spine with and without gadolinium can be useful in differentiating postoperative granulation tissue from recurrent or residual disk herniations.[212223] Granulation tissue tends to enhance homogenously, [Figure 2a] whereas herniated nucleus pulposis demonstrate peripheral enhancement [Figure 2b]. In addition, nerve roots may become damaged during surgery and enhance after gadolinium administration [Figure 2b].[24] While useful in the postoperative period, no consensus criteria have been published regarding the length of time after surgery in which administration of gadolinium is necessary. In our institution, gadolinium is used for patients who have had microdiskectomy within the past 2 years. Physicians should consult their local radiologists for recommendations on usage of gadolinium for patients who need postoperative imaging.
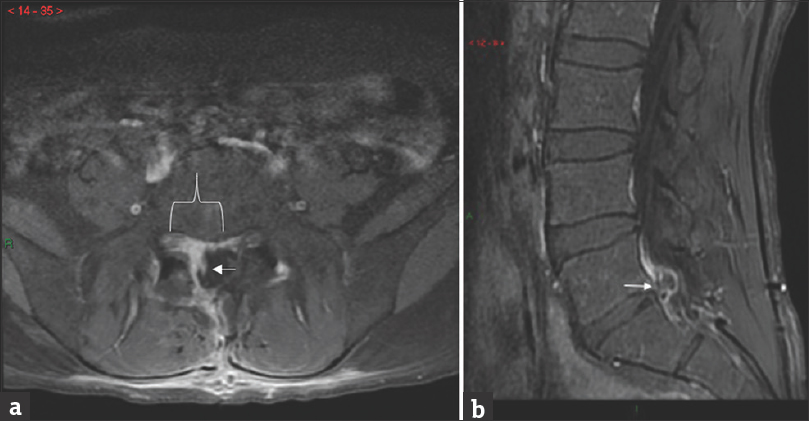
- (a) A 25-year-old male complained of worsening L1 distribution radiculopathy symptoms 1 day after microdiskectomy. Axial T1 fat saturated image of the lumbar spine with contrast demonstrates homogenously enhancing tissue in the right subarticular recess (white bracket) which represents granulation tissue. The traversing right S1 nerve root (white arrow) is enhancing and was likely injured during surgery. (b) A 32-year-old male complained of worsening right lower extremity radiculopathy symptoms for one year after previous microdiskectomy for similar radicular symptoms. A Sagittal T1 fat saturated image of the lumbar spine with contrast demonstrates a residual/recurrent disk herniation at the L5-S1 level (white arrow) resulting in residual lumbosacral radiculopathy symptoms. The disk herniation was confirmed during repeat surgery.
LUMBAR SPINAL STENOSIS
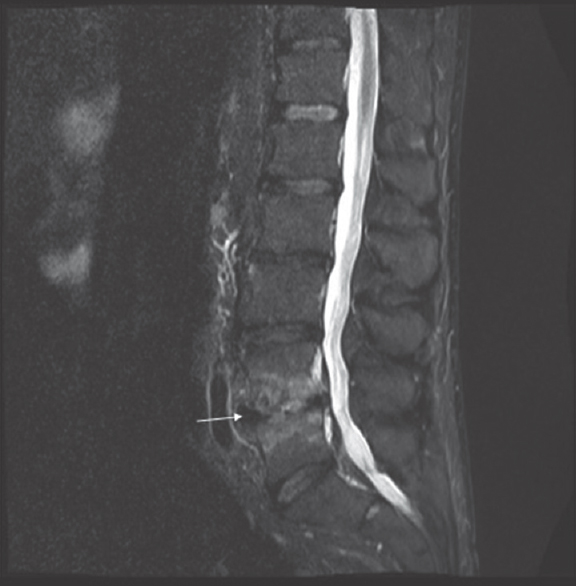
Lumbar spinal stenosis is an anatomic condition that commonly affects patients over the age of 60 years. Degenerative lumbar spinal stenosis is caused by decreased space for neural and vascular elements in the lumbar canal secondary to degenerative arthritic lumbar changes.[25] Spinal stenosis can occur as a congenital-developmental problem with diminutive caliber of the spinal canal but is usually an acquired condition due to disk bulges, herniations, facet hypertrophy, and ligamentum flavum redundancy [Figure 3]. Patients with lumbar canal stenosis can present with buttock or lower extremity pain, radiculopathy, or neurogenic claudication. Neurogenic claudication is defined as radiculopathy or pain and weakness in one or both lower extremities that worsen with walking and may be relieved with sitting or bending forward.[2627] MRI without gadolinium is considered the best imaging modality for diagnosing spinal stenosis.[272829] Specific measurements of spinal canal size on radiological imaging have not been shown to correlate with clinical symptoms of spinal canal stenosis. However, a cross-sectional area of the dural sac of <110 mm2 on MRI with can be useful in decision making for patients with clinically suspected lumbar stenosis.[25]

- A 43-year-old woman complained of progressive chronic low back pain which worsened when walking short distances. A sagittal T2-weighted image of the lumbar spine demonstrates a disk herniation at L2-3 (white arrow) resulting in severe spinal canal stenosis.
CAUDA EQUINA SYNDROME
Cauda equine syndrome (CES) results from dysfunction of the sacral and lumbar nerve roots resulting in motor impairment of the bladder, bowel, sexual function, and perineal numbness. The patients can present with low back pain with or without radiculopathy, lower extremity weakness or sensory changes, or absent reflexes. The most common symptom of CES is low back pain.[30] A prospective cohort study by Bell et al., recommends urgent unenhanced lumbar MRI in all patients with new-onset urinary symptoms with low back pain or sciatica.[31] The most common cause of CES is lumbar disc herniation at the L4-5 or L5-S1 levels, but can also occur secondary to trauma, metastatic disease or spinal hemorrhage [Figure 4]. In patients who are unable to undergo MRI, myelography can be used as an alternative.[18]
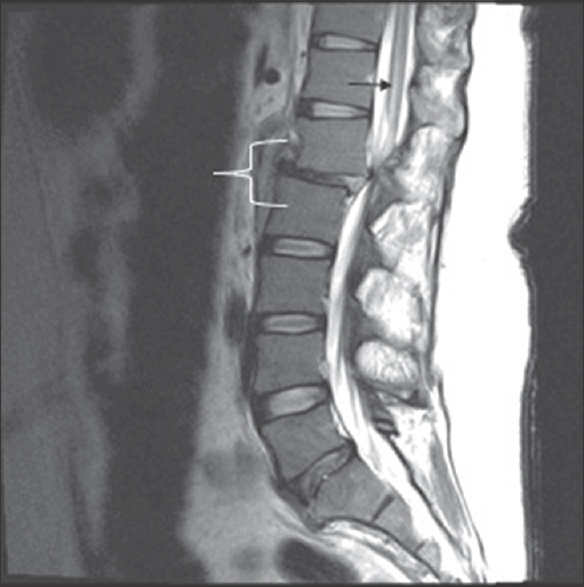
- A 24-year-old male presented with bilateral lower extremity paralysis and loss of sensation after a motor vehicle collision. A sagittal T2-weighted image demonstrates traumatic retrolisthesis of L1 on L2 (white bracket) resulting in severe canal stenosis. Note the hyperintense T2 signal in the spinal cord which represents a spinal cord infarction (black arrow).
INFECTION
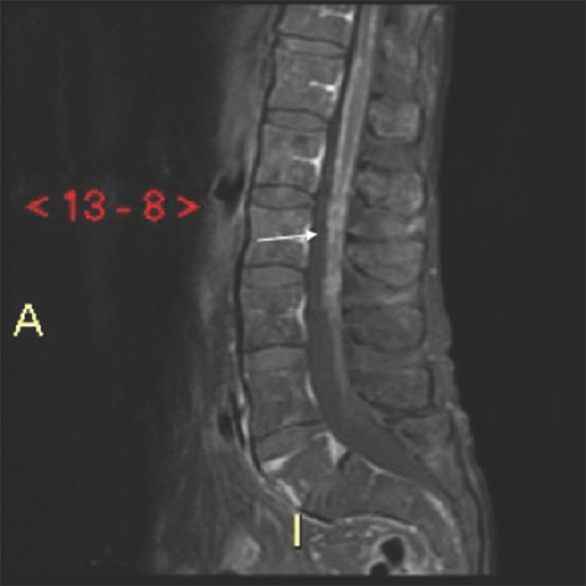
Spinal infection is usually secondary to a primary source elsewhere in the body. Infection can spread to the spine hematogenously through direct adjacent infection as a complication of recent surgery or spinal procedure, intravenous drug use, or penetrating trauma. Symptoms of spinal infection are nonspecific. Patients often complain of low back pain that is not relieved with analgesics. Fever is not consistently present. Constitutional symptoms such as chills, night sweats, and weight loss may not be consistently present, but raise suspicion for infection when present.[32] White blood cell count may be normal, while erythrocyte sedimentation rate and C-reactive protein are usually, but not always, elevated.[3233] The lumbar spine is most commonly affected, followed by the thoracic spine and the cervical spine.[34] Pyogenic discitis osteomyelitis most commonly involves one lumbar segment, beginning in the anterior portion of the endplates of adjacent vertebral bodies and the intervertebral disk. MRI with and without gadolinium is the preferred imaging study to diagnose and localize spinal infection because of its high sensitivity and specificity.[3435363738] T1-weighted images display low signal intensity along the endplate with loss of definition of the cortex with corresponding high signal intensity of T2 and short tau inversion recovery (STIR) images [Figure 5a]. The disk space usually demonstrates fluid like signal intensity on all pulse sequences.[36] Epidural and paraspinal abscess develops later in disease course and are characterized by peripheral enhancing fluid collections on MRI [Figure 5b].
- (a) A 42-year-old male with a history of intravenous drug use presented with fever and low back pain. A sagittal short tau inversion recovery magnetic resonance imaging of the lumbar spine demonstrates edema-like signal in the L1 and L2 vertebral bodies with fluid signal within the intervertebral disk space and endplate destruction (thin arrow). Note the paraspinal phlegmon (thick white arrow). (b) A 43-year-old female presented with fever, severe low back pain, and bilateral lower extremity weakness. Axial T1 fat, saturated magnetic resonance imaging with gadolinium of the lumbar spine demonstrates a paraspanal abscess (thin white arrow) as well as epidural phlegmon and abscess (short, thick white arrow) in the lumbar spine.
Modic Type 1 degenerative changes can mimic early discitis osteomyelitis. Type 1 degenerative change is defined edema such as signal on fluid-sensitive sequences with enhancement of the vertebral body endplates and disk [Figure 6]. However, these imaging features can occur both in Type 1 changes and discitis osteomyelitis. Aggressive imaging features such as endplate destruction can also occur in both scenarios. If the fluid signal in the disk or soft tissue or epidural abscess are present, infectious etiology rather than Type 1 degenerative changes should be favored.[39] Correlation with the patient history for risk factors, spinal infection, and us of inflammatory markers is essential in differentiating imaging findings in infection from Modic 1 changes. Serial follow-up MRI examinations may be useful in distinguishing the infection from degenerative changes and monitoring therapeutic responses.
- A 50-year-old male presented with chronic low back pain. Modic Type 1 endplate changes characterized by hyperintense signal (white arrow) on a sagittal short tau inversion recovery image of the lumbar spine.
Atypical infections, such as tuberculosis and fungal infections, have a different appearance on imaging than most typical bacterial infections. Mycobacterial and fungal pathogens frequently involve the vertebral bodies, but initially spare the intervertebral disks. This type of infection spreads beneath the anterior and posterior longitudinal ligaments leaving intervertebral disks unaffected until late in the disease course [Figure 7].[40]

- A 30-year-old male presented with fever, night sweats, weight loss, and severe low back pain. A fat, saturated T1 enhanced magnetic resonance imaging of the lumbar spine demonstrates enhancement of the L4 and L5 endplates (white bracket) with subligamentous enhancement posteriorly (white arrow). There is also enhancement of the L3 inferior endplate. Biopsy cultures revealed atypical mycobacterial infection.
MALIGNANCY
Although a history of malignancy is the strongest risk factor for pain from bone metastasis, <1% of patients in a primary care center have malignancy as the etiology for low back pain.[41] Other risk factors such as insidious onset, age >50, and failure to improve with conservative management have high false positive rates. Among solid cancers, metastatic disease to the spine is most commonly from breast, prostate, lung, thyroid, and renal cancers. Around 60% of patients with multiple myeloma present with skeletal lytic lesions.
The osseous spinal metastatic disease most often occurs with pain, and a specific complaint of sudden severe pain should raise concern for pathologic fracture. The spine is the third most common site for metastatic disease to manifest and is the most common site for the osseous metastatic disease.[4243] Osseous metastasis most frequently involves the thoracic spine. Metastatic lesions can occur within the bone, the epidural space, the intradural extramedullary space (i.e., leptomeningeal carcinomatosis), or intramedullary (within the parenchyma of the spinal cord).
Spinal X-ray is relatively insensitive for the detection of bone metastases to the spine, with false negative results approaching 40%.[44]
Nuclear medicine bone scans are the standard for initial screening for skeletal metastasis, but the results should be correlated with CT or MRI scans because of a lack of specificity.[45] FDG-PET scans detect increased glucose metabolism, when combined with CT have a reported sensitivity of 74% and 98% respectively.[46]
CT provides excellent spatial resolution and can demonstrate sclerotic or lytic changes in the marrow space or cortex, however MRI with and without gadolinium is significantly superior to CT for detection of osseous metastases with higher sensitivity and similar specificity.[46] MRI is also superior for tumor characterization, allowing evaluation of both bone and soft tissue components that may involve the spinal cord and nerve roots [Figure 8]. The combination of T1 hypointensity and STIR hyperintensity has been shown to be the most useful in the detection of metastatic lesions and in discrimination of malignant from benign bone changes. The MRI appearance of metastatic lesions depends on the nature of the bone replacement or destruction. Lytic lesions are typically hypointense on T1-weighted images and exhibit diffuse enhancement. Blastic metastatic lesions are typically hypointense on T1 and T2-weighted pulse sequences. Mixed lytic and sclerotic lesions will have features of both.[46]
- A 59-year-old male presented with progressive bilateral lower extremity weakness, cough, and malaise Sagittal T1 fat, saturated magnetic resonance imaging of the lumbar spine demonstrates thin micronodular enhancement of the surface of the spinal cord. Further patient workup revealed metastatic lung cancer.
SPINAL HEMORRHAGE
Spinal hematomas should be considered in patients with signs of acute or progressive paraparesis, paresthesia or bowel, and bladder incontinence.[47] Intraspinal hematomas can occur in the setting of trauma or recent procedure, secondary to anticoagulation, or can occur spontaneously. MRI without gadolinium is considered the study of choice for diagnosis for diagnosis.[4849] Intraspinal hematomas can occur in the epidural space (epidural hematomas [EDH]) [Figure 9], subdural space (subdural hematomas [SDH]), subarachnoid space or within the spinal cord. The location of intraspinal hematoma can be determined by the location of signal changes and the effect of the hematoma on adjacent structures. SDH are classified if blood products do not displace epidural fatty tissue. EDH can be suspected if epidural fat is displaced, and if there is displacement of the dura toward the spinal canal. A subarachnoid hemorrhage will be in an extramedullary intradural location.[50]

- A 68-year-old male presented with severe low back pain and altered bilateral lower extremity sensation after falling down. He was taking Plavix for a coronary stent. A sagittal T1 weighted magnetic resonance imaging of the lumbar spine demonstrates an anterior epidural hematoma from T12 through L5 (black arrow).
OSTEOPOROSIS
Vertebral fractures secondary to osteoporosis are common, affecting 30 million American women and 14 million American men.[51] Vertebral fractures are associated with lower quality of life. Risk factors for osteoporotic fractures include increasing age, female gender, and steroid use. In a large study in Europe, the prevalence of osteoporotic fractures ranged from 10% to 24%.[52] Many vertebral fractures are asymptomatic; however, even asymptomatic fractures can have significant consequences because of the increased risk of future fractures.[535455] Vertebral fractures may present with spinal pain that is worse with walking or standing and relieved by lying flat but are difficult to diagnose due to the nonspecific nature of such symptoms. Only one in four vertebral fractures is clinically recognized.[56] When there is concern for osteoporotic fracture, noncontrast CT is recommended [Figure 10].[18]

- A 53-year-old male presented with severe low back pain. He was taking oral steroids. He denied trauma. An unenhanced sagittal computerized tomography image of the lumbar spine demonstrates a compression fracture of the L5 vertebral body with vertebra plana and retropulsion of bone into the spinal canal (white arrow).
ANKYLOSING SPONDYLITIS
Ankylosing spondylitis (AS) most commonly occurs in men under the age of 40 who present with back pain and morning stiffness that improves with exercise. Systemic disease manifestations such as uveitis and iritis may also be present. No comprehensive studies have been conducted regarding the use of MRI in the management of inflammatory spondyloarthropathies.[57] Plain radiography is used routinely for the initial evaluation of patients with AS, while MRI is used for subsequent evaluations.[575859] MRI can show signal changes at the corners of the vertebral bodies, known as Romanus lesions or “shiny corners.” [Figure 11]. Sacroiliitis can also be seen on MRI and CT and can be an isolated cause of LBP. MRI has a sensitivity of 25%–85% with a specificity of 90%–100% for the evaluation of AS.[484951] MRI has also been used to assess treatment response with anti-TNF factor therapy in patients with AS.[57]
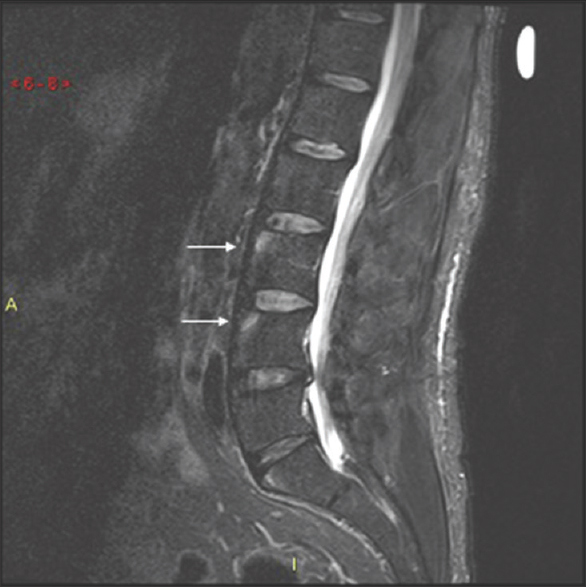
- A 28-year-old male was imaged because of progressive worsening low back pain. A Sagittal short tau inversion recovery magnetic resonance imaging of the lumbar spine demonstrates Romanus lesions, also known as “shiny corners” at the anterior superior endplates of L3 and L4 (white arrows). Further workup revealed a diagnosis of ankylosing spondylitis.
SUMMARY
Routine acute LBP is usually a benign, self-limiting condition that does not warrant evaluation with any imaging modality. Advanced imaging modalities such as CT and MRI can provide useful clinical information if used correctly in patients with radiculopathy that unresponsive to conservative management, myelopathy, neurogenic claudication, or patients with “red flag” symptoms. A thorough history and physical exam is essential to identifying patients who would most benefit from advanced imaging. Plain films are insensitive to many pathologies. Noncontrast CT is the initial study of choice if a fracture of the spine is suspected. MRI is the gold standard diagnostic imaging modality for many disease states associated with LBP, with use of intravenous gadolinium contrast reserved for patients in whom infection, malignancy, or postoperative sequelae are suspected. In patients who cannot safely undergo MRI, CT with or without myelography can be considered as a less sensitive alternative diagnostic imaging tool.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/30/239701
REFERENCES
- Cost, controversy, crisis: Low back pain and the health of the public. Annu Rev Public Health. 1991;12:141-56.
- [Google Scholar]
- Increased costs and rates of use in the California workers' compensation system as a result of self-referral by physicians. N Engl J Med. 1992;327:1502-6.
- [Google Scholar]
- Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36:811-6.
- [Google Scholar]
- Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:403-8.
- [Google Scholar]
- Computed tomography-evaluated features of spinal degeneration: Prevalence, intercorrelation, and association with self-reported low back pain. Spine J. 2010;10:200-8.
- [Google Scholar]
- A study of computer-assisted tomography. I. The incidence of positive CAT scans in an asymptomatic group of patients. Spine (Phila Pa 1976). 1984;9:549-51.
- [Google Scholar]
- Imaging of degenerative spine disease – The state of the art. Adv Clin Exp Med. 2012;21:133-42.
- [Google Scholar]
- Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology. 2005;237:597-604.
- [Google Scholar]
- Imaging strategies for low-back pain: Systematic review and meta-analysis. Lancet. 2009;373:463-72.
- [Google Scholar]
- Percent spinal canal compromise on MRI utilized for predicting the need for surgical treatment in single-level lumbar intervertebral disc herniation. Spine J. 2005;5:608-14.
- [Google Scholar]
- Magnetic resonance imaging predictors of surgical outcome in patients with lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 2013;38:1216-25.
- [Google Scholar]
- Relationship of early magnetic resonance imaging for work-related acute low back pain with disability and medical utilization outcomes. J Occup Environ Med. 2010;52:900-7.
- [Google Scholar]
- Diagnostic imaging for low back pain: Advice for high-value health care from the American college of physicians. Ann Intern Med. 2011;154:181-9.
- [Google Scholar]
- Rapid magnetic resonance imaging vs. radiographs for patients with low back pain: A randomized controlled trial. JAMA. 2003;289:2810-8.
- [Google Scholar]
- Determinants of spontaneous resorption of intervertebral disc herniations. Spine (Phila Pa 1976). 2006;31:1247-52.
- [Google Scholar]
- Acute low back problems in adults: Assessment and treatment. Agency for health care policy and research. Clin Pract Guidel Quick Ref Guide Clin. 1994;384:iii-iv.
- [Google Scholar]
- The postoperative lumbar spine: Imaging considerations. Semin Ultrasound CT MR. 1993;14:425-36.
- [Google Scholar]
- The postoperative lumbar spine. A radiological investigation of the lumbar spine after discectomy using MR imaging and CT. Acta Radiol Suppl. 1998;414:1-23.
- [Google Scholar]
- Symptomatic nerve root changes on contrast-enhanced MR imaging after surgery for lumbar disk herniation. AJNR Am J Neuroradiol. 2009;30:1062-7.
- [Google Scholar]
- An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update) Spine J. 2013;13:734-43.
- [Google Scholar]
- Variation in eligibility criteria from studies of radiculopathy due to a herniated disc and of neurogenic claudication due to lumbar spinal stenosis: A structured literature review. Spine (Phila Pa 1976). 2010;35:803-11.
- [Google Scholar]
- Diagnosis of lumbar spinal stenosis: A systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976). 2006;31:1168-76.
- [Google Scholar]
- Lumbar spinal stenosis assessment with computed tomography, magnetic resonance imaging, and myelography. Clin Orthop Relat Res. 2001;384:122-36.
- [Google Scholar]
- Does patient history and physical examination predict MRI proven cauda equina syndrome? Evid Based Spine Care J. 2011;2:27-33.
- [Google Scholar]
- Cauda equina syndrome: What is the correlation between clinical assessment and MRI scanning? Br J Neurosurg. 2007;21:201-3.
- [Google Scholar]
- MR imaging assessment of the spine: Infection or an imitation? Radiographics. 2009;29:599-612.
- [Google Scholar]
- Magnetic resonance imaging of spinal infections. Top Magn Reson Imaging. 1994;6:69-81.
- [Google Scholar]
- Imaging of pyogenic infectious spondylodiskitis. Radiol Clin North Am. 2001;39:203-13.
- [Google Scholar]
- Imaging of musculoskeletal and spinal tuberculosis. Radiol Clin North Am. 2001;39:329-42.
- [Google Scholar]
- MR imaging findings in spinal infections: Rules or myths? Radiology. 2003;228:506-14.
- [Google Scholar]
- MR appearances of the temporal evolution and resolution of infectious spondylitis. AJR Am J Roentgenol. 1996;166:903-7.
- [Google Scholar]
- Cancer as a cause of back pain: Frequency, clinical presentation, and diagnostic strategies. J Gen Intern Med. 1988;3:230-8.
- [Google Scholar]
- Surgery insight: Current management of epidural spinal cord compression from metastatic spine disease. Nat Clin Pract Neurol. 2006;2:87-94.
- [Google Scholar]
- The role of plain radiographs in management of bone metastases. J Palliat Med. 2009;12:195-8.
- [Google Scholar]
- Detection of osseous metastases of the spine: Comparison of high resolution multi-detector-CT with MRI. Eur J Radiol. 2009;69:567-73.
- [Google Scholar]
- Spinal epidural hematoma with spontaneous recovery demonstrated by magnetic resonance imaging. Spine (Phila Pa 1976). 1994;19:483-6.
- [Google Scholar]
- Acute spinal subdural hematoma: MR and CT findings with pathologic correlates. AJNR Am J Neuroradiol. 1994;15:1895-905.
- [Google Scholar]
- MRI findings in spinal subdural and epidural hematomas. Eur J Radiol. 2007;64:119-25.
- [Google Scholar]
- America's Bone Health: The State of Osteoporosis and Low Bone Mass in Our Nation. Washington DC: National Osteoporsis Foundation; 2002.
- The prevalence of vertebral deformity in European men and women: The European vertebral osteoporosis study. J Bone Miner Res. 1996;11:1010-8.
- [Google Scholar]
- Patients with prior fractures have an increased risk of future fractures: A summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721-39.
- [Google Scholar]
- Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of osteoporotic fractures research group. J Bone Miner Res. 1999;14:821-8.
- [Google Scholar]
- Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285:320-3.
- [Google Scholar]
- Imaging of seronegative spondyloarthritis. Best Pract Res Clin Rheumatol. 2008;22:1045-59.
- [Google Scholar]
- Evaluation of the diagnostic utility of spinal magnetic resonance imaging in axial spondylarthritis. Arthritis Rheum. 2009;60:1331-41.
- [Google Scholar]
- Comparison of bone scan, computed tomography, and magnetic resonance imaging in the diagnosis of active sacroiliitis. Semin Arthritis Rheum. 1993;23:161-76.
- [Google Scholar]






