Translate this page into:
Ureteritis Cystica: A Radiologic Pathologic Correlation
Address for correspondence: Dr. Jennifer G Rothschild, Department of Urology, University of Rochester School of Medicine, 601 Elmwood Ave, Box 648, Rochester, NY 14642, USA. E-mail: jennifer_rothschild@urmc.rochester.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Ureteritis cystica (UC) is a benign condition that commonly affects the ureter and can mimic other conditions such as transitional cell carcinoma, blood clots, air bubbles, radiolucent stones, fibroepithelial polyps, and sloughed renal papillae. Radiographically, UC is characterized by multiple small, round, lucent defects, which cause scalloping of the ureteral margins when seen in profile. The scalloping is produced by the projection of the submucosal cysts into the lumen and represents an important differential feature of this disease. We present a case of UC with a radiological pathological correlation.
Keywords
Histopathology
retrograde pyelography
ureteroscopy
ureteritis cystica
INTRODUCTION

Ureteritis cystica (UC) is a rare and benign entity characterized by inflammatory pathology. The entity, first reported by Morgagni in 1761,[1] is a proliferative condition characterized by multiple cysts and filling defects in the urothelium.[2] UC may be associated with chronic urothelial irritation. Some studies have shown causes of UC to be nephrolithiasis[3] and urinary tract infections.[4] In one study, UC has been found in a patient following formalin treatment for cyclophosphamide-induced hemorrhagic cystitis.[5] Usually, there are no symptoms attributable to UC;[2] therefore, it is most frequently detected accidentally and the diagnosis is usually made during uretersoscopy or during radiography. Radiographically, a differential diagnosis of multiple transitional cell tumors, ureteral pseudodiverticula, nonopaque calculi, polyps, papillary tumors, vascular impressions, tuberculosis, iatrogenic gas bubbles, gas-forming microorganisms, and submucosal hemorrhage can be considered with an appropriate clinical correlation.
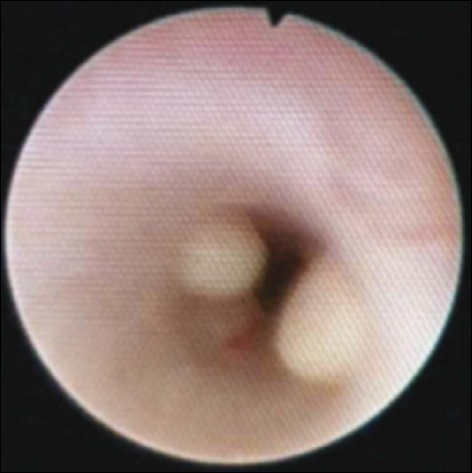
Our patient, a 62-year-old female, was found to have recurrent urinary tract infections (UTIs), while being evaluated for hip replacement surgery. Contrast-enhanced computed tomography (CT) of her abdomen and pelvis demonstrated bilateral 2- to 3-mm renal calculi. Since the stones were quite small, the patient underwent ureteroscopy for the planned treatment of her calculi. A retrograde pyelogram was performed that showed multiple filling defects [Figure 1]. A subsequent ureteroscopic examination showed multiple cystic lesions dispersed throughout the bladder as well as along both ureters and renal pelvises [Figure 2]. A biopsy of the cystic lesion was obtained and it proved to be UC [Figure 3].
- A 62-year-old female with ureteritis cystica of bilateral ureters. Retrograde pyleogram shows multiple smooth, well-rounded filling defects with sharp borders that protrude into the lumen of the ureter.
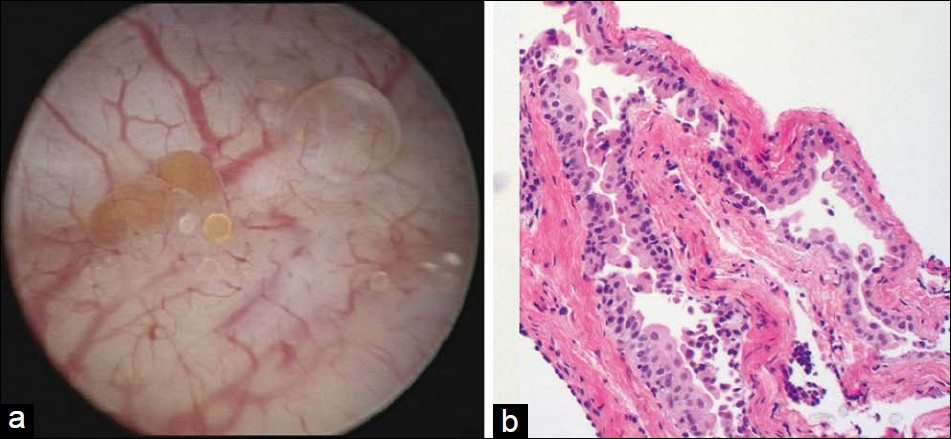
- A 62-year-old female with ureteritis cystica of bilateral ureters. Intraoperative ureterocystoscopy revealed multiple superficial cystic lesions lining (a) the inner wall of both the ureters and (b) the urinary bladder.

- Microscopic photograph of the ureteral biopsy shows a cystic structure with a thin epithelial lining. The epithelium lining consists of a benign urothelium with intact umbrella cells (hematoxylin and eosin stain).
RADIOLOGIC FEATURES
On intravenous urography or retrograde pyleography, the most common radiologic appearance of UC was that of numerous small, true contour defects of a near uniform size, 2–3 mm in diameter in the ureter and up to 2 cm in the renal pelvis. The majority of cysts appeared hemispherical in shape as opposed to air bubbles that appear round [Figure 1].
PATHOLOGIC FEATURES
UC manifests as cystic areas of glandular metaplasia associated with chronic urothelial inflammation. The more commonly seen presentation is in the bladder, where they are called cystitis cystica, here the nodules are usually located in the trigone and bladder neck region. Within islands of the benign-appearing urothelium are von Brunn's nests located in the lamina propria. Cystitis cystica occurs when the urothelium in the center of the von Brunn's nests has undergone eosinophilic liquefaction.[6]
The microscopic examination of our patient's ureteral biopsy showed an intact cystic structure lined by benign urothelium with intact umbrella cells, most consistent with cystitis cystica. Neither goblet cells nor dysplasia or malignancy was seen [Figure 3].
In conclusion, ureteral cystitis, although encountered on incidental diagnosis, should be considered during differential diagnosis, when there are small filling defects with a bead-like appearance along the urothelium of the renal pelvis, ureters, and bladder.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/23/80375
REFERENCES
- De sedibus et causis morborum per anatomen indagatis libri quinque. London: William Cooke Translation; 1822. p. :316-411.
- [Google Scholar]
- A rare condition: The ureteritis cystica. A report of two cases and review of literature. Inonu Universitesi Tip Fakultesi Dergisi. 2003;10:87-9.
- [Google Scholar]
- Should we get routine urothelial biopsies in every stone surgery? Int Urol Nephrol. 1997;29:415-20.
- [Google Scholar]
- Ureteritis cystica after treatment of cyclophosphamide-induced hemorrhagic cystitis. Urology. 1976;7:521.
- [Google Scholar]






