Translate this page into:
Timely Identification of Pregnancy in Noncommunicating Horn of Unicornuate Uterus by Three-Dimensional Transvaginal Ultrasonography
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pregnancy in the rudimentary horn of a unicornuate uterus is uncommon and needs to be diagnosed at early stages to avoid uterine rupture to avert the high morbidity and mortality. In this case report, we discussed the advantage of three-dimensional transvaginal ultrasonography (3D TV-USG) in assessing the early pregnancy in the noncommunicating rudimentary horn of uterus. A 23-year-old woman approached us for routine pregnancy scan. The location of 5-week pregnancy was confirmed in the right noncommunicating horn of a unicornuate uterus by 3D TV-USG. She has undergone laparohysteroscopy, and excision of a gravid rudimentary horn was done. After an interval of 6 months, the patient received fertility treatment and conceived consequently. Although magnetic resonance imaging (MRI) is an excellent way of diagnosing uterine anomalies, the procedure is expensive, time-consuming, and not widely available. 3D USG is less expensive and more readily accessible for early diagnosis of uterine anomalies, particularly in health-care centers where MRI is not readily available or affordable.
Keywords
Gestational sac
laparohysteroscopy
three-dimensional ultrasound
transvaginal
unicornuate uterus

INTRODUCTION
When there is nonfusion of the mullerian ducts during development associated with the normal maturation of one and partial development of the contralateral duct, it results in a unicornuate uterus associated with a rudimentary noncommunicating horn.[1] A unicornuate uterus with a noncommunicating cavitated horn is classified as Class IIB according to the American Fertility Society and U4a according to the European Society of Human Reproduction and Embryology/European Society for Gynaecological Endoscopy classification of uterine anomalies.[2]
After the study of 366 rudimentary horn presentations, it was observed that 92% were noncommunicating horns presenting usually with imminent rupture or a ruptured uterus.[3]
Pregnancy in a unicornuate uterus with the noncommunicating horn is extremely rare with the frequency of 1/100,000–140,000.[45] Timely diagnosis of this condition is challenging. and could be overlooked, especially if the patient has no symptoms. It could also be misdiagnosed as a cornual or isthmic pregnancy.[6] In this report, we present the advantages of three-dimensional ultrasonography (3D USG) in the diagnosis of an early pregnancy in the noncommunicating horn of a unicornuate uterus. By diagnosing the anomaly in early pregnancy, it is possible to prevent complications such as uterine rupture, unnecessary induction of labor, and fetal death at a later gestation.[7]
CASE REPORT
A 23-year-old woman approached our clinic with 1½ months of amenorrhea and a positive urine pregnancy test. A two-dimensional ultrasound (Voluson™ E10, GE Healthcare, Austria GmbH and Co OG) with the endovaginal probe (GE-RIC5-9-D) disclosed an intrauterine sac with the presence of yolk sac and fetal pole with gestational age of 5 weeks [Figure 1]. Fetal cardiac activity was not seen. During the normal ultrasound evaluation protocol of the institute, while following the cervical canal upward into the uterine cavity, a normal uterine cavity with a thick endometrium without a gestational sac was identified. On further assessment and for better evaluation, a 3D ultrasound was performed identifying the location of the pregnancy to be in the noncommunicating horn of a unicornuate uterus. Beside the noncommunicating horn, a corpus luteum cyst in the right ovary was observed [Figure 2]. No other additional pathologies were identified. A diagnosis of unicornuate uterus with a 5-week gestational sac in the right noncommunicating horn was thus confirmed. We further evaluated the connection between the unicornuate uterus and the rudimentary horn. Using a Doppler assessment of the connection, we could predict that it was a thick fibrous band with minimal vascularity and hence minimal blood loss would be expected during surgery. As expectant management is not an option, the patient was counseled for excision of the gravid noncommunicating horn. A hystero-laparoscopy revealed normal peritoneal cavity with free fluid in the Pouch of Douglas (POD), a unicornuate uterus with a distended right rudimentary horn with the pregnancy, normal fallopian tubes, and a corpus luteum in the right ovary [Figure 3]. On hysteroscopy, we could observe a normal fundus, left ostia, and thick endometrium. The right ostium was not observed. Excision of the pregnant gravid horn of the uterus was done along with ipsilateral salpingectomy. The specimen was retrieved vaginally through colpotomy. The patient was discharged 2 days after the procedure. She conceived after ovulation induction and now has a 11-week healthy intrauterine pregnancy.
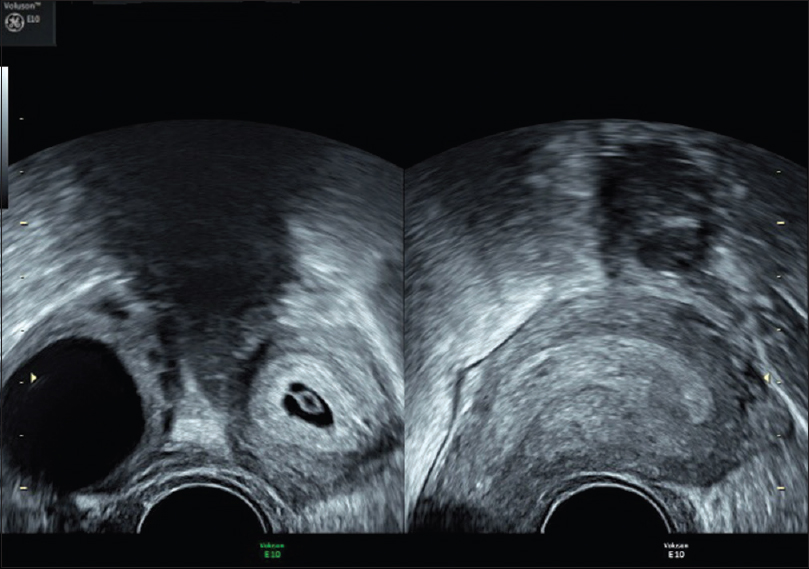
- A 23-year-old woman approached us with 1½ months of amenorrhea and a positive urine pregnancy test. A transvaginal two-dimensional image showed the presence of intrauterine gestational sac in the right horn with yolk sac and a corpus luteum cyst in the ipsilateral ovary. A nonpregnant horn on the left side was observed. Nonpregnant horn shows the typical shape of the uterus with extreme lateral flexion.

- Three-dimensional ultrasound in coronal view clearly demonstrates unicornuate uterus on the left side and presence of pregnancy in the right horn. Myometrium surrounding the gestational sac with no thinning and no communication between the two horns. There is no continuity between the cavities containing the gestational cavity with the cervical canal.

- Laparoscopic picture showing left unicornuate uterus and an unruptured right rudimentary horn pregnancy with attached tube and ovary. Globular shape of the pregnant form can be made out with wide separation and no communication between the cavities.
DISCUSSION
Pregnancy in a noncommunicating rudimentary horn occurs as a result of transperitoneal migration of the sperm to fertilize an oocyte in the fallopian tube of the rudimentary horn or implantation of a zygote that was formed in the POD and was transported into the rudimentary horn.[8] In our case, as the corpus luteum is on the side of the horn, it appears that sperm migrated through the fallopian tube of the unicornuate uterus into the peritoneal cavity to fertilize the oocyte in the fallopian tube of the rudimentary horn. Subsequently, the formed zygote implanted in the rudimentary horn.[6]
Diagnosis of a rudimentary horn pregnancy can be easily missed if not looked for. In the case presented here, if further evaluation to see the continuation of the uterine cavity with the cervix was not assessed, the rudimentary horn would go unnoticed and it would have been wrongly diagnosed as a normal intrauterine pregnancy. Due to the enlarging horn and thinning myometrium, misdiagnosis of a bicornuate uterus, interstitial pregnancy, and abdominal pregnancy is possible.[3] Hence, we need to be attentive when performing a 1st or 2nd trimester scan not only about the detection of pregnancy, but also of a uterine anomaly.[9] Presence of myometrium surrounding the gestational sac, absent continuity to the cervix, and pseudo pattern of the asymmetrical bicornuate uterus should alert us about a rudimentary horn pregnancy.[10]
During an assessment of a uterine anomaly, it is important to assess the vascularity of the connecting band as it could give the surgeon information regarding the possibility of increased bleeding during surgery if it is a thick band with increased vasculature. The surgeon could be prepared and take all the precautions during dissecting the band to maintain hemostasis. The patient could be counseled beforehand about the increased risk of hysterectomy if the band is thick and vascular. Due to the associated significant obstetric complications and maternal mortality[6] in pregnancy and due to increased vascularity leading to surgical difficulty in hemostasis, it is advisable to identify the anomaly before conception and resect it prophylactically.
The maternal mortality was 47.6% before the advent of ultrasound. However, after 1960, no maternal death has been reported due to rupture of the horn.[11] Nearly 80%–90% of rudimentary horn pregnancies rupture typically in the 10th–20th week of pregnancy due to the inability of the week musculature to accommodate a growing fetus.[6] Due to the scanty endometrium, placenta acreta is usually observed.[12] It is suggested that it is due to this that there is placental insufficiency leading to raised maternal S-alpha-fetoprotein, oligohydramnios, microhemorrhages, and intrauterine growth restriction (IUGR).[813] Rarely, if the pregnancy reaches term, the fetal salvage rate is between 0% and 13%.[6] A 3D ultrasound and/or magnetic resonance imaging (MRI) is advised if IUGR is observed with no risk factors and if uterine anomalies are suspected in an ultrasound examination in early pregnancy.[7]
It is justified to excise the rudimentary horn to treat dysmenorrhea and prevent endometriosis and intracornual pregnancy.[1] In case of a rudimentary horn diagnosed with pregnancy, surgical excision is the treatment of choice although methotrexate and intracardiac potassium chloride have been alternatively used.[6] Laparoscopic removal of the unruptured gestation with a preoperative workup to exclude urinary tract anomalies is crucial to avoid complications.[6]
In a two-dimensional (2D) ultrasound, a pregnancy was identified. We observed that there was no continuity between the gestational cavity and the cervix, and this ruled out the possibility of uterus didelphys. To determine the exact location of the pregnancy, 3D ultrasound was applied. The differential diagnosis between rudimentary horn (cornual) pregnancy, bicornuate pregnancy, and didelphic uterus pregnancy was analyzed. The uterine mantle was seen all around the gestational sac which was isoechoic to that of the myometrium in the left horn of the uterus, establishing the diagnosis of the pregnancy in the rudimentary horn. The identification of these diagnostic features which are possible with MRI is clearly made out in 3D ultrasound with equal resolution. 3D ultrasound also enables us to acquire images in coronal, sagittal, and frontal sections to reconstruct the uterine anomaly for a clear understanding of the doctor and clear explanation to the patient. The growing pregnancy in a rudimentary horn tends to displace the normal uterus giving a false picture of no uterine anomaly, which can only be detected by a 3D ultrasound examination or MRI.[7] Besides, 3D USG offers better patient tolerability. Although MRI is an excellent way of evaluating uterine anomalies, the drawback is that the procedure is expensive, time-consuming, and not widely available. Endovaginal 3D USG is a new technology that creates new volumes from a series of 2D images and, unlike MRI, an ultrasound creates real-time moving images of what you are looking at. It was concluded that the diagnostic accuracy of 3D ultrasound and MRI is similar when classifying uterine anomalies. The coronal sections of the uterus in 3D ultrasound and MRI are practically equivalent in establishing a relationship between the fundus and uterine cavity.[14] Hence, we suggest a 3D TVS- USG in early pregnancy for every patient with a suspected uterine anomaly.
CONCLUSION
Uterine rupture is the most common complication that may extend to a life-threatening condition by resulting hemoperitoneum and hemorrhagic shock. Therefore, timely diagnosis of rudimentary horn pregnancy is imperative. USG is a noninvasive method of screening and can be served as virtual laparoscopy to identify the uterine anomalies. In the present case, we demonstrated the advantage of three-dimensional reconstructed sonograms in identifying the pregnancy in the rudimentary horn.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/39/241523
REFERENCES
- Laparoscopic removal of the cavitated noncommunicating rudimentary uterine horn: Surgical aspects in 10 cases. Fertil Steril. 2005;83:432-6.
- [Google Scholar]
- Comparison of the ESHRE-ESGE and ASRM classifications of müllerian duct anomalies in everyday practice. Hum Reprod. 2015;30:569-80.
- [Google Scholar]
- The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol. 2005;105:1456-67.
- [Google Scholar]
- Laparoscopic management of rudimentary uterine horn pregnancy: Case report and literature review. JSLS. 2006;10:396-9.
- [Google Scholar]
- Pregnancy in non-communicating unicornuate uterus: Diagnosis difficulty and outcomes – A case report. Rev Bras Ginecol Obstet. 2017;39:640-4.
- [Google Scholar]
- Rupture of pregnant rudimentary uterine horn with fetal salvage. Acta Obstet Gynecol Scand. 1994;73:359-60.
- [Google Scholar]
- Rupture of noncommunicating rudimentary uterine horn pregnancy. Obstet Gynecol. 2002;100:1108-10.
- [Google Scholar]
- Rudimentary horn pregnancy: First-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med. 2005;24:219-23.
- [Google Scholar]
- Rudimentary uterine horn pregnancy. The 20th-century worldwide experience of 588 cases. J Reprod Med. 2002;47:151-63.
- [Google Scholar]
- Rupture of rudimentary uterine horn pregnancy at 37 weeks gestation with fetal survival. Arch Gynecol Obstet. 2006;274:325-6.
- [Google Scholar]
- Case of live birth in a non-communicating rudimentary horn pregnancy. J Obstet Gynaecol Res. 2005;31:329-31.
- [Google Scholar]
- Three-dimensional ultrasound in the diagnosis of Müllerian duct anomalies and concordance with magnetic resonance imaging. Ultrasound Obstet Gynecol. 2010;35:593-601.
- [Google Scholar]






