Translate this page into:
Noninvasive Fractional Flow Reserve for the Diagnosis of Lesion-specific Ischemia: A Case Example
Address for correspondence: Dr. Jesper Møller Jensen, Department of Cardiology, Aarhus University Hospital, Skejby, Brendstrupgaardsvej 100, Aarhus N - 8200, Denmark. E-mail: jespje@rm.dk
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A physically active 52-year-old male with atypical chest pain was referred to our department. A coronary computed tomography angiography (CCTA) showed a stenotic plaque in the mid left anterior descending coronary artery (LAD). A rest–stress Rubidium-82 myocardial perfusion was normal. One year later the patient sustained a cardiac arrest and percutaneous coronary intervention of the mid-LAD was successfully performed. The original CCTA data were submitted for noninvasive determination of fractional flow reserve (FFRCT) revealing an ischemia-producing lesion in the mid-LAD. This case demonstrates the inherent limitations of assessing lesion-specific ischemia. FFRCT shows promise as a new method for future selection of patients for coronary angiography.
Keywords
Coronary artery disease
fractional flow reserve
nuclear medicine
INTRODUCTION

Recently, a new method for assessing the functional significance of coronary computed tomography angiography (CCTA) has become available.[1234] This method uses patient-specific anatomic data from CCTA, mathematic modeling of coronary physiology, and computation of coronary pressure and blood flow utilizing computational fluid dynamics[1] to provide a noninvasive measure of fractional flow reserve (FFRCT), which can identify ischemia-producing stenoses.[234] The present case demonstrates the potential role of this new method as a gatekeeper to the catheterization laboratory.
CASE REPORT
A 52-year-old male was referred for evaluation of atypical chest discomfort after strenuous exercise and occasional stabbing pain in the left thorax not associated with physical activity. The patient exercised daily and he had competed in 39 marathons without any chest symptoms. He had familial hypercholesterolemia but no history of diabetes, hypertension, or smoking. The patient had discontinued cholesterol-lowering medication. The patient's blood pressure, electrocardiogram, and echocardiogram were normal. Total cholesterol and low density lipoprotein were 7.1 and 5.5 mmol/L, respectively. Due to the uncharacteristic nature of the patient's symptoms, a CCTA was performed. The calcium score was 140 and CCTA revealed calcified and noncalcified coronary atherosclerosis with a mixed, stenotic plaque in the mid left anterior descending coronary artery (LAD) [Figure 1]. Functional testing was scheduled with a rest–stress Rubidium-82 myocardial perfusion scan. Myocardial perfusion and coronary flow reserve were normal during adequate stress response to adenosine (140 μg/kg/min) [Figure 2]. Atorvastatin was prescribed and the patient continued his high level of daily physical activity.

- 52-year-old male with atypical chest pain. Coronary computed tomography angiography curved planar reformation image of the mid left anterior descending coronary artery. The white arrow marks an area suspicious for significant stenosis (>70%).
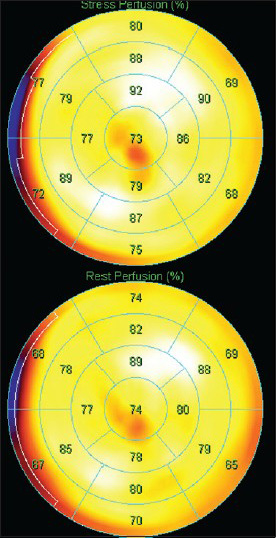
- 52-year-old male with atypical chest pain. Static rubidium-82 perfusion images (17 segment polar maps) demonstrates no difference between stress (top) and rest perfusion (bottom). Images were acquired 150 s after injection of 1110 MBq Rb82. Total acquisition time was 270 s.
One year later, following strenuous running, the patient sustained a cardiac arrest. Cardiopulmonary resuscitation was started immediately with successful electrical cardioversion of ventricular fibrillation and return of spontaneous circulation 6 min after the alarm. The electrocardiogram showed ST-elevation [Figure 3]. Acute invasive angiography revealed occlusion of the mid-LAD. Normal coronary flow was restored after recanalization and stenting [Figure 4]. Ten days later, transthoracic echocardiography showed left ventricular ejection fraction of 40–45% with apical hypokinesis. The patient was advised cardiac rehabilitation.
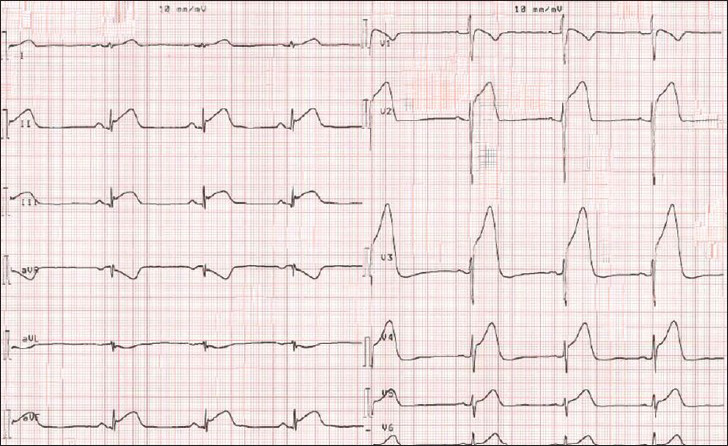
- 53-year-old male presenting with severe chest pain and cardiac arrest, which was successfully treated with resuscitation and cardioversion. 12-lead electrocardiogram shows massive ST-elevation consistent with anterior ST-elevation myocardial infarction.
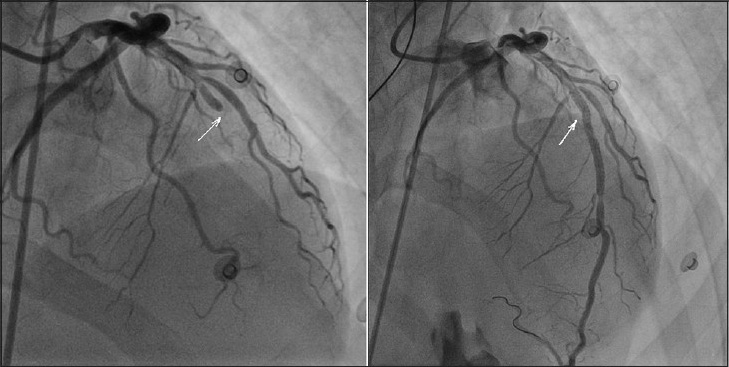
- 53-year-old male presenting with severe chest pain and cardiac arrest, which was successfully treated with resuscitation and cardioversion. Invasive angiography shows prestent image of left anterior descending coronary artery occlusion marked by the white arrow (left side, angiography projection: 4° right anterior oblique and 24° cranial) and poststent image of re-perfused left anterior descending coronary artery with the white arrow marking the point of previous occlusion (right side, angiography projection: 6° right anterior oblique and 30° cranial).
As a blind study, we submitted the patient's CCTA data, which had been obtained one year earlier and had revealed a highly significant ischemia-producing lesion in the mid-LAD, for FFRCT analysis [Figure 5]. FFRCT analysis was performed at HeartFlow (Redwood City, CA, USA) utilizing updated proprietary software. Computation of noninvasive FFRCT from CCTA image data requires a physiologic model of coronary blood flow. The physiologic model is based on three underlying principles as described in detail by Taylor et al.,:[1] (i) The total resting coronary blood flow can be quantified relative to the myocardial mass, (ii) The microcirculatory vascular resistance at rest is inversely proportional to the size of the coronary arteries supplying the myocardium, and (iii) The vasodilatory response of the coronary microcirculation to adenosine infusion can be predicted, allowing computational modeling of the maximal hyperemic state. The integration of the model of coronary physiology to 3-dimensional computational models allows computation of coronary flow and pressure at each point in the coronary arteries under hyperemic conditions.
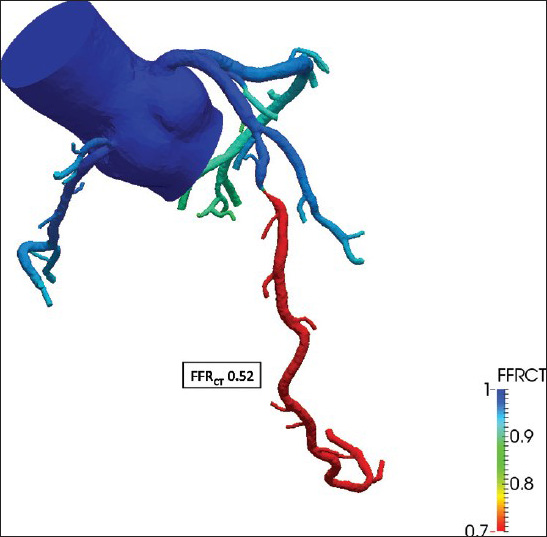
- 52-year-old male with atypical chest pain. Fractional flow reserve (FFRCT = 0.52) derived from coronary computed tomography images and based on a physiologic model of coronary blood flow using three principles: (1) The total resting coronary blood flow can be quantified relative to the myocardial mass, (2) The microcirculatory vascular resistance at rest is inversely proportional to the size of the supplying coronary arteries, and (3) The vasodilatory response of the coronary microcirculation to adenosine can be predicted, allowing computational modeling of maximal hyperemia. The integration of the physiological model into 3-dimensional computational models allows computation of coronary flow and pressure under hyperemic conditions.
DISCUSSION
This case demonstrates the inherent limitations of assessing lesion-specific ischemia utilizing currently available noninvasive imaging modalities. While CCTA can reliably identify coronary stenoses, it cannot assess their functional significance.[5] A coronary stenosis ≥50% detected by conventional angiography has a significantly lower diagnostic accuracy when compared with FFRCT in detecting significant coronary artery disease as defined by FFR.[4] Myocardial perfusion imaging can detect perfusion abnormalities, but cannot assess the hemodynamic significance of individual coronary lesions.[6] Moreover, myocardial perfusion imaging misclassifies up to 58% of ischemic myocardial territories when compared with FFR in multivessel disease.[7] The prospective, randomized Fractional Flow Reserve versus Angiography for Multivessel Evaluation (FAME 2) study[8] has demonstrated reduced mortality and myocardial infarction from revascularization of lesions with FFR <0.80 when compared with standard practice. One putative mechanism for this benefit is identification of stenoses at high risk for plaque rupture. Noninvasive FFRCT values compare well with measured FFR,[234] thus FFRCT may play a major role for selection of patients for coronary angiography. Large-scale prospective studies comparing the effect of FFRCT versus standard diagnostic evaluation are ongoing.[9]
CONCLUSION
FFRCT shows promise as a new method to identify lesion-specific ischemia noninvasively and, thus, FFRCT may play a role in the selection of patients for coronary angiography.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/3/150443
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: Scientific basis. J Am Coll Cardiol. 2013;61:2233-41.
- [Google Scholar]
- Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol. 2011;58:1989-97.
- [Google Scholar]
- Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 2012;308:1237-45.
- [Google Scholar]
- Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps) J Am Coll Cardiol. 2014;63:1145-55.
- [Google Scholar]
- Quantitative computed tomographic coronary angiography: Does it predict functionally significant coronary stenoses? Circ Cardiovasc Imaging. 2014;7:43-51.
- [Google Scholar]
- Prevalence, location, and extent of significant coronary artery disease in patients with normal myocardial perfusion imaging. J Nucl Cardiol. 2014;21:284-90.
- [Google Scholar]
- Fractional flow reserve and myocardial perfusion imaging in patients with angiographic multivessel coronary artery disease. JACC Cardiovasc Interv. 2010;3:307-14.
- [Google Scholar]
- Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med. 2014;371:1208-17.
- [Google Scholar]
- ClinicalTrials.gov A service of the U.S. National Institutes of Health. Available from: https://clinicaltrials.gov/ct2/show/NCT01943903?term = PLATFORMandrank = 2
- [Google Scholar]






