Translate this page into:
Isolated Tuberculous Tenosynovitis of the Anterior Tibial and Extensor Digitorum Longus Tendons
Address for correspondence: Dr. Berhan Genç, Department of Radiology, Şifa University School of Medicine, 35240 İzmir, Türkiye. E-mail: be.genc@hotmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Musculoskeletal system is involved in 1-5% of extrapulmonary cases of tuberculosis. Tuberculous tenosynovitis is a rare form of musculoskeletal tuberculosis. Tuberculosis of the tendon sheath in the hand has been seen in a few cases. Involvement of the tendons of the leg is less common. Diagnosis is not easy as there are no specific clinical symptoms or signs. A 33-year-old male presented with painful swelling in the distal right lower limb that caused restriction of movement. Imaging studies showed inflammation and infection of the extensor digitorium longus and tibialis anterior tendons. Histopathological studies showed a necrotizing granulomatous inflammation in the synovial tissue. A diagnosis of tuberculosis was made and medical treatment was initiated that proved successful. Patient remained infection-free at 26-month follow-up examination.
Keywords
Foot
tenosynovitis
tuberculosis

[SHOW_RELATED_PUBMED_ARTICLES]
INTRODUCTION

Musculoskeletal system is responsible for 1-5% of extrapulmonary tuberculosis (TB) involvement.[1] Although tendon involvement is a rare complication of TB, it continues to be a major cause of chronic tendon sheath infection.[2] Although TB tenosynovitis is rare, it is mostly encountered as hand or wrist involvement. Foot tendon involvement is very rare, with only a few cases having been reported so far.
A 33-year-old man working in a courier company presented with a 4-year history of progressive painful swelling located distal to cruris in the right ankle. Pain had intensified during walking and climbing stairs. He had no history of a recent illness, fever, or trauma. Physical examination did not reveal any abnormality but showed a swollen right ankle. The swelling was not tender; its size was 13 × 7 cm, stretching from the distal end of cruris to the ankle. He had no history of chronic illness, rheumatic disease, diabetes mellitus, or any surgery. He had been treated by many physicians with non-steroidal anti-inflammatory drugs prior to presenting to our facility.
Laboratory tests revealed an erythrocyte sedimentation rate (ESR) of 30 mm/h and a C-reactive protein (CRP) of 4.4 mg/dl. Mountaux test was positive. Complete blood count was normal. Radiographic examinations of cruris and lungs were in normal limits.
RADIOLOGIC FEATURES
On ultrasonography (USG), thickening and decreased echogenicity of extensor digitorum longus and tibialis anterior tendons as well as minimal fluid collection around tendon sheath were observed. Coronal T1-weighted image with gadolinium enhancement showed tenosynovitis in the distal portion of the lower limb [Figure 1a and b]. Axial T1-weighted images at the level of the right tibiotalar joint demonstrated contrast enhancement of the extensor digitorum longus and tibialis anterior tendons surrounding the smooth tissue. The extensor hallucis longus tendon was normal [Figure 2a and b]. Axial fat-suppressed T2-weighted MR image at the level of the right tibiotalar joint showed thickening of the extensor digitorum longus and tibialis anterior tendons, peritendinous edema and minimal fluid within the synovial sheath, edema in the surrounding subcutaneous tissues with loss of fat planes, and increased signal intensity within the tendons [Figure 3].
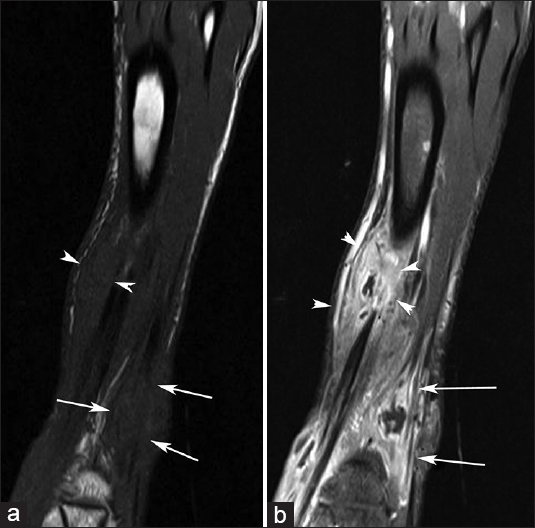
- 33-year-old man with painful swelling in the right ankle diagnosed with tuberculous tenosynovitis. (a) Pre-contrast and (b) post-contrast coronal T1-weighted images with gadolinium enhancement show tenosynovitis in the distal portion of the lower limb – thickening of the extensor digitorum longus (white arrows) and anterior tibial (arrow heads) tendons.
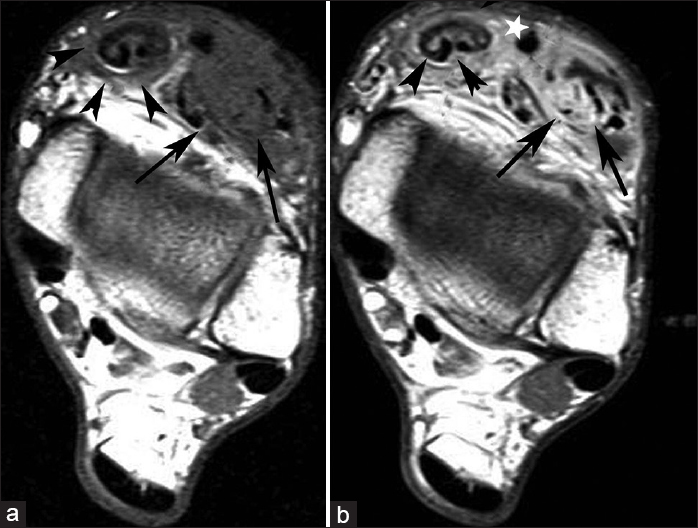
- 33-year-old man with painful swelling in the right ankle diagnosed with tuberculous tenosynovitis. (a) Pre-contrast and (b) post-contrast Axial T1-weighted images at the level of the right tibiotalar joint demonstrate contrast enhancement of the extensor digitorum longus (black arrows) and tibialis anterior tendons (arrow heads) and surrounding smooth tissue. The extensor hallucis longus tendon is normal (white star).
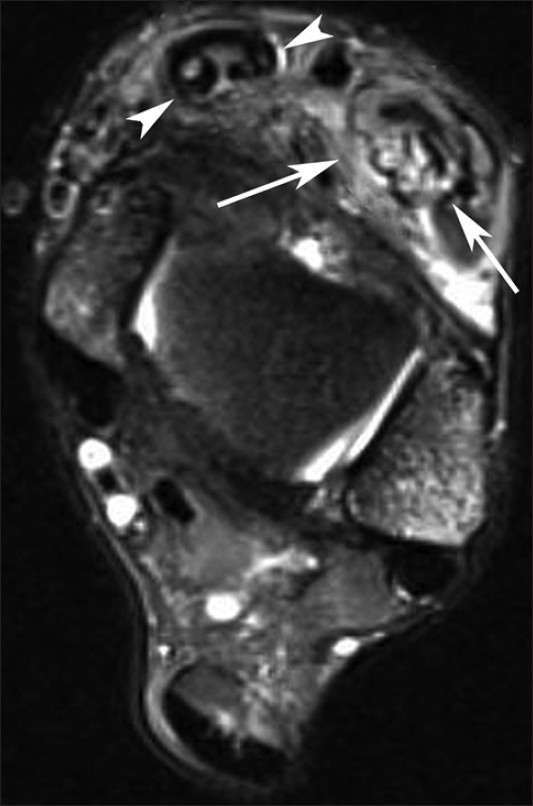
- 33-year-old man with painful swelling in the right ankle diagnosed with tuberculous tenosynovitis. Axial fat-suppressed T2-weighted MR images at the level of the right tibiotalar joint shows thickening of the extensor digitorum longus (arrows) and tibialis anterior tendons (arrow heads), peritendinous edema and minimal fluid within the synovial sheath, edema in the surrounding subcutaneous tissues with loss of fat planes and increased signal intensity within the tendons.
Post-contrast images showed moderate contrast uptake in the tendons in question and the surrounding synovial membrane, supporting the diagnosis of synovitis and inflammation. Peritendinous soft tissue showed marked homogenous contrast uptake. Magnetic resonance imaging (MRI) showed thickening of extensor digitorum longus and tibialis anterior tendons, increased vascularization, minimal fluid accumulation in tendon sheath, and signs of reactive inflammation around the tendon.
PATHOLOGIC FEATURES
A tru-cut needle biopsy was performed. The biopsy specimens were sent for histological examination, and for aerobic, anaerobic, acid-fast bacilli, and gram staining. However, no bacteria were detected by Gram stain. Necrotizing, granulomatous inflammation was observed upon histopathological examination of the synovium using hematoxylin-eosin stain [Figure 4]. Based on the findings of the histopathological examination, anti-TB treatment was started. Mycobacterium tuberculosis was isolated on Lowenstein-Jensen culture media after seven weeks. The patient received anti-TB therapy for 9 months, which included pyrazinamide (1500 mg) and ethambutol (1000 mg) for the first 3 months, and rifampicin (600 mg) and isoniazide (300 mg) for the entire treatment period of 9 months. At the end of the treatment, he was asymptomatic and had a full range of motion in his right ankle and lower limb. No recurrence was detected at intermittent and at 26-month follow-ups.
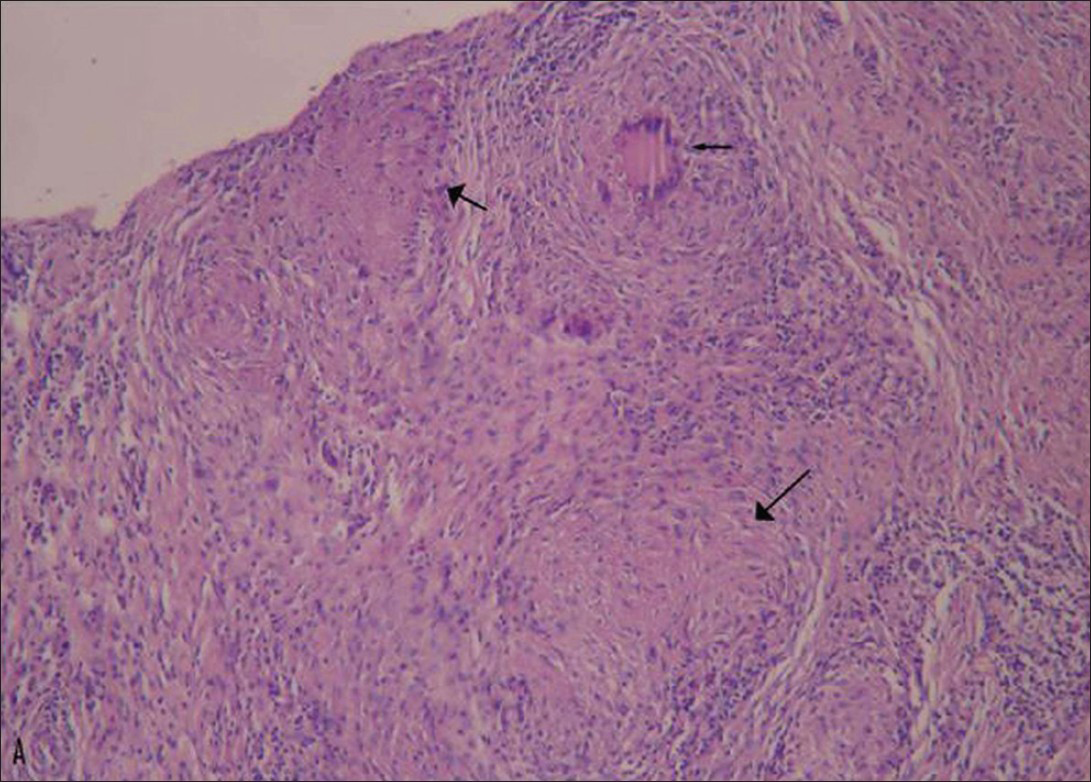
- 33-year-old man with painful swelling in the right ankle diagnosed with tuberculous tenosynovitis. Photomicrograph of a histopathological section of the synovium stained with hematoxylin-eosin (×100) shows casseous necrosis with granuloma formation (black arrow), typical of tuberculosis infection.
DISCUSSION
Extra-pulmonary TB originates from hematogenous spread of active or inactive bacilli in lymphatics or other visceral organs. The disease can start with a slowly-growing swelling in the involved tendon. Erythema, pain, and limitation in joint movements may be seen. Laboratory examinations may be in normal limits except for increased ESR and CRP levels.
The most striking feature of the disease is the long period between disease onset and diagnosis due to subtle clinical signs and symptoms. Although tuberculin test is positive in majority of the cases, X-ray is normal in 50% of cases[2] The characteristic feature of the disease is minimal fluid accumulation in the synovial sheath together with synovial thickening. However, a marked increase in synovial sheath fluid is observed in acute suppurative tenosynovitis compared to TB synovitis.
Synovial thickening is due to the presence of granular tissue in the synovial sheath. “Rice bodies” or “Melon seeds” are fibrinous masses (tubercles) seen mostly in atypical TB synovitis and are present in 50% of tuberculosis cases. These nodules are macroscopically similar to the polished white rice and they contain an inner morphous core of acidophilic material and a surrounding layer composed of collagen and fibrin. Rice bodies can be seen by USG during surgery. However, rice bodies may also be present in patients with rheumatoid arthritis, seronegative inflammatory arthritides, and synovial chondromatosis.[34]
Clinical and imaging properties of TBC tenosynovitis depend on the disease duration, immunity of the host, and virulence of the organism. The typical histopathology of TBC synovitis include caseous granulomas surrounded by epithelioid histiocytes and multinucleated giant cells. The tissue infected by mycobacterium (typical or atypical TBC) usually does not give a positive reaction with Ziehl-Nielsen stain. The anti-tuberculous therapy usually begins empirically, based on radiological, clinical, and histopathological findings, as in our case[56] because it takes many months for the culture results to confirm the presence of tuberculosis bacilli.
Imaging modalities play an important role in the detection of TBC tenosynovitis. The USG is used as an initial step for diagnosis. It shows tendon thickening and fluid within tendon sheath. The MRI is a useful modality to assess tendon and its sheath. This method can show thickening in synovial membrane with increased vascularization, fluid in the sheath, active inflammation around the tendon, and thickening in the tendon. Although synovial sheath fluid is markedly increased in acute suppurative tenosynovitis, a minimal amount of synovial fluid is encountered in TB tenosynovitis. Rice bodies are visible both on USG and MRI; however, very small Rice bodies may be missed with USG. Rice bodies of small size may be seen with MRI. Rice bodies are isointense on T1 weighted MR imaging and relatively hyperintense compared with muscle tissue on T2-weighted images.[56] Computed tomography is not used for primary diagnosis of tuberculous tenosynovitis; however, it is useful in demonstrating tuberculous tenosynovitis-associated destructive bone changes.
Although there are few reports on this topic, cases of TB tenosynovitis originating from flexor digitorum longus, posterior tibial, and Achilles tendons have been reported.[34567] Pimm and Waugh examined a total of 44 cases; 52 lesions with tenosynovitis were detected and only 3 of these lesions had lower extremity involvement.[8] Surgical debridement in the treatment of TB tenosynovitis is debated. Some authors have recommended debridement of the surrounding tissue and decompression of the tendon sheath without excision.[4] Tuli recommended surgical debridement in cases unresponsive to treatment for 4-5 months.[9] In our case, we planned to perform surgical debridement after anti-TB treatment because medical therapy prior to surgical treatment prevents miliary dissemination and/or meningeal TB.
Prior to anti-TB therapy, most infections used to be treated by extensive surgical therapy including complete sinoviectomy and excision of surrounding tissue. To reduce the size of the lesion to an extent, anti-TB chemotherapy should begin after the diagnosis of TB is made before a more extensive surgical intervention is performed.[10] Total or subtotal snoviectomy may be necessary in the management of TB tenosynovitis unresponsive to treatment.[9]
Our patient presented with painful swelling in the lower extremity. He had no history of TB or constitutional symptoms. A long interval had elapsed between onset of symptoms and diagnosis of TB with ultrasonography, MRI and culture and histopathologic examination. He was treated with anti-tuberculosis therapy for 9 months. Although TB is a very rare cause of tenosynovitis in the foot, it should be considered in differential diagnosis of chronic or recurrent tenosynovitis. Differential diagnosis of TB tenosynovitis should include rheumatoid arthritis, pyogenic infection, gout arthritis, giant cell tumor of tendon sheath, and fungal tenosynovitis.
CONCLUSION
Tuberculosis lesions can have atypical localizations. TB should necessarily be considered in cases of slowly developing tenosynovitis. MRI plays a useful role in identifying cases of tenosynovitis. MR scans show thickening of the tendon sheath and presence of reduced synovial fluid in the sheath. Histopathological findings of granulomatous inflammation and culture tests confirm the diagnosis. Although TB is not a common cause of tenosynovitis in the foot, it should be considered in the differential diagnosis of chronic tenosynovitis in countries where the prevalence of TB is high. Anti-tuberculosis therapy should be started before surgical therapy. Surgical debridement can be employed when cases of TB tenosynovitis are unresponsive to medical therapy.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/37/119015
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Granulomatous tenosynovitis: A rare musculoskeletal manifestation of tuberculosis. Clin Rheumatol. 1998;17:166-9.
- [Google Scholar]
- Isolated tuberculous tenosynovitis of the Achilles tendon: A report of two cases. Acta Orthop Traumatol Turc. 2007;41:314-20.
- [Google Scholar]
- Tibialis posterior tenosynovitis and associated pesplano valgus in rheumatoid arthritis: EMG, multi-segment foot kinematics and ultrasound features. Arthritis Care Res (Hoboken). 2013;65:495-502.
- [Google Scholar]
- Atypical mycobacterial tenosynovitis and bursitis of the wrist. Diagn Interv Radiol. 2009;15:266-8.
- [Google Scholar]
- Rice-body formation in atypical mycobacterial tenosynovitis and bursitis: Findings on sonography and MR imaging. AJR Am J Roentgenol. 2003;180:1455-9.
- [Google Scholar]
- Tuberculous tenosynovitis of flexor digitorum longus tendon. Orthopedics. 2008;31:499.
- [Google Scholar]
- General principles of osteoarticular tuberculosis. Clin Orthop Relat Res. 2002;398:11-9.
- [Google Scholar]
- Treatment algorithm in synovial tuberculosis of the hand and wrist: A report of three cases. Acta Orthop Traumatol Turc. 2006;40:255-9.
- [Google Scholar]





