Translate this page into:
Low Dose versus Standard Single Heartbeat Acquisition Coronary Computed Tomography Angiography
Address for correspondence: Prof. Ernesto Di Cesare, Department of Biotechnological and Applied Clinical Science, University of L’aquila, Via Vetoio 1,67100 L’aquila, Italy. E-mail: ernesto.dicesare@cc.univaq.it
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Purpose:
The aim of this study was to compare image quality and mean radiation dose between two groups of patients undergoing coronary computed tomography angiography (CCTA) using a 640-slice CT scanner with two protocols with different noise level thresholds expressed as standard deviation (SD).
Materials and Methods:
Two-hundred and sixty-eight patients underwent a CCTA with 640 slice CT scanner. In the experimental group (135 patients), an SD 51 protocol was employed; in the control group (133 patients), an SD 33 protocol was used. Mean effective dose and image quality with both objective and subjective measures were assessed. Image quality was subjectively assessed using a five-point scoring system. Segments scoring 2, 3, and 4 were considered having diagnostic quality, while segments scoring 0 and 1 were considered having nondiagnostic quality. Signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) between the two groups as well as the effective radiation dose (ED) was finally assessed.
Results:
Comparative analysis considering diagnostic quality (2, 3, and 4 score) and nondiagnostic (score 0 and 1) quality demonstrated that image quality of SD 51 group is not significantly lower than that of S33 group. The noise was significantly higher in the SD 51 group than in the SD 33 group (P < 0.0001). The SNR and CNR were higher in the SD 33 group than in SD 51 group (P < 0.0001). Mean effective dose was 49% lower in the SD 51 group than in SD 33 group; indeed mean effective dose was 1.43 mSv ± 0.67 in the SD 51 group while it was 2.8 mSv ± 0.57 in the SD 33 group.
Conclusion:
Comparative analysis shows that using a 640-slice CT with a 51 SD protocol, it is possible to reduce the mean radiation dose while maintaining good diagnostic image quality.
Keywords
Coronary computed tomography angiography
image noise
image quality
radiation dose

INTRODUCTION
Coronary-computed tomography angiography (CCTA) is considered the most reliable noninvasive method for CAD assessment.[1234]
Nevertheless, the risks associated with ionizing radiation in cardiac CT have raised serious and growing concerns.[15]
All major scanner manufacturers developed different system to reduce radiation exposure as much as possible.[67]
A previous study shows that 640-slice CCTA using an electrocardiographic (ECG)-gated CCTA prospective acquisition using a prefixed target noise of 33 standard deviation (SD) is able to lower the radiation exposure up to 2.5 mSv.[2]
The aim of this study was to evaluate the effects of a scan protocol with a higher target noise (expressed as SD) on the image quality and mean radiation dose, in comparison with a scan protocol with our standard noise level threshold. We compared image quality and mean radiation dose in two groups of patients undergoing CCTA.
MATERIALS AND METHODS
Patients
A total of 268 consecutive patients, referred to our Hospital for CCTA, were prospectively scanned. The patients were divided into two groups according to the different noise level thresholds (SD) used. The experimental group was composed of 135 patients undergoing a CCTA using a noise level threshold (SD) of 51. This group was compared with a pool of patients (133 patients) scanned employing our standard noise level threshold of 33. Inclusion criteria were typical or atypical angina pectoris, dyspnea, previous uncertain or inconclusive stress test (echocardiography or nuclear), presence of multiple cardiac risk factors, and previous radiotherapy for breast cancer.[8] Exclusion criteria were glomerular filtration rate <30 ml/min/1.73 m2, pregnancy, previous allergic reactions to iodinated contrast media, heart rate (HR) higher than 65 bpm (beats per minute) after beta-blocker premedication, nonsinus atrial rhythm, and hemodynamic instability. The images were evaluated to assess the presence of significant coronary artery stenosis that was defined as a reduction in the vessel diameter of 50% or more (≥50%).
Positive cases were confirmed by coronary angiography. Discrepancies were analyzed by consensus. Nonsignificant stenosis was followed clinically after 12 months; absence of cardiovascular symptoms during the follow-up was considered as confirmation of the absence of the significant disease.
Institutional Review Board approved the study and all patients gave written informed consent before CT examination.
Acquisition protocol
All patients underwent a CCTA using a first-generation 640-slice CT scanner (Aquilion One, Toshiba Medical Systems, Otawara, Japan), with 320 row detector of 0.5 mm each, and a prospectively ECG-triggered single heartbeat acquisition protocol. Images were acquired with the following parameters: Tube voltage of 100 kV, longitudinal coverage up to 12/16 cm, rotation time of 350 ms, with the best temporal resolution of 175 ms using half-scan reconstruction. Tube current was adjusted by automatic exposure control (AEC); sure exposure three-dimensional (3D), Toshiba Medical Systems) to maintain a user-specified noise level in the image data (SD) that was 51 SD in the experimental group and 33 SD in the control group. Images were reconstructed using adaptive - iterative dose reduction) 3D. The SD is defined as the expected noise value calculated in a circular region of interest (ROI) positioned in the center of a single slice, with a body standard filter of a homogeneous phantom. ConeXact algorithm (ConeXact; Toshiba Medical Systems) performs a proprietary double slice technique obtaining up to a maximum of 640 reconstructed slices with 0.5 mm thickness and 0.25 mm interval. In order to obtain one single acquisition per beat, all patients with pre-scanning heart rate exceeding 64 bpm received beta-blocker. A 2 ml intravenous dose of beta-blocker (Metoprololo; Seloken®, AstraZeneca, Sweden) was administered every 5 min up to a maximum of 14ml, depending on heart rate and blood pressure. Patients with systolic blood pressure >100 mmHg received also 0.5 mg of isosorbide dinitrate sublingually (Carvasin®, Wyeth Lederle) before the scanning procedure, to ease the dilation of coronary arteries. 50 mL of nonionic iodinate contrast medium (Visipaque® 320; Iodinaxol 625 mg/mL) were injected into the antecubital vein at 6 mL/s, followed by 40 ml of saline flush at the same flow rate, using a dual power injector (Stellant, Medrad, Indianola, PA, USA). CT scanning was performed using a prospectively ECG-triggered single heartbeat acquisition protocol during inspiratory breath holding. CT timing acquisition was made employing the automatic bolus tracking option (SUREStart™) using a start threshold of 300 Hounsfield unit (HU). A narrow acquirable phase window (70/80% of RR cycle) was employed. The system identified automatically the phase with minimum artifacts employing auto best phase. When the images provided by the auto best phase were of poor quality, other reconstructions were made using diverse cardiac phases and selecting the best reconstruction phase.
Subjective image analysis
Subjective quality of the reconstructed images was assessed by two experienced cardiac radiologists (Ernesto Di Cesare and Alessandra Di Sibio). The readers were unaware of the technical characteristics of the specified CT data set; the images were assessed autonomously and in a random fashion. Discordant ratings were examined in consensus. The coronary arteries were divided into 15 segments according to the modified American Heart Association classification.[5]
The intermediary artery, when present, was not analyzed to avoid differences between the two groups.[5]
Each reviewer was asked to independently grade the quality of all assessable coronary artery segments using a 5-point scoring system consisting of a subjective interpretation of image quality: 0 (nondiagnostic) = poor vessel quality with excessive image noise; 1 (adequate) = seriously limited vessel wall definition and contrast resolution with severe image noise; 2 (good) = slightly limited wall definition and contrast resolution with moderate image noise; 3 (very good) = good attenuation of the vessel lumen and wall definition with minimal image noise; and 4 (excellent) = excellent attenuation of the vessel lumen and wall definition, with barely perceived image noise [Figure 1].[691011]

- (a) Right coronary artery. Scores 2 (a), 3 (b), and 4 (c) are compared.
Objective evaluation of image quality
Objective evaluation of the image quality was carried out by two reviewers using four parameters, as previously described in literature: Noise (N), signal-to-noise ratio (SNR), and contrast-to-noise ratio (CNR). Noise was defined as the SD of CT signal assessed at the level of the ascending aorta placing the largest possible ROI without including the aortic wall.[691213]
Density (V) of the proximal aorta and left main and right coronary artery was measured as the mean attenuation value (HU) within a round ROI placed in the central part of the aorta, right coronary artery, and left main coronary artery with concern to avoid the inclusion of the artery wall. CT signal of the epicardial fat (VE) was measured by placing an ROI besides the right coronary artery and left main coronary artery. SNR was calculated by dividing the density (V) of the artery (right coronary artery and left main coronary artery) by the noise (N) using the following formula: SNR = V/N. CNR was calculated by subtracting CT signal of the epicardial fat (VE) from the signal of the artery (right coronary artery and left main coronary artery; V), which was then divided by the image noise (N) using the following formula: CNR = (V-VE)/N.[214]
Estimation of effective radiation dose
For each single case, we evaluated the effective radiation dose (ED) using an approach suggested by the European Working Group for Guidelines on Quality Criteria in CT.[15] The effective radiation dose was assessed multiplying the dose length product value by an organ-weighting factor for the chest as the examined anatomical structure. This weighting factor (k = 0.014 mSv mGy-1 cm-1) is deemed to result from the most reliable data set and is balanced between female and male subjects.[15]
Statistical analysis
Continuous variables were condensed by means. SD, standard error (SE), or 95% confidence interval (CI) was used as measure of dispersion. Differences in continuous variables were analyzed by Student's t-test and mean difference, SE, and 95% CI of mean difference were reported. Differences in categorical variables were compared with Pearson's Chi-square test with Yates’ continuity correction. Fisher's exact test was used when data frequencies expected in the contingency tables were less than five. The post hoc analysis significance level was adjusted by the Bonferroni method. In order to reduce treatment selection bias and determine treatment effect, a case–control-matched propensity analysis was performed. This strategy was employed to minimize the bias related to nonrandom assignment of studied patients in the study groups.[16]
Propensity score was arranged using as covariates gender, age, weight, and BMI. A 1:1 matched analysis was performed where 1 case was matched to 1 control. For the matched analysis, differences between matched pairs were evaluated using signed rank test for continuous variables and the McNemar's test for binary data. Only patients with overlapping values of propensity score were compared and included in the final analysis. P < 0.05 were considered statistically significant. Interobserver agreement for image quality was calculated with Cohen's k statistic, which was interpreted as poor (k < 0.20), fair (k = 0.21–0.40), moderate (k = 0.41–0.60), good (k = 5 0.61–0.80), very good (k = 0.81–0.90), or excellent (k > 0.91). The SPSS® version 13.0 (IBM, Armonk, NY, USA) was used for statistical analysis and graphic presentation.[17]
RESULTS
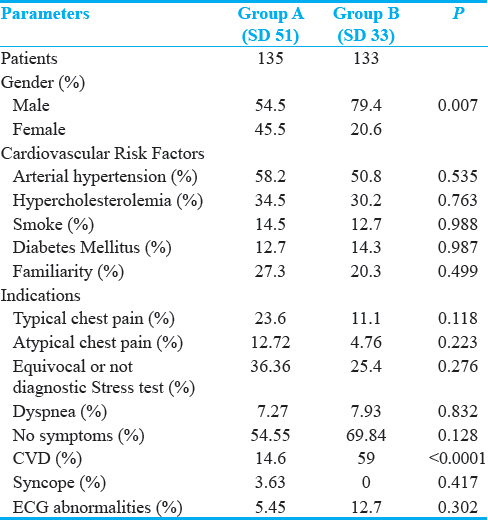
Two-hundred and sixty-eight patients were evaluated comparing 135 patients studied by means of CCTA using a noise level threshold (SD) of 51 with SD and 133 with a noise level threshold (SD) of 33. In Table 1, demographic and clinical features of the study population are summarized. There were no significant differences in age, body mass, cardiovascular risk factors, clinical presentations, scanning range, and HR between the two groups. In Group SD 51, 94 patients (69.6%) did not present significant stenosis, 21 (15.5%) had single-vessel disease, 16 (11.9%) had two-vessel disease, and 4 (3.0%) had three-vessel disease. In Group SD 33, 89 patients (66.9%) did not present significant stenosis, 25 (18.8%) had single-vessel disease, 13 (9.8%) had two-vessel disease, and 8 (6.9%) had three-vessel disease.
All positive cases were confirmed by coronary angiography. In the per-patient analysis were confirmed as significant stenosis 20 of 21 of single vessel (95.2%), 14 of 16 of two vessels (87.5%), and 4 of 4 of three-vessel disease patients (100%) in the Group SD 51. A total of 23 of 25 single-vessel patients (92%), 13 of 13 of two-vessel disease (100%), and 8 of 8 three-vessel diseases were confirmed in the Group SD 33. No significant stenosis was followed clinically after 12 months; absence of cardiovascular symptoms during the follow-up was reported as confirmation of the absence of the significant disease on all SD 33 and SD 51 patients. In the percentage of single-, double-, and triple-vessel stenosis between the two groups, no significant difference was observed at Chi-squared test for trend (P = 0.75).
Subjective evaluation of image quality
Among 4020 potentially analyzable segments, 468 segments in the SD 51 group and 457 in the SD 33 group, respectively, were deemed to be nonassessable because the segment was missing (325 and 318 segments, respectively), too small (diameter <1.5 mm; 135 and 128 segments, respectively), or entirely occluded (8 and 11 segments, respectively).
A total number of 3095 segments were finally evaluated, 1527 in the SD 51 group and 1538 in the SD 33 group. Interobserver agreement of subjective image quality was deemed as “very good” for both groups (k = 0.86 for the SD 51 group and 0.89 for the SD 33 group). In the SD 51 group, 401 segments (26.3%) were graded as 4 (= excellent), 595 segments (37.3%) as 3 (= very good), 589 segments (32%) as 2 (= good), 30 segments (2%) as 1 (= adequate), and 12 segments (0.8%) as 0 (= non-diagnostic). In the SD 33 group, 517 segments (33.6%) were graded as 4; 847 segments (55%) as 3; 134 segments (8.7%) as 2; 28 segments (1.8%) as 1; 12 segments (0.8%) as 0 [Table 2]. Segmental class analysis showed that score 2 is statistically significantly more represented in SD 51 group (P < 0.0001), while score 3 is statistically significantly more represented in SD 33 group (P < 0.0001); score 4 did not show a statistically significant difference between the two groups for the proximal (P = 0.32) and mid segments (P = 0.11). Comparative analysis considering two scoring classes, diagnostic quality (2, 3 and 4 score) and nondiagnostic (score 0 and 1) quality, demonstrated that image quality of SD 51 group was not lower than that of SD 33 group figure for the total number of segments (P = 0.20), for proximal (P = 0.78), middle (P = 0.52), and distal (P = 0.26) segmental classes [Figure 2].

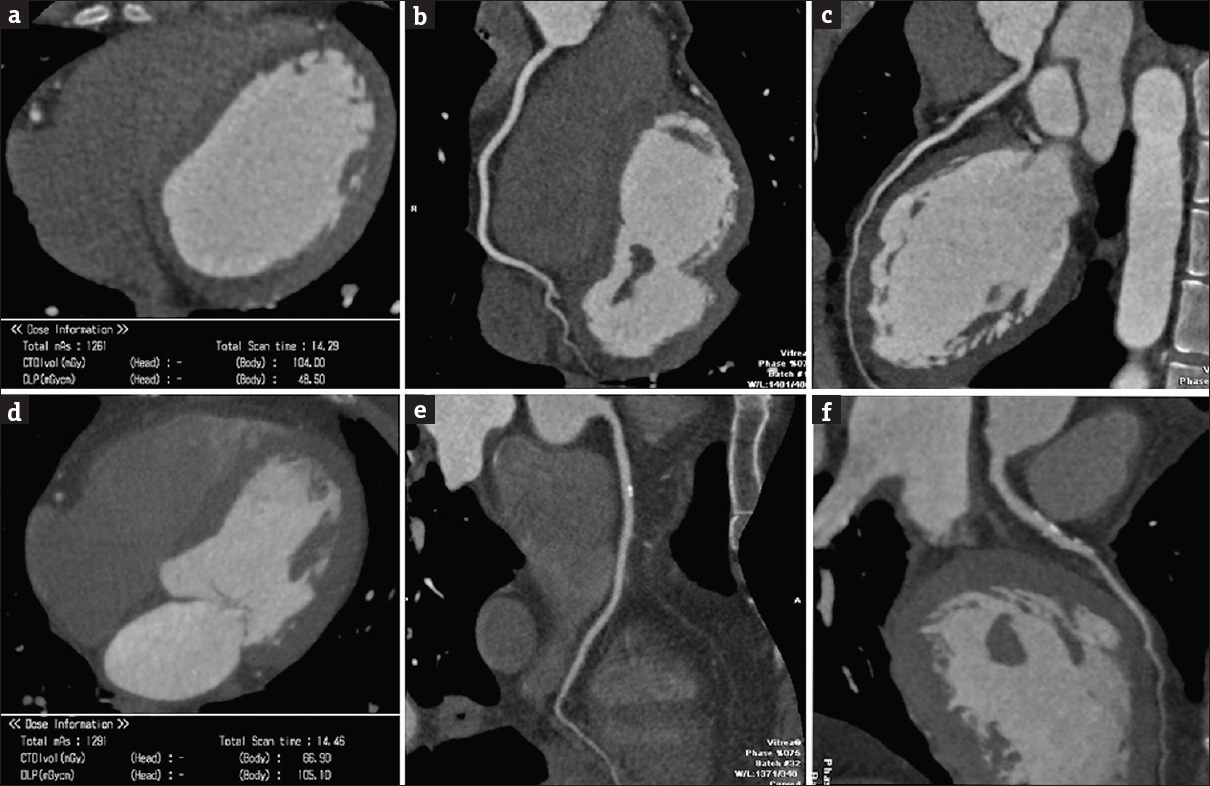
- Score 4. Comparison between SD 51 (a-c) and standard SD 33 (d-f) reformatted images at the right coronary artery (b and e) and the anterior descending coronary artery (d and f). The volume acquisition dose–length product was 154.6 in the standard acquisition (d) and 48, 5 in the SD 51 (a).
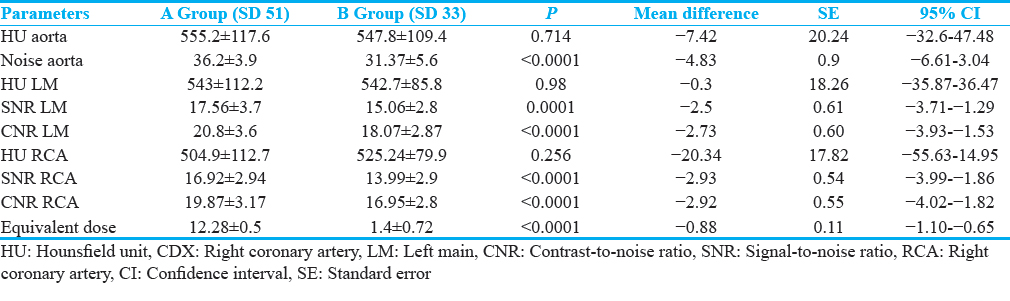
Objective evaluation of image quality
The noise was significantly higher in the SD 51 group than in the SD 33 group (P < 0.0001). SNR and CNR were significantly higher in the SD 33 group than in SD 51 group (P < 0.0001). Mean effective dose was 101 ± 12 mGy corresponding to an equivalent dose of 1.43 mSv ± 0.67 in the SD 51 group, while a mean dose of 200 ± 16 mGy was corresponding to an equivalent dose of 2.8 mSv ± 0.51 in the SD 33 group. The mean effective dose was therefore 49% lower in the SD 51 group than in SD 33 group, representing a statistically significant difference (P < 0.0001) [Table 3].
DISCUSSION
CCTA is rated as appropriate for ambiguous cases (atypical angina, discordant noninvasive stress test results, inconclusive or unfeasible noninvasive stress tests) but, considering costs and risks, not in asymptomatic patients.[41819]
Previous studies using 64–128 slice CT scanners and retrospective ECG gating[15] reported a mean effective dose of about 8–10 ms. This dosimetric data lead to a broad debate about the appropriateness of CCTA based on radiation-related cancer risks. Indeed, Food and Drugs Administration estimates a 1:2000 risk of cancer per exposition higher than 10 mSv. Until now, the use of CCTA was limited to symptomatic cases, also because the mean radiation exposure during a diagnostic coronary catheterization did not exceed 7–9 mSv.[20]
The newest CT scanners can cover the whole heart within one heartbeat. Using an ECG prospective gating, an AEC system, and an iterative reconstruction, they are able to deliver radiation doses lower than those delivered by coronary catheterization, without the risks of the latter diagnostic tool.[221]
In our experience, we considered two groups of patients with no significant differences in age, body mass, cardiovascular risk factors, clinical presentations, scanning range, and HR.
The mean equivalent dose in the standard technique (SD 33) group was 2.8 mSv ± 0.51 corresponding to an absorbed mean dose of 200 ± 16 mGy. These data show that CCTA may have a minimal radiation-related risk and, thus, support a broader use of CCTA. However, radiation-related cancer risks increase with increasing radiation exposure and a radiation dose as low as reasonably achievable is mandatory. The international commission on radiological protection reported that a radiation exposure inferior to 100 mGy does not have the potential to damage cellular structures.[2223]
A 100 mGy absorbed dose corresponds to a 1.4 mSv equivalent dose calculated using the mean adsorbed dose and multiplied by the radiation weighting factor of 0.014. Indeed, an equivalent dose of 1.4 mSv is reasonably deemed as devoid of the potential to damage cellular structures. Therefore, we evaluated the quality (objective and subjective) of CT images obtained by an equivalent dose close to 1.40 mSv. We established a noise level threshold (expressed as SD) higher than the one usually employed in our institution (33 SD). A 640-slice CCTA using a 51 SD protocol delivers, in fact, a 1.43 mSv ± 0.67 equivalent dose, which corresponds to about 100 mGy mean absorbed dose. The images obtained by the 51 SD protocol show more noise due to this lower dose. Therefore, SNR and CNR were higher in the SD 33 group, but the mean attenuation value (HU) of the proximal coronary artery was similar between the two groups. Indeed, the images in the SD 51 group were more noisy than SD 33 group, still showing a good quality. In fact, the subjective evaluation of image quality did not show a statistically significant difference between the two groups considering the score 0 and 1 for proximal, middle, and distal segmental classes and for the total number of segments. Furthermore, score 4 did not show a statistically significant difference between the two groups for the proximal (P = 0.32) and mid segments (P = 0.11). Nevertheless, score 4 is so much more represented in SD 33 group for distal segments to have a statistically significant difference between the two groups for the total number of segments. This can be explained by the fact that the higher noise in the experimental group may limit wall definition, especially in the small caliber vessels. Score 2 is more represented in the experimental group, while score 3 is more represented in SD 33 group but segments evaluated as score 2 and 3 have both diagnostic quality, with score 2 segments showing good quality and score 3 segments presenting very good quality. Comparative analysis considering two scoring classes, diagnostic quality (2, 3 and 4 score) and not diagnostic (score 0 and 1) quality, demonstrated that image quality of SD 51 group is not lower than the one of SD 33 group. It is worth mentioning that in our study most patients had no significant stenosis (69.6% in the SD 51 group and 66.9% in the SD 33 group). However, the aim of our study was the qualitative evaluation of the images obtained by low- and very-low radiation dose protocol. Our data showed that subjective image quality of SD 51 group was not significantly lower than that of SD 33 group although quantitative noise was higher in the SD 51 group. These data are interesting also considering that the mean radiation dose in the SD 51 group is reasonably deemed as devoid of the potential to damage cellular structures. For all these reasons, we consider that the experimental (SD 51) protocol may be suggested to spare dose, maintaining adequate quality, in many clinical situations with emphasis on cases of symptomatic patient with low pretest probability such as young people with atypical angina or when the ECG stress test is inconclusive or in the preoperative noncardiac CCTA assessment. This sentence may be supported by the very high negative predictive value previously reported up to 99% by CCTA.[418]
CONCLUSION
Using a 640-slice CT with an ECG prospective gating and a 51 SD protocol, it is possible to deliver mean radiation doses that are reasonably deemed as without radiation-related risks, while keeping the diagnostic image quality at a clinically acceptable level, suggesting an appropriate role in low pretest probability patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/52/245530
REFERENCES
- Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298:317-23.
- [Google Scholar]
- Assessment of dose exposure and image quality in coronary angiography performed by 640-slice CT: A comparison between adaptive iterative and filtered back-projection algorithm by propensity analysis. Radiol Med. 2014;119:642-9.
- [Google Scholar]
- Executive summary: Heart disease and stroke statistics–2010 update: A report from the American Heart Association. Circulation. 2010;121:948-54.
- [Google Scholar]
- Clinical indications for cardiac computed tomography. From the working group of the cardiac radiology section of the Italian Society of Medical Radiology (SIRM) Radiol Med. 2012;117:901-38.
- [Google Scholar]
- Image quality and radiation dose of single heartbeat 640-slice coronary CT angiography: A comparison between patients with chronic atrial fibrillation and subjects in normal sinus rhythm by propensity analysis. Eur J Radiol. 2015;84:631-6.
- [Google Scholar]
- Adaptive statistical iterative reconstruction: Assessment of image noise and image quality in coronary CT angiography. AJR Am J Roentgenol. 2010;195:649-54.
- [Google Scholar]
- Iterative reconstruction for coronary CT angiography: Finding its way. Int J Cardiovasc Imaging. 2012;28:613-20.
- [Google Scholar]
- Breast cancer radiotherapy and coronary artery stenosis: Location, location, location. J Clin Oncol. 2012;30:350-2.
- [Google Scholar]
- Iterative reconstruction in image space (IRIS) in cardiac computed tomography: Initial experience. Int J Cardiovasc Imaging. 2011;27:1081-7.
- [Google Scholar]
- Radiation dose modulation techniques in the multidetector CT era: From basics to practice. Radiographics. 2008;28:1451-9.
- [Google Scholar]
- Iterative reconstruction of dual-source coronary CT angiography: Assessment of image quality and radiation dose. Int J Cardiovasc Imaging. 2012;28:1775-86.
- [Google Scholar]
- Image quality of adaptive iterative dose reduction 3D of coronary CT angiography of 640-slice CT: Comparison with filtered back-projection. Int J Cardiovasc Imaging. 2013;29:669-76.
- [Google Scholar]
- Iterative reconstruction technique for reducing body radiation dose at CT: Feasibility study. AJR Am J Roentgenol. 2009;193:764-71.
- [Google Scholar]
- Effects of nitroglycerin on the diagnostic accuracy of electrocardiogram-gated coronary computed tomography angiography. J Comput Assist Tomogr. 2008;32:86-92.
- [Google Scholar]
- European Guidelines for multislice Computed Tomography: Appendix C. Funded by the European Commission. Brussels, Belgium: European Commission; 2004.
- [Google Scholar]
- Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757-63.
- [Google Scholar]
- ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864-94.
- [Google Scholar]
- Improvement and problems in appropriate use of cardiac CT: 2003, 2007 and 2011 use of CT-based on ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac CT. Int J Cardiol. 2014;174:385-8.
- [Google Scholar]
- Radiation exposure during cardiac catheterisation is similar for both femoral and radial approaches. Heart Lung Circ. 2015;24:264-9.
- [Google Scholar]
- 320-row coronary computed tomography angiography (CCTA) with automatic exposure control (AEC): Effect of 100 kV versus 120 kV on image quality and dose exposure. Radiol Med. 2016;121:618-25.
- [Google Scholar]
- Clinical indications for the use of cardiac MRI. By the SIRM study group on cardiac imaging. Radiol Med. 2013;118:752-98.
- [Google Scholar]






