Translate this page into:
Occult Primary Neuroendocrine Tumor Metastasis to the Breast Detected on Screening Mammogram
Address for correspondence: Dr. Limin Yang, Department of Radiology, University of Iowa Hospitals and Clinics, Iowa City, IA, USA. E-mail: limin-yang@uiowa.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Metastatic tumors are rare in the breast. Well-differentiated neuroendocrine tumors (WDNETs) are slow-growing neoplasms that arise from neuroendocrine cells, particularly in the gastrointestinal tract and bronchial tree. Metastatic WDNET to the breast is a rare entity. We present a case report of ileal WDNET metastatic to the breast which was initially identified as a small mass in the patient's left breast on screening mammography. Targeted ultrasound identified a suspicious mass, and ultrasound-guided percutaneous core biopsy was performed. Pathology revealed metastatic WDNET. Breast magnetic resonance imaging (MRI) was then performed and demonstrated left axillary Level 2 lymphadenopathy, and liver lesions were suspicious for metastasis. The patient underwent abdominal computed tomography (CT) to evaluate for distant metastatic disease. A spiculated mass was found near the ileocecal valve, suggestive of primary ileal WDNET. In addition, CT identified multiple liver lesions, most compatible with metastasis. Indium 111 OctreoScan confirmed radiotracer uptake in the ileum consistent with primary neuroendocrine tumor. In this report, we review the imaging characteristics of metastatic WDNET to the breast by different imaging modalities including mammogram, ultrasound, and breast MRI.
Keywords
Breast imaging
breast metastasis
neuroendocrine tumor

INTRODUCTION
Breast metastases are uncommon breast lesions, accounting for approximately 2% of breast tumors. The most common primary tumors that metastasize to the breast are melanoma, contralateral breast carcinoma, and lung carcinomas.[123]
Well-differentiated neuroendocrine tumors (WDNETs) are slow-growing neoplasms arising from neuroendocrine cells, most commonly those found in the luminal gut, pancreas, and lung. When these tumors occur in the luminal gut or pancreas, the most common locations for metastatic disease are the regional lymph nodes and liver.[4]
WDNET metastatic to the breast is rare; however, a breast lesion can be the first manifestation of this nonmammary malignancy. The most common location of a primary WDNET that metastasis to the breast is the ileum.[1] There are several case reports of metastatic WDNET to the breast in the literature.[1234567] Most of these case reports focus on the challenge of the pathological diagnosis and rarely focus on the imaging findings of the metastatic WDNET to the breast. There are no previous reports demonstrating metastatic WDNET on breast magnetic resonance imaging (MRI) or OctreoScan. We present a case report of a metastatic WDNET that presented as a breast lesion on screening mammogram. The unique contribution of this case to the literature is the imaging finding of the metastatic WDNET in the breast in different imaging modalities, including mammogram, breast ultrasound, breast MRI, computed tomography (CT), and OctreoScan.
CASE REPORT
A 66-year-old woman underwent screening mammogram in October. During the screening mammogram, the patient mentioned a lump in the lower inner quadrant of her left breast. The mammogram did not show any abnormal finding in this palpable area; however, the mammogram did show an approximately 6 mm mass in the upper outer quadrant of the left breast [Figure 1]. This lesion was further evaluated with a targeted ultrasound. Ultrasound demonstrated an irregular hypoechoic mass at 2 O’clock position [Figure 2], corresponding to the abnormality seen on the mammogram. Given the suspicious appearance of the mass, ultrasound-guided core biopsy was performed.
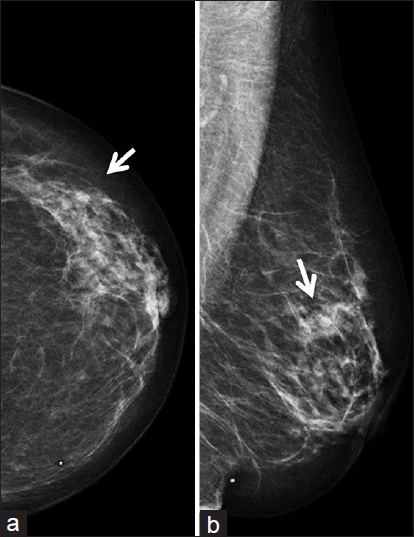
- A 66-year-old female with neuroendocrine tumor metastasis to the breast detected on mammogram. Screening mammogram craniocaudal (a) and mediolateral oblique (b) views demonstrates a 5 mm partially obscured mass (arrows) in the upper outer left breast.
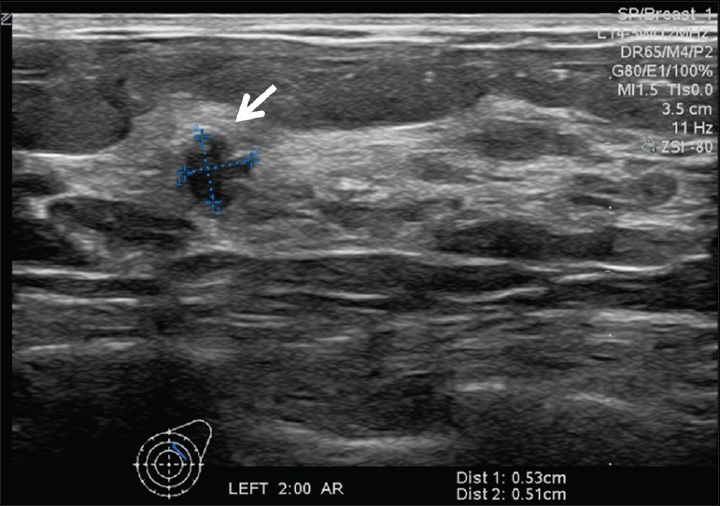
- A 66-year-old female with neuroendocrine tumor metastasis to the breast detected on screening mammogram. Ultrasound of the left breast demonstrates a 5 mm irregular hypoechoic mass (arrows) at 2:00 position, corresponding to mass seen on the screening mammogram.
Histologic sections showed a cellular neoplasm arranged in vague lobules with delicate fibrovascular cores embedded in a fibrous stroma [Figure 3]. The tumor cells were uniform and bland with a moderate amount of granular eosinophilic cytoplasm. The nuclei were round to oval and uniform with granular chromatin and absent nucleoli. The morphologic differential diagnosis included solid papillary carcinoma of the breast versus metastatic WDNET.
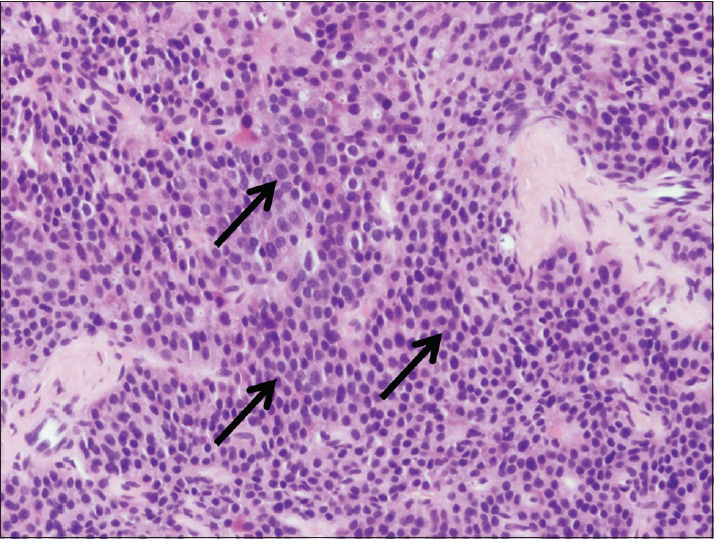
- A 66-year-old female with neuroendocrine tumor metastasis to the breast detected on screening mammogram. Solid area of tumor demonstrates uniform cells with moderate amounts of pink granular cytoplasm and uniform round to oval nuclei (arrows). Tumor cells are supported by delicate fibrovascular cores (×400).
Immunohistochemical stains showed the tumor cells were positive for synaptophysin, supporting neuroendocrine differentiation, which could be seen in either lesion. Importantly, the tumor cells were negative for estrogen receptor arguing against solid papillary carcinoma of the breast. In addition, the tumor cells were positive for caudal-related homeobox gene 2 and somatostatin receptor Type 2A. The immunohistochemical profile, in conjunction with the tumor morphology and the imaging findings, was most compatible with metastatic midgut WDNET.
Breast MRI was also performed to evaluate the extent of the disease which demonstrated the irregular enhancing mass in the upper outer quadrant of the left breast [Figure 4a], corresponding to the known biopsy proven metastatic neoplasm. MRI identified additional lesions in the liver as well as Level 2 lymphadenopathy seen between the pectoralis major and minor muscles (Rotter's node) [Figure 4b].
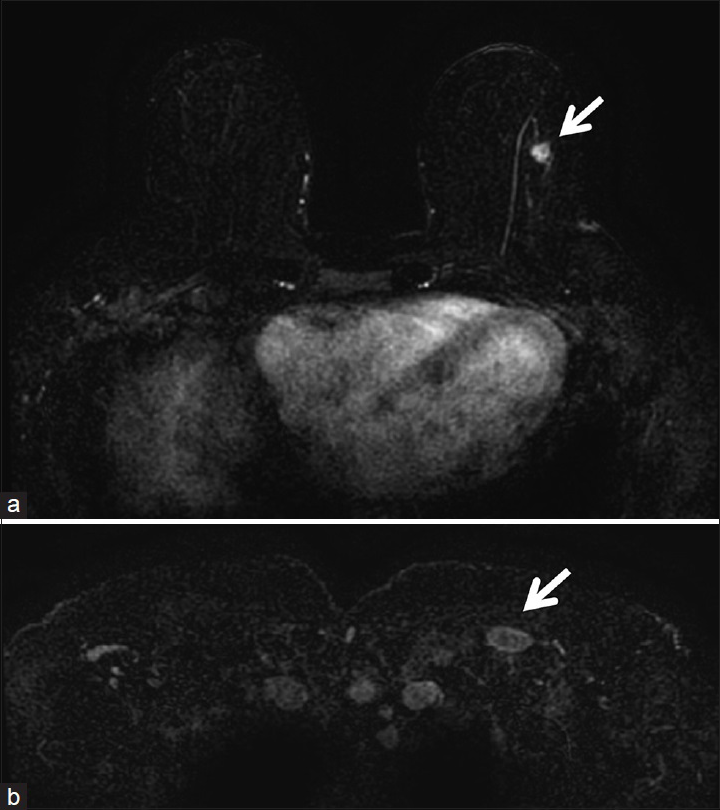
- A 66-year-old female with neuroendocrine tumor metastasis to the breast detected on screening mammogram. (a) Subtraction postcontrast images of breast magnetic resonance imaging show a 9 mm microlobulated enhancing mass (arrows) at 2:00 position of the left breast corresponding to the biopsy proven metastatic well-differentiated neuroendocrine tumor. (b) An enlarged lymph node (arrows) is present between the left pectoralis major and minor muscles (Rotter's node) consistent with Level II lymphadenopathy.
Subsequently, the patient underwent to a CT of the abdomen and pelvis which showed at least seven liver lesions, with the largest lesion at segment 4 measuring approximately 2.6 cm [Figure 5b]. There was also a spiculated mass with calcifications in the right lower quadrant near the ileocecal valve concerning for primary ileal WDNET [Figure 5a]. The patient then underwent OctreoScan [Figure 6] which demonstrated increased uptake in the left axillary Level 2 lymph node, within the breast lesion itself, in the liver lesions, and within the ileal mass consistent with primary ileal WDNET with metastasis to the breast, liver, and axillary lymph node. Fine needle aspiration of the left Level 2 axillary lymph node was performed, and the cytology was consistent with metastatic WDNET.
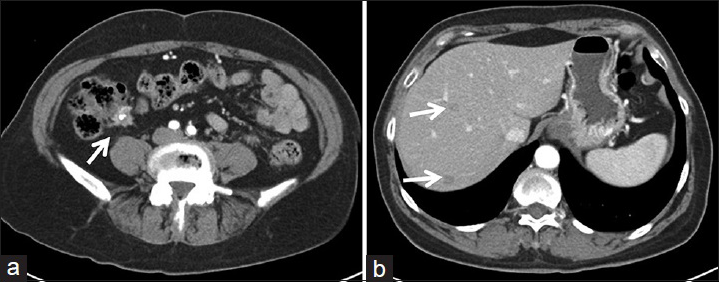
- A 66-year-old female with neuroendocrine tumor metastasis to the breast detected on screening mammogram. (a) Cross-section images from abdominal computed tomography scan show 2 cm irregular enhancing mass (arrow) at the ileocecal valve with central calcification consistent with primary well-differentiated neuroendocrine tumor. (b) Two hypoenhancing lesions (arrows) were noted in the liver most compatible with metastases.
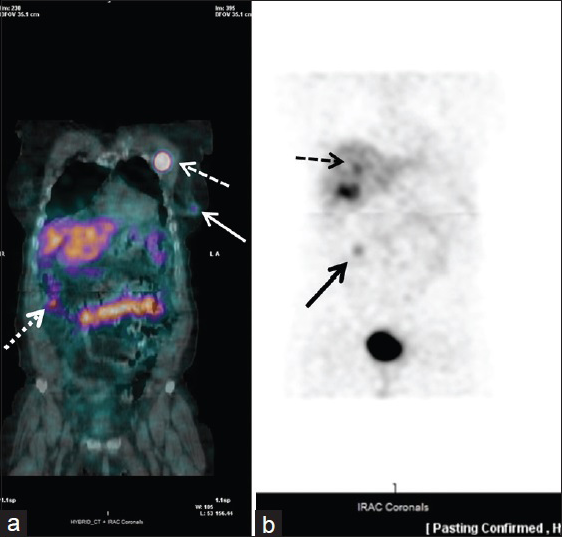
- A 66-year-old female with neuroendocrine tumor metastasis to the breast detected on screening mammogram. (a) Fused image of OctreoScan shows intense radiotracer activity in the lymph node (dashed arrow) between the left pectoralis major and minor muscles (Rotter's node), consistent with Level 2 lymphadenopathy and metastatic lesion in the left breast (solid arrow). There is also a focus of increased activity in the distal small bowel (dotted arrow), consistent with primary well-differentiated neuroendocrine tumor. (b) Planar image of OctreoScan reveals foci of increased activity in the liver (dashed arrow) compatible with liver metastases as well as demonstration of increased activity in the distal small bowel (solid arrow), consistent with primary well-differentiated neuroendocrine tumor.
On further questioning, the patient reported night sweats, heat intolerance, episodes of lightheadedness, some stomach pain, and constipation, consistent with symptoms of ileal WDNET with hepatic metastasis.
A treatment plan including ileal resection, cholecystectomy, and liver ablation with resection of the pectoralis lymph node as a separate operation was offered to the patient. The patient was very reluctant to pursue any operative treatment at this time.
DISCUSSION
WDNETs are slow-growing neoplasms derived from neuroendocrine cells. The most common sites are the gastrointestinal tract and bronchopulmonary system.[2] Classically, carcinoid syndrome is related to an ileal WDNET with hepatic metastases and production of various polypeptides including serotonin and substance P. Carcinoid syndrome, which includes diarrhea, flushing, and bronchospasm, is only present in 5–10% of patients with WDNET.[2]
Although there are no reliable criteria for distinguishing a primary breast lesion from metastatic WDNET, the appearance of the lesion on various imaging modalities may be helpful. On mammography, neuroendocrine tumor of the breast usually presents as a round mass with well-circumscribed borders.[2] In contrast, breast carcinoma usually presents as a spiculated mass with ill-defined borders. Calcifications are often present in a primary breast carcinoma; however, they are usually absent in metastatic WDNET.
On ultrasound, although both can present as a solid and irregular hypoechoic mass with increased vascularity,[2] metastatic WDNET commonly has more well-defined borders than primary breast cancer. The imaging features on ultrasound are not sufficient for diagnosis; however, a core needle biopsy is typically necessary for definitive classification. Our case is the second case reported in the literature, demonstrating the sonographic characteristics of metastatic WDNET on ultrasound imaging.
MRI shows both primary breast cancer and metastatic WDNET as a small, relatively circumscribed, oval enhancing mass with dynamic kinetics of early enhancement in the initial phase and rapid washout in the delayed phase.[2] Our case is the first case report to show the MRI findings of the metastatic WDNET to the breast.
Once the diagnosis of metastatic WDNET is made, an OctreoScan should be performed to localize the primary site and other sites of metastatic disease. Octreotide is a somatostatin analog radiolabeled with Indium-111 and used as the radiotracer in the OctreoScan scintigraphy. The radiolabeled molecule attaches to tumor cells that have receptors for somatostatin. Our case demonstrated radiotracer uptake in the ileum consistent with primary midgut WDNET with metastasis to the breast, liver, and axillary lymph node.
Since these tumors are uncommon, there are no clear recommendations regarding surgical management.[2] If clinically indicated, the surgical management should be similar to that for primary breast cancer taking into account the size and extent of the lesion. Options may include mastectomy or breast conserving surgery;[2] however, systemic therapy is still the cornerstone of therapy for metastatic disease.
CONCLUSION
We present a case report of a breast lesion found on screening mammogram, which was the first detected site of a metastatic WDNET of the midgut origin. Our case is the first in the published literature to show the images of metastatic WDNET to the breast on breast MRI and OctreoScan, and the second case report to show the images on ultrasound. Although metastatic WDNET is an uncommon breast lesion, it should be included in the differential diagnosis of the breast lesions and biopsy should be recommended for suspicious lesions. It is extremely important to make the correct diagnosis so that additional imaging modalities can be performed to the determinate the source of the primary tumor and additional sites of metastatic disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/41/191439
REFERENCES
- Breast metastasis: An unusual manifestation of a malignant carcinoid tumor. Cancer. 1977;40:3102-6.
- [Google Scholar]
- Solitary breast metastasis: First manifestation of an occult carcinoid of the ileum. Virchows Arch A Pathol Anat Histol. 1980;386:117-24.
- [Google Scholar]
- Neuroendocrine small cell carcinoma of the breast – A case report. Coll Antropol. 2012;36:1053-5.
- [Google Scholar]
- Breast metastasis as the first clinical manifestation of ileal neuroendocrine tumor. A challenging diagnosis with relevant clinical implications. Endocr Pathol. 2015;26:145-51.
- [Google Scholar]






