MRI Findings of Coexistence of Ectopic Neurohypophysis, Corpus Callosum Dysgenesis, and Periventricular Neuronal Heterotopia
Address for correspondence: Dr. Harun Arslan, Department of Radiology, Van Training and Research Hospital, Van, Turkey. E-mail: harun.ars75@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Ectopic neurohypophysis is a pituitary gland abnormality, which can accompany growth hormone deficiency associated with dwarfism. Here we present magnetic resonance imaging (MRI) findings of a rare case of ectopic neurohypophysis, corpus callosum dysgenesis, and periventricular neuronal heterotopia coexisting, with a review of the literature.
Keywords
Corpus callosum dysgenesis
ectopic neurohypophysis
magnetic resonance imaging
periventricular neuronal heterotopia
INTRODUCTION

Ectopic neurohypophysis may be accompanied by midline brain defects and some degree of endocrine disorders. The associated endocrine disease varies from isolated growth hormone (GH) deficiency to multiple anterior pituitary hormone deficiencies, but posterior pituitary function remains unchanged. Anterior pituitary hormone deficiencies may present with varied clinical manifestations like growth failure, central hypothyroidism, or underdeveloped secondary sexual characters. At the same time, the disease starting with GH deficiency can progress to pan hypopituitarism with time.[1] Neurohypophysis is observed as a bright dot behind normal posterior lobe of adenohypophysis on T1-weighted magnetic resonance (MRI) images. Ectopic neurohypophysis is specifically monitored at the level of the median eminence of the hypothalamus in imaging studies. Because of its rareness, we present radiological findings of a case that showed coexistence of ectopic neurohypophysis, corpus callosum dysgenesis, and periventricular neuronal heterotopia, with accompanying literature review.
CASE REPORT
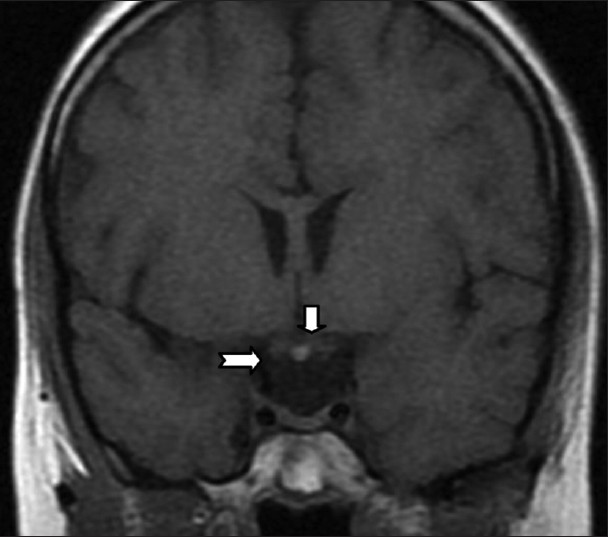
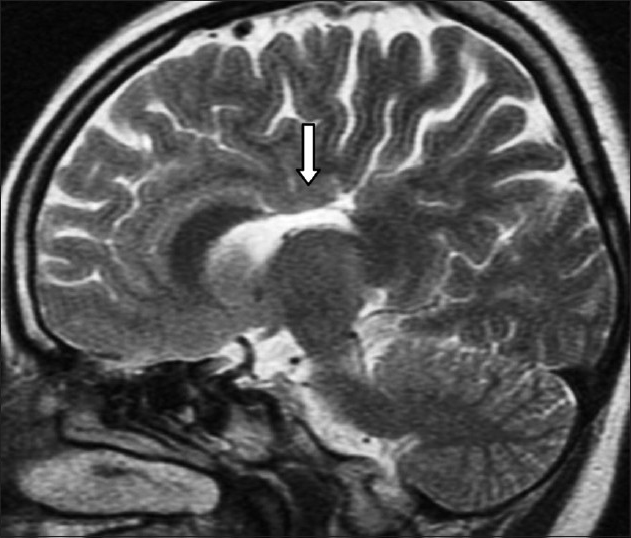
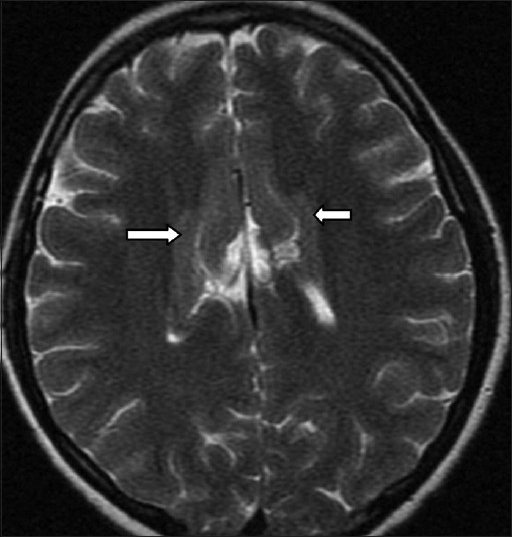
A 21-year-old female patient was admitted to the neurology clinic of our hospital with complaints of forgetfulness, twitching of eyes, and short stature. The patient's height was 135 cm and weight was 45 kg. Her past medical history was unremarkable. Laboratory measurements for the pituitary hormones uncovered a very low level of GH (0.06 ng/ml), while the other hormones and their levels were normal [Table 1]. In MR images of the brain and pituitary (1.5-T system, GE Medical Systems Signa, Milwaukee, WI), the neurohypophysis was seen at the ectopic site as a bright dot at the level of the optic chiasm on coronal T1 images. Infundibular part was thinner than usual [Figure 1]. At the same time, partial dysgenesis of corpus callosum and periventricular neuronal heterotopia were observed on the MR images [Figures 2 and 3]. Ophthalmologic examinations for a possible involvement of the optic discs, including visual acuity test, visual field test, and dilated fundoscopy were completely normal. Also, the systemic evaluation of the patient for other possible associations was normal.
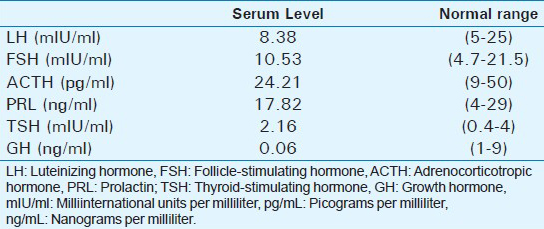
- 21-year-old female patient with complaints of forgetfulness, twitching of eyes, and short stature later diagnosed with coexistence of ectopic neurohypophysis, corpus callosum dysgenesis, and periventricular neuronal heterotopia. A coronal non-contrast T1-weighted MRI image reveals a hyperintense ectopic posterior pituitary adjacent to the optic chiasm, at the level of the median eminence of the hypothalamus (arrows). The bright dot in the ectopic site indicates neurohypophysis.
- 21-year-old female patient with complaints of forgetfulness, twitching of eyes, and short stature later diagnosed with coexistence of ectopic neurohypophysis, corpus callosum dysgenesis, and periventricular neuronal heterotopia. Sagıttal T2-weighted MRI image reveals partial dysgenetic view of the corpus callosum and protrusion of cingulated gyrus (arrow).
- 21-year-old female patient with complaints of forgetfulness, twitching of eyes, and short stature later diagnosed with coexistence of ectopic neurohypophysis, corpus callosum dysgenesis, and periventricular neuronal heterotopia. Axıal T2-weighted MRI image reveals an appearance that is compatible with periventricular-subependymal heterotopic neuronal tissue (arrows).
DISCUSSION
The pituitary gland consists of two portions: The adenohypophysis and the neurohypophysis. The neurohypophysis comprises the posterior pituitary lobe, the infundibulum, and the median eminence of the hypothalamus. The adenohypophysis and the neurohypophysis differ from each other, both embryologically and histologically. The neurohypophysis is formed by the evagination of neural tissue from the floor of the third ventricle. It consists of the distal axons of the hypothalamic magnocellular neurones that shape the neurohypophysis. After its downward migration, it is encapsulated together with the ascending ectodermal cells of Rathke's pouch, which form the adenohypophysis. The pituitary gland acts as an endocrine gland under control of the hypothalamus via the infundibular stalk.[2]
Regardless of the underlying cause, the ectopic neurohypophysis results from incomplete downward growth and fusion of the neurohypophysis with the adenohypophysis in the sella. Possible pathophysiologic mechanisms for ectopic neurohypophysis development are transection of the pituitary stalk followed by hypertrophy of the proximal axons with subsequent reorganization. Also trauma of the pituitary stalk due to vascular accidents, anoxia, or compression injuries have been suggested as acting through similar mechanisms leading to reorganization of the proximal neurons of the neurohypophysis.[3] Although early studies describe a traumatic cause in the etiology of the ectopic neurohypophysis, more recent studies favor a genetic basis, supported by rare familial cases of ectopic neurohypophysis.[45] The ectopic neurohypophysis cases have been reported in idiopathic GH deficiency or in subjects with HESX1, LHX4, and SOX3 gene mutations.[2]
Again, a few earlier reports have suggested that ectopic neurohypophysis may share a similar pathogenesis as septo-optic dysplasia, which classically has features of optic nerve hypoplasia, hypothalamic-pituitary dysfunction, and agenesis of the septum pellucidum. The HESX1 homebox gene has been implicated in both of these conditions.[6]
The other well-known malformations associated with ectopic neurohypophysis include Chiari 1 malformation, agenesis of the corpus callosum, persistent cranio-pharyngeal canal, Kallmann syndrome, basilar impression, medial deviation of the carotid arteries, microcephaly, cerebellar atrophy, and vermian dysplasia. Associated ophthalmic and midline facial abnormalities, such as a single central incisor tooth, are typical, and non-midline somatic conditions, including cardiac and musculoskeletal abnormalities, have been noted. Breech presentation and neonatal hypoglycemia are also commonly reported.[456]
As a result of ectopic neurohypophysis and associated stalk abnormalities, factors released by the hypothalamus, which usually travel down the portal circulation to the anterior pituitary can only reach their target via the general circulation. The patients with an ectopic neurohypophysis located at the median eminence and no visible pituitary stalk present a more severe form of the disease, with multiple anterior hormone deficiencies. Whereas visibility of the pituitary stalk and an ectopic neurohypophysis located at some point along the stalk is associated with isolated GH deficiency.[36]
In our patient, there were radiological findings of coexistence of ectopic neurohypophysis, corpus callosum partial dysgenesis, and periventricular neuronal heterotopia. Dysgenesis of the corpus callosum represents an in utero developmental anomaly, which may be complete (agenesis) or partial. It may occur in isolation or in association with other central nervous system or systemic malformations. Isolated partial dysgenesis of the corpus callosum is often asymptomatic.[7] Periventricular heterotopia is the most common form of gray matter heterotopia and is characterized by nodules of gray matter located immediately beneath the ependyma of the lateral ventricles. For this reason, it is also known as subependymal heterotopia. They are most commonly seen in the region of the trigones and occipital horns. They are most frequently associated with epilepsy and sometimes developmental delay.[8] Previous reports of cases with coexistent periventricular heterotopia and ectopic neurohypophysis suggest both conditions can share a common underlying causative mechanism, even though pituitary development occurs earlier in fetal life than does neuronal migration.[6] Another study has found HESX1 mutations in only 5 of 93 patients with ectopic neurohypophysis, indicating that other unrecognized genes or local environmental factors are likely to be involved in the ectopic neurohypophysis development.[9]
In ectopic neurohypophysis cases, normal neurohypophysis bright spot is absent in the sella and there is high T1 signal at the median eminence (floor of third ventricle) or along infundibuler stalk, instead of normal sellar position, on unenhanced T1-weighted images. Infundibuler stalk may be tiny or absent. Although controversy still exists on the source of this distinct signal, it has most recently been attributed to phospholipids within the walls of the secretory vesicles containing the arginine vasopressin neurophysin complex.[10] Distinction of the ectopic neurohypophysis from dermoid tumor or lipoma can be confirmed by images obtained using fat saturation.[910]
In this article, because of its rareness, we present MRI findings of concurrence of ectopic neurohypophysis, dysgenesis of the corpus callosum, and periventricular neuronal heterotopia. No systemic association was detected in our case.
CONCLUSION
Ectopic neurohypophysis can be detected by MRI. Radiologists should carefully evaluate MR images in patients with epilepsy or hormone deficiency for the possibility of ectopic neurohypophysis and neuronal heterotopia. In the presence of ectopic neurohypophysis, other associated cerebral malformations should be thoroughly investigated.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/22/131649
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Hypothalamic-pituitary dysfunction ingrowth hormone-deficient patients with pituitary abnormalities. J Clin Endocrinol Metab. 1991;73:79-83.
- [Google Scholar]
- Developmental abnormalities of the posterior pituitary gland. Endocr Dev. 2009;14:83-94.
- [Google Scholar]
- Pituitary Stalk and ectopic hyperintense T1 signal on magnetic resonance imaging. Am J Dis Child. 1993;147:647-52.
- [Google Scholar]
- MR findings in growth hormone deficiency: Correlation with severity of hypopituitarism. AJNR Am J Neuroradiol. 1998;19:1495-9.
- [Google Scholar]
- Growth hormone deficiency with ectopic neurohypophysis: Anatomical variations and relationship between the visibility of the pituitary stalk asserted by magnetic resonance imaging and anterior pituitary function. J Clin Endocrinol Metab. 1999;84:2408-13.
- [Google Scholar]
- Ectopic posterior pituitary lobe and periventricular heterotopia: Cerebral malformations with the same underlying mechanism? AJNR Am J Neuroradiol. 2002;23:1475-81.
- [Google Scholar]
- Agenesis and dysgenesis of the corpus callosum: Clinical, genetic and neuroimaging findings in a series of 41 patients. Am J Med Genet A. 2008;146:2501-11.
- [Google Scholar]
- Disorders of cortical formation: MR imaging features. AJNR Am J Neuroradiol. 2009;30:4-11.
- [Google Scholar]
- Molecular effects of novel mutations in Hesx1/HESX1 associated with human pituitary disorders. Development. 2001;128:5189-99.
- [Google Scholar]
- Posterior pituitary ectopia: Another hint toward a genetic etiology. AJNR Am J Neuroradiol. 2000;21:1116-8.
- [Google Scholar]






