Translate this page into:
Massive Left-sided Congestive Colitis Due to Idiopathic Inferior Mesenteric Arteriovenous Malformation
Address for correspondence: Dr. Laura Martí Gelonch, Department of General Surgery, Hospital Universitario Donostia, San Sebastián, Spain. E-mail: lauramartig_@hotmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Arteriovenous malformations (AVM) of the inferior mesenteric artery are rare. They may be primary (congenital or idiopathic) or secondary (acquired) after trauma or of iatrogenic origin. Of the abdominal AVM, the inferior mesenteric trunk is the least commonly involved. Most reported cases are of iatrogenic origin, resulting from colon surgery. Only 17 cases have been described and published in the literature. The objective of this work is to make known a case treated in our center. We present a case of 73-year old male, who came to the emergency service with symptoms of abdominal distension, pain lasting 48 hours along with months of diarrhoea. CT scan and an abdominal CT angiography showed a massive left-sided congestive colitis due to idiopathic inferior mesenteric arteriovenous malformation. In our case, the decision was to carry out the treatment in two stages. Embolisation was performed in the first stage in order to decrease the blood flow and the risk of intraoperative bleeding, followed by resective surgery of the affected colon.
Keywords
Arteriovenous malformation
congenital
congestive colitis
inferior mesenteric trunk

INTRODUCTION
Arteriovenous malformations (AVMs) of the inferior mesenteric vasculature are rare. They may be primary (congenital or idiopathic) or secondary due to trauma or iatrogeny. The inferior mesenteric trunk is the least commonly affected territory of visceral vessel AVMs. Most reported cases are iatrogenic in etiology following colon surgery. Congenital cases are the result of persistence of embryonic vessels that do not differentiate into arteries and veins and interconnect the arterial and venous system. Mesenteric AVMs may be symptomatic and in severe cases can cause portal hypertension and right heart failure due to left-right shunting.[12]
CASE REPORT
We present a case of a 73-year-old male with a history of alcohol use and smoking, arterial hypertension, diabetes mellitus type 2, hypertrophic cardiomyopathy, and Bence Jones monoclonal gammopathy with no surgical or trauma history. He presented to the emergency department with symptoms of abdominal distention and pain for 48 h as well as several months of watery diarrhea and defecation urgency. Physical examination revealed abdominal distension with shifting dullness and a positive fluid wave as well as a palpable mass on the left flank. He was admitted to the General Medicine Service for detailed investigation. Abdominal ultrasound revealed large volume abdominal ascites and portal vein in the high limit of normality [Figure 1]. Paracentesis was performed which was negative for malignant cells. Serum-ascites albumin gradient was 15 g/L, which indicates portal hypertension as the origin of ascites. Blood tests revealed normal tumor markers except an elevation of CA-125. Computed tomography (CT) abdomen and pelvis with contrast showed wall thickening of the descending and sigmoid colon with edematous wall and extensive collateral formation in the inferior mesenteric artery (IMA) territory [Figure 2]. Optical colonoscopy revealed edema in the left colon corresponding to the wall thickening seen on CT scan, but no mass lesions were seen endoscopically, and no biopsy was performed [Figure 3]. CT angiography of the abdomen and pelvis confirmed a large arterial malformation involving the IMA [Figure 4].
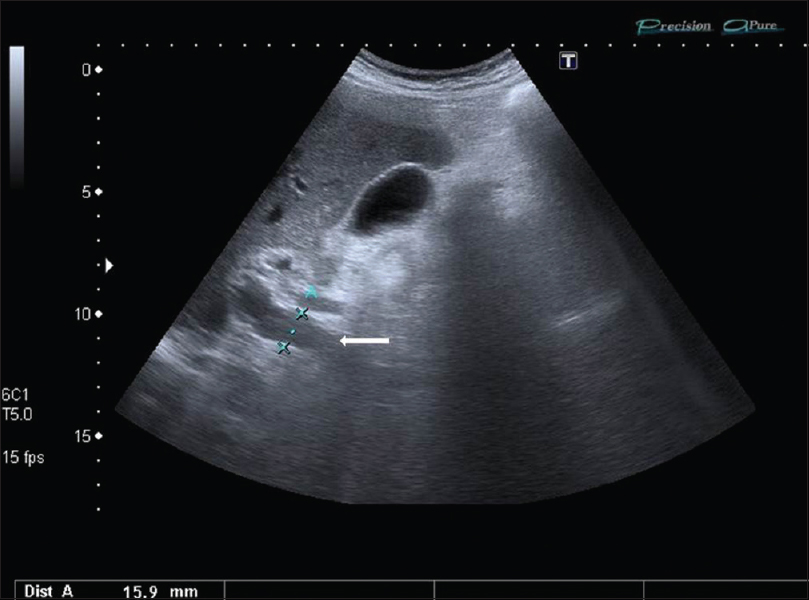
- A 73-year-old man with an arteriovenous malformation of the inferior mesenteric artery; abdominal ultrasound revealed a portal vein (white arrow) in the high limit of normality (15 mm).
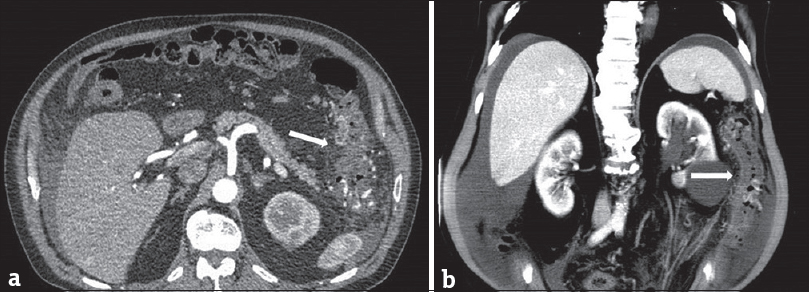
- A 73-year-old man with an arteriovenous malformation of the inferior mesenteric artery; (a) transversal computed tomography scan showed wall thickening of the descending colon (white arrow). (b) Coronal image (white arrow showed wall thickening of the descending colon).
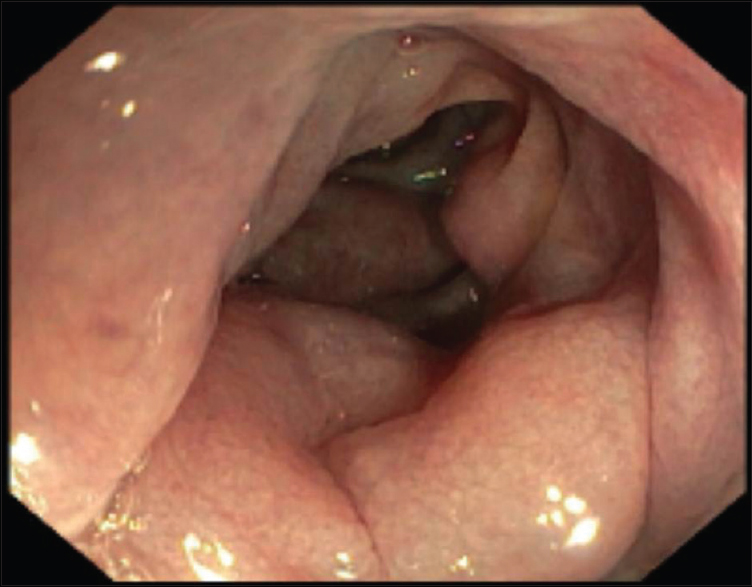
- A 73-year-old man with an arteriovenous malformation of the inferior mesenteric artery; colonoscopy revealed edema in the left colon.
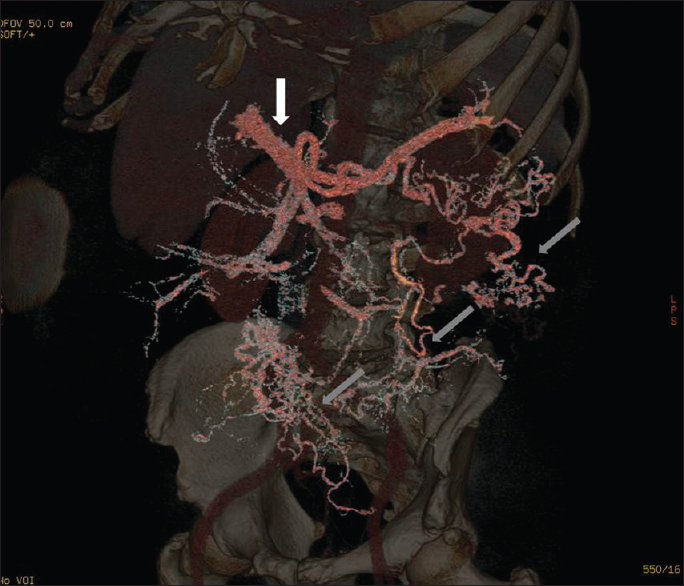
- A 73-year-old man with an arteriovenous malformation of the inferior mesenteric artery; computed tomography angiography of the abdomen and pelvis confirmed a large arterial malformation involving the inferior mesenteric artery (white arrow). Gray arrows revealed abnormal vascularization.
Treatment
Treatment was initiated with diuretics, and the patient had a slight improvement in symptoms. Subsequently, the patient underwent selective microcoil embolization of IMA branches supplying the splenic flexure, descending colon and sigmoid, selectively excluding the superior hemorrhoidal artery [Figure 5]. After embolization, there was a significant decrease in the size of the palpable mass on physical examination. The patient was observed postembolization for pain management followed by laparotomy 24 h later. Intraoperative findings revealed 3 litres of ascites as well as a swollen left colon with swollen epiploic appendices and a very congested mesentery obliterating retroperitoneal planes. A large draining vein within the transverse mesocolon level was observed [Figure 6]. A left colectomy was performed from the transverse colon to the upper rectum with transverse colorectal anastomosis. There were no complications during the postoperative period, and the patient was discharged after 6 days. The pathological specimen revealed significant vascular proliferation and collateral formation within the mesentery and congestive changes in the mucosa secondary to a large AVM [Figure 7].
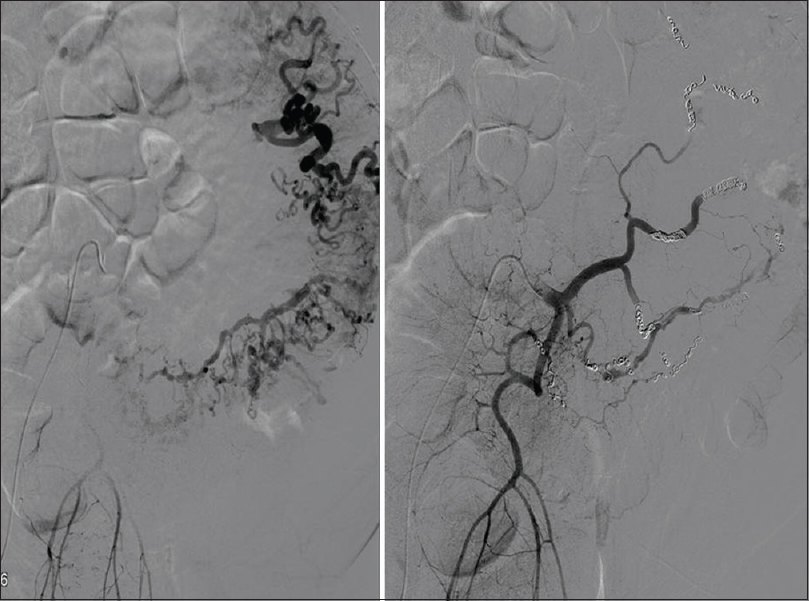
- A 73-year-old man with an arteriovenous malformation of the inferior mesenteric artery; arteriography; pre-embolization image (left) and post-embolization image (right). All branches of the inferior mesenteric artery are embolized with microcoils, from the splenic angle to the sigmoid branches, respecting the territory of the upper hemorrhoidal artery.
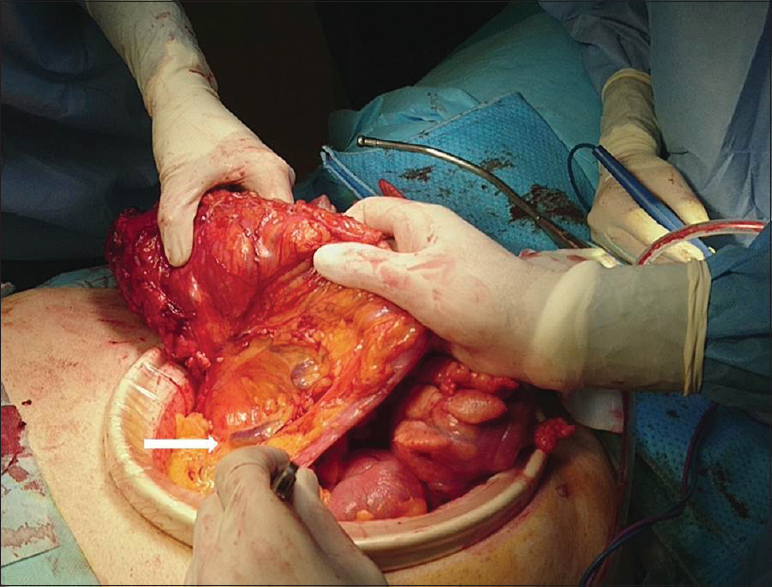
- A 73-year-old man with an arteriovenous malformation of the inferior mesenteric artery; a large draining vein within the transverse mesocolon level was observed intraoperatively (white arrow).

- A 73-year-old man with an arteriovenous malformation of the inferior mesenteric artery; resected colon specimen.
DISCUSSION
AVMs of the visceral vasculature are rare, occurring in order of decreasing frequency within the hepatic artery (45%), splenic artery (30%), superior mesenteric artery, gastroduodenal artery, and least commonly, the IMA.[2] AVMs of the IMA can be primary or secondary, but the majority are secondary to penetrating trauma or colon surgery.[34] Congenital visceral AVMs are exceedingly rare, with only 17 cases having been described in the literature.[1] These vascular malformations act as left-right shunts, and the severity of the symptoms are flow dependent. At the intestinal level, this provokes physiological changes that result in abdominal pain (62.5%), gastrointestinal bleeding (56.3%), portal hypertension secondary to the increase of flow through the portal system (50%), ischemic colitis (43.8%), palpable/pulsatile mass (12.5%) secondary to intestinal congestion and variceal bleeding secondary to portal hypertension.[1234] Right heart failure or portal hypertension can result in the most severe cases.[1]
Visceral AVMs are usually identified first with cross-sectional imaging obtained during the workup of the nonspecific symptoms described above. To prevent erroneous diagnoses and inadequate treatment, Athanasiou et al.,[1] proposed the following criteria to establish the diagnosis: (1) the presence of ischemic colitis; (2) confirmation of the presence of AVM with an angiogram; and (3) intraoperative confirmation of colon congestion. Preoperative conventional angiography has the benefit of determining precisely which vascular territories are involved in cases which are not clear, in addition to permitting embolization of the AVM before definitive surgical resection.
The treatment should be individualized to each patient depending on the location and size of the AVM and the severity of symptoms. The initial treatment of visceral vessel AVMs is endovascular embolization before definitive surgical resection with a hemicolectomy or total colectomy. Embolization is the safest and least invasive technique;[56] however, AVMs have been reported to recur due to inadequate embolization and/or further collateral formation if surgery is not subsequently performed. Endovascular embolization is not recommended in large AVMs with vessels >8 mm diameter or with high-flow AVMs due to the risk of nontarget distal embolization of material, thrombosis, and ischemia. In these cases, the treatment is surgery alone.[78]
CONCLUSION
Our case is an example of a large symptomatic idiopathic inferior mesenteric AVM resulting in portal hypertension secondary to the increase of flow through the portal system. Given the large vascular network created by the AVM in our case, the decision was made to carry out the treatment in two stages. Embolization was performed first to decrease the blood flow, determine specifically which vascular territory was affected, and reduce the risk of intraoperative bleeding, followed by left hemicolectomy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/40/216812
REFERENCES
- Inferior mesenteric arteriovenous fistula: Case report and world-literature review. World J Gastroenterol. 2014;20:8298-303.
- [Google Scholar]
- Acute massive congestive ischaemic colitis related to inferior mesenteric arteriovenous malformation. BJR Case Rep. 2016;2:20150275.
- [Google Scholar]
- Inferior mesenteric arteriovenous malformation: An unusual cause of ischemic colitis. Ann Gastroenterol. 2012;25:165.
- [Google Scholar]
- Ischemic colitis: An unusual case of inferior mesenteric arteriovenous fistula causing venous hypertension. Report of a case. Dis Colon Rectum. 2008;51:1422-4.
- [Google Scholar]
- Inferior mesenteric arteriovenous fistula treated by percutaneous arterial embolization: A breathtaking story! Diagn Interv Imaging. 2014;95:85-6.
- [Google Scholar]
- Inferior mesenteric arteriovenous fistula eight years after sigmoidectomy. Intern Med. 2002;41:543-8.
- [Google Scholar]
- Inferior mesenteric arteriovenous fistulas. Report of a case. Ann Chir. 2005;130:417-20.
- [Google Scholar]
- Inferior mesenteric arteriovenous fistula with ischemic colitis: Multidetector computed tomographic angiography for diagnosis. Turk J Gastroenterol. 2009;20:67-70.
- [Google Scholar]






