Translate this page into:
A novel dual balloon rectal catheter for use in the postoperative assessment of low rectal anastomoses following low anterior resection

-
Received: ,
Accepted: ,
How to cite this article: Mercer M, Kocher M, Shaheen N, Flemming BP, Waltz J. A novel dual balloon rectal catheter for use in the postoperative assessment of low rectal anastomoses following low anterior resection. J Clin Imaging Sci 2022;12:18.
Abstract
Following low anterior resection (LAR) of the colon, an image-guided assessment of the anastomosis for leak is typically performed using an enema via a rectal catheter, whether by CT or fluoroscopy. However, there is potential for poor assessment due to inappropriate catheter positioning as well as potential risk that the anastomosis becomes compromised by the balloon inflation. This article discusses the adaptation of a novel double-balloon catheter (originally designed by a member of our institution for use in pediatric intussusception reduction) for assessment of low rectal anastomoses. The goal of this technical note is to demonstrate our experience with this catheter, primarily through example cases, and explain its potential for optimizing colon distension, minimizing improper catheter placement, and potentially reducing the risk of iatrogenic anastomosis disruption.
Keywords
Low anterior resection
Computed tomography
Rectal anastomosis
Rectal contrast
Rectal catheter
INTRODUCTION
The integrity of the low rectal anastomosis following low anterior resection (LAR) surgery (often due to colon cancer) can be assessed by fluoroscopy or CT using rectal contrast material administration via enema.[1] This assessment requires the insertion of a rectal catheter to introduce the contrast material. Traditionally, a single balloon catheter (commonly a Foley catheter) is used and reverse pressure is applied by the operator to achieve a seal and prevent leakage of the contrast material. While this can be achieved manually during fluoroscopy examinations, it is more difficult to maintain during CT examinations, as the user must release their physical hold on the catheter to obtain the images. Adhesive tape can be used in lieu of manual pressure with varying degrees of success in our personal experience. As such, there is a clinical need for a catheter design that can maintain an effective rectal seal without “hands-on” manipulation, especially for rectal contrast used for CT.
Postoperative imaging following colorectal surgery for anastomotic disruption is nearly ubiquitous. Accurate, early identification of colonic anastomotic leak is correlated to improved patient outcomes[2] and leak is associated with up to 50% serious morbidity without effective treatment.[3] In fact, low anterior colorectal resection has the highest rate of anastomotic leak among colorectal surgeries.[4]
Whether by CT or fluoroscopy, the integrity of a low anterior anastomosis can be difficult to assess, primarily as the requisite balloon is in close proximity to the anastomosis [2] Although real-time visualization is an advantage of fluoroscopy for catheter placement, CT has advantages over fluoroscopy in anatomic visualization. However, peri-anastomotic air, a finding readily seen on CT, is commonly present in the early postoperative abdomen making this finding of questionable diagnostic value without contrast material installation. On rectal enema CT, the combination of peri-anastomotic air and extra-luminal contrast material markedly increases confidence in the diagnosis of an anastomotic leak, making CT a valuable imaging tool.[5]
A significant technical pitfall of CT in the evaluation for an anastomotic leak is incontinence of the rectal contrast agent, which is often related to an inability to achieve and maintain optimal balloon catheter position [6] Further, the location of the balloon inflation is essential, as it must be below, not at or above, the anastomosis for the contrast agent to be able to identify a leaking anastomosis. This technical note will demonstrate through case examples some of the potential limitations of rectal enema CT for assessment of low rectal anastomoses and the potential for improved assessment with a double balloon rather than a single balloon catheter.
METHODS AND CLINICAL RESULTS WITH USAGE OF DOUBLE BALLOON CATHETER
Historically at our institution, rectal enema for assessment of anastomotic leak following LAR was performed with a single balloon catheter commonly referred to as a “Foley” catheter. Additionally, both radiologists and the requesting surgeons have increasingly favored CT in this assessment for its improved visualization of the operative region. However, our radiology group identified a significant number of CT enema examinations that were suboptimal using the Foley catheter. Most commonly, cases were identified which had sub-optimal opacification and incomplete colonic distension [Figure 1]. One of the causes suggested by the technologists was due to the fact that they were unable to manually hold the catheter in place while the CT scan was being performed. Additionally, cases in which the location of the inflated balloon was incorrect in relation to the anastomosis were identified, in some cases rendering the study non-diagnostic [Figure 2]. There was also concern expressed by radiologists that such incorrect placement could potentially compromise the healing anastomosis, thus potentially causing a leak that was not previously present.

- A57-year-old male who presented for assessment of anastomotic dehiscence. Sagittal reconstruction of a CT with water soluble rectal contrast using a traditional (single balloon) rectal catheter. There was incomplete distension of the colon with contrast material leaking around the tube due to inadequate seal and incontinence.

- A 74-year-old male who underwent recent LAR. Coronal and sagittal reconstructions demonstrate a single balloon catheter inflated above the anastomosis (white arrow). Despite extra-luminal gas surrounding the anastomosis, the rectal contrast material is not in the appropriate location to assess for the anastomotic leak.
To address these issues, it was decided to change our routine clinical practice. Our group was familiar with a novel double balloon catheter that was already being used clinically in the pediatric division at our institution. This novel dual balloon catheter (originally designed for air enema reduction of ileocolic intussusception)[7] was already FDA approved for general rectal use in adults and children, therefore it was accepted for clinical use by our division. It is important to note that this catheter was designed and is solely owned by an employee of the Department of Radiology at the Medical University of South Carolina. However, the decision for the clinical use of this catheter was based on the clinical discretion of physicians who were not involved in the design or development of this catheter. Further, individuals with no ownership stake in the company undertook this manuscript as an independent endeavor. Additionally, this catheter has not been marketed for use in patients being evaluated for anastomosis breakdown following low anterior resection of the colon.
For background, the instructions which were given to the technologists for its clinical use will be reviewed [Table 1]. First, the catheter, without any balloons inflated, is passed carefully through the anus into the rectal vault [Figure 3a]. Next, the distal balloon is inflated and retracted lightly until seated at the anorectal junction [Figure 3b]. Finally, the proximal balloon is inflated in order to secure the catheter in place. Additionally, the shape of the proximal balloon, which is conical when inflated, applies retrograde pressure [Figure 3c]. Once contrast material is instilled via enema, the rectal seal is maintained by the two balloons (not by technologist’s hands) to prevent incontinence [Figure 4].
| 1. Check function of both balloons to ensure proper inflation and no leakage from the catheter or balloons. |
| 2. Aspirate all air from balloons and ensure they are completely deflated. |
| 3. Lubricate the catheter tip before insertion. |
| 4. Warn patient and insert catheter at least 6 inches. |
| 5. Inflate distal (internal) balloon with no more than 50 cc of air. Retract until resistance is felt. OPTIONAL: If there is a possible low anastomosis, distal balloon can remain deflated and proceed to step 6. |
| 6. Inflate proximal (external) balloon with no more than 70 cc of air. |
| 7. Proceed with contrast administration. |
| 8. After exam completion completely deflate distal (internal) balloon followed by proximal (external) balloon. |
| 9. Carefully remove catheter and dispose. |
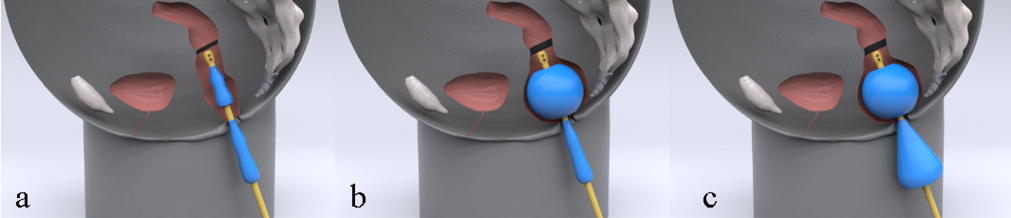
- (a) Diagram of enema tip inserted into rectum prior to balloon inflation located below the anastomosis (black line) but above the anorectal junction. (b) Diagram of enema tip inserted into rectum following inflation of the distal balloon, still located below the anastomosis (black line) but above the anorectal junction. (c) Diagram of enema tip in rectum following inflation of the second (proximal) conical shaped balloon below the anorectal junction.

- Sagittal reconstruction of a rectal enema CT using the dual balloon catheter to fill the colon with both proximal (white arrow) and distal (outline arrow) balloons inflated.
RESULTS AND DISCUSSION
Our experience has not been without some technical errors. The most common error encountered was the failure to pass the catheter (prior to balloon inflation) far enough into the rectum at initial insertion. When the balloons are subsequently inflated, the balloons did not capture the anorectal junction between them [Figure 5a]. However, when this occurs the examination has still been diagnostic. We theorize that the reason for a maintained rectal seal despite inadequate technique is that the conical shape of the proximal balloon is often adequate to maintain the seal [Figure 5b]. In fact, when evaluating the anastomosis following LAR, we specifically ask the CT technologists to only use the proximal balloon. We have seen excellent results with the technique with very few nondiagnostic exams. Our institution uses the dual balloon rectal catheter for essentially all of the LAR rectal anastomosis assessments. While we do not have specific numbers as to how many we have used, it is now built into the protocol to be used in every LAR rectal anastomosis assessment.

- (a) Sagittal reconstruction of a rectal enema CT using the dual balloon catheter however the distal balloon has been inflated BELOW the anorectal junction (arrow). Note the quality of the colonic distention remains diagnostic. (b) Sagittal reconstruction of a rectal enema CT using the dual balloon catheter, however the distal balloon has not been inflated. The conical shaped proximal balloon has been inflated with the degree of colonic distention remaining diagnostic.
We believe this catheter has other potential uses in the radiology department such as conventional fluoroscopic enemas. We also think that it has the potential to improve CT colonography given its superior seal and potential for increased colonic distention, although we have not yet started using the catheter for this purpose in our division.
CONCLUSION
This article has presented insights from a single institution experience by using a novel double balloon catheter for evaluation of low rectal anastomosis following colon surgery. Potential advantages of this catheter over single balloon catheters include: (a) Improved accuracy in catheter placement and balloon location in relation to the anastomosis, (b) Decreased need to manually secure the catheter in place, and (c) Consistently high quality colon insufflation (filling) leading to optimal characterization of the anastomosis for the leak. Routine clinical use of such a dual balloon catheter should be considered when evaluating low rectal anastomoses.
Declaration of patient consent
Patient’s consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Anastomotic leaks after low anterior resection for rectal carcinoma: evaluation with CT and barium enema. AJR Am J Roentgenol. 1995;165:567-71.
- [CrossRef] [PubMed] [Google Scholar]
- Multidetector CT of the postoperative colon: review of normal appearances and common complications. Radiographics. 2013;33:515-32.
- [CrossRef] [PubMed] [Google Scholar]
- Anastomotic leakage after anterior resection for rectal cancer: Risk factors. Colorectal Dis. 2010;12:37-43.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of multidetector CT in detecting anastomotic leaks following stapled left-sided colonic anastomosis. Clin Radiol. 2014;69:59-62.
- [CrossRef] [PubMed] [Google Scholar]
- Early postoperative imaging after non-bariatric gastric resection: A primer for radiologists. Insights Imaging. 2017;8:393-404.
- [CrossRef] [PubMed] [Google Scholar]
- Successful reduction of recalcitrant ileocolic intussusception with a double-balloon-tipped catheter that prevents air leaks and catheter expulsion. Radiol Case Rep. 2021;16:3341-5.
- [CrossRef] [PubMed] [Google Scholar]






