Hyperdense Endobronchial Mass - A Rare Manifestation of Metastatic Melanoma
Address for correspondence: Dr. Chul Y Chung, Department of Radiology, Baylor College of Medicine, One Baylor Plaza, BCM MS: 360, Houston, Texas - 77030, USA. E-mail: Chris.Young.Chung@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Parenchymal lung metastases are common in malignant melanoma. However, endobronchial metastatic melanoma is uncommon. In this report, we describe a patient with a hyperdense endobronchial mass diagnosed as a melanoma metastasis. We review the imaging findings of pulmonary metastatic melanoma and discuss the differential diagnosis of an endobronchial mass in adults.
Keywords
Endobronchial
melanoma
metastasis
multidetector computed tomography
INTRODUCTION

Parenchymal lung metastases are common in malignant melanoma with various documented manifestations on computed tomography (CT). We report an uncommon case of a hyperdense endobronchial metastasis from melanoma and discuss the differential diagnosis for an endobronchial mass in an adult.
CASE REPORT
A 57-year-old man with a history of right lower extremity cutaneous melanoma, who had undergone first and second toe amputation 3-years prior, presented with dyspnea and black-colored sputum. Chest radiograph revealed a collapsed left lung, pathologic fracture of the left sixth rib, and a destructive mass involving the right posterior fifth rib [Figure 1]. Non-Enhanced CT (NECT) of the chest showed a hyperdense mass with a mean density of 56 Hounsfield units within the left main bronchus, resulting in postobstructive left lower lobe collapse [Figure 2a and b]. In addition, there were two hyperdense left lower lobe intraparenchymal masses, one of which was lobulated [Figure 2c]. There were also lytic bone lesions in the right scapula (not shown) and thoracic vertebrae [Figure 2d]. Contrast-enhanced CT (CECT) through the lower chest demonstrated heterogeneous enhancement of the left lower lobe masses [Figure 3]. Bronchoscopy revealed a black-colored hemorrhagic endobronchial mass that was confirmed on histopathology to be an endobronchial metastasis from melanoma [Figure 4]. The patient was treated with imatinib (Gleevec) (Novartis Pharmaceuticals, East Hanover, NJ, USA).
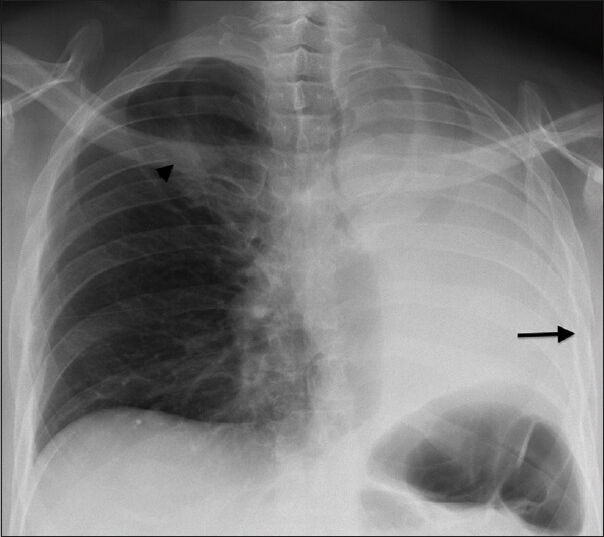
- 57-year-old man presenting with dyspnea and black-colored sputum diagnosed with endobronchial metastasis from melanoma. Posteroanterior chest radiograph demonstrates complete collapse of left lung, pathologic fracture of left sixth rib (arrow), and destructive mass (arrowhead) involving the right posterior fifth rib.
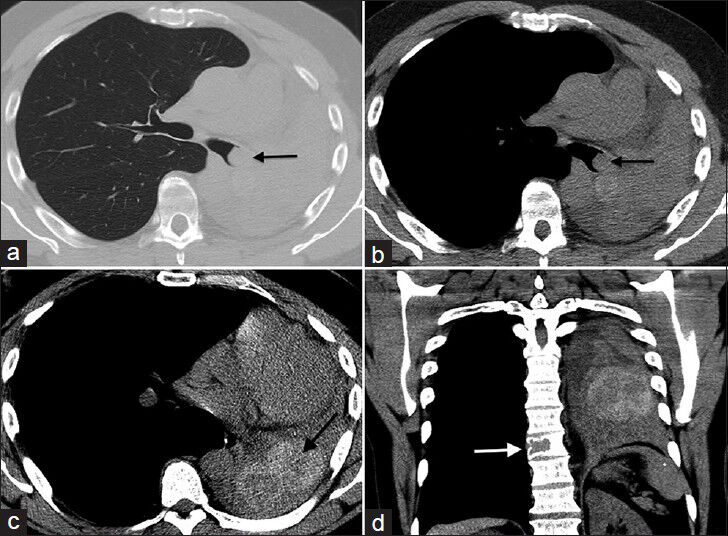
- 57-year-old man presenting with dyspnea and black-colored sputum diagnosed with endobronchial metastasis from melanoma. Non-enhanced CT of the chest. Axial CT images at a mid level in the chest in (a) lung window and (b) soft tissue window show a hyperdense mass (arrow) in the left main bronchus with postobstructive collapse and leftward mediastinal shift. (c) Axial CT image of a lower level in the chest demonstrates an additional hyperdense lobulated left lower lobe mass (arrow). (d) Coronal CT image shows a lytic lesion in a thoracic vertebra (arrow).
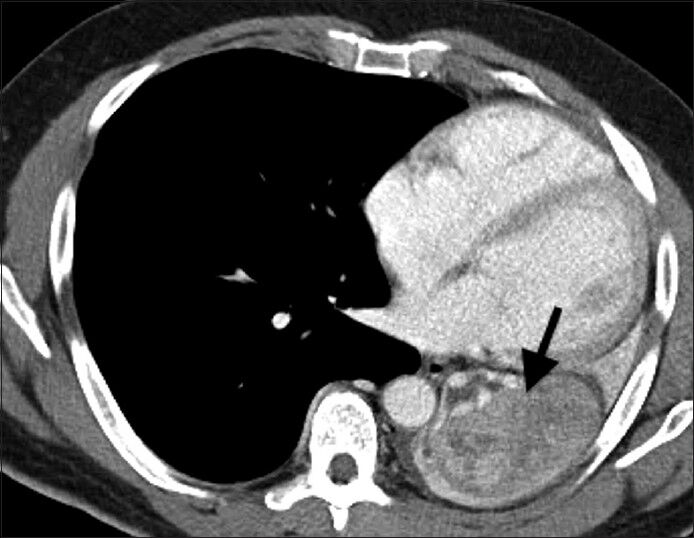
- 57-year-old man presenting with dyspnea and black-colored sputum diagnosed with endobronchial metastasis from melanoma. Contrast-enhanced axial CT image through the lower chest demonstrates heterogeneous enhancement of the left lower lobe mass (arrow).
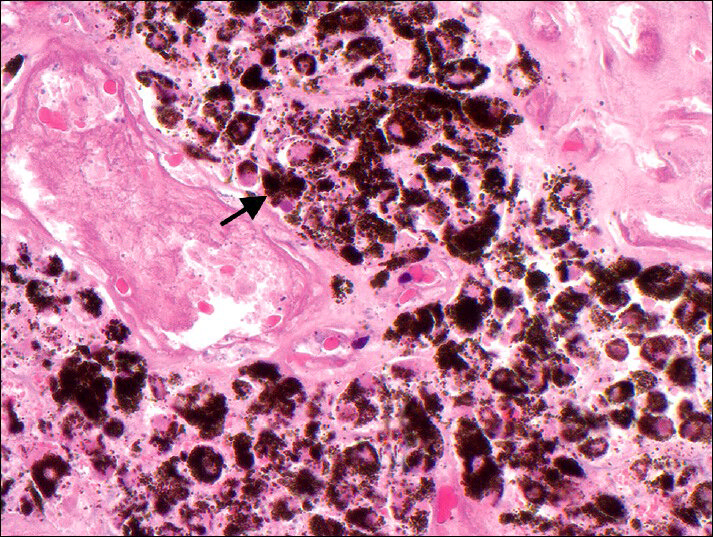
- 57-year-old man presenting with dyspnea and black-colored sputum diagnosed with endobronchial metastasis from melanoma. Microscopic findings: Staining of endobronchial biopsy specimen with hematoxylin and eosin shows pigment-laden cells, indicative of metastatic melanoma (×400).
DISCUSSION
Metastatic melanoma involves the lungs in up to 71% of cases and the thorax is the most common site of disease relapse.[1] CT findings of metastatic melanoma to the lungs include pulmonary nodules (occasionally in a miliary pattern), feeding vessels associated with hematogenous lung metastases, postobstructive atelectasis, and hilar/mediastinal lymphadenopathy.[1] Endobronchial metastasis from melanoma is uncommon and not well-documented.[1] In an autopsy series of 21 cases of pulmonary metastatic melanoma, only two cases showed endobronchial involvement.[2] Primary melanoma of the bronchus is a rare diagnosis of exclusion if no primary site of melanoma is identified.[3] The presence of known cutaneous melanoma and multiplicity of findings in this case make metastatic melanoma the likely diagnosis, rather than primary melanoma of the bronchus. The high attenuation of melanoma metastases on NECT in this case is likely secondary to the hemorrhagic nature of the masses. Similarly, direct correlation has been shown between the degree of hemorrhage within an intracranial melanoma metastasis and its hyperdensity on NECT.[4]
Staging work-up of metastatic melanoma includes brain magnetic resonance imaging and either CECT or positron emission tomography (PET)-CT of the chest, abdomen, and pelvis. PET-CT is more sensitive (86%) and specific (91%) than CECT (63% sensitivity and 78% specificity) in detecting melanoma metastases; however, due to the relatively reduced availability of PET imaging, CECT is often the study of choice.[1] Preoperative lymphoscintigraphy is performed to identify regional lymph node drainage, in order to help plan a thorough lymph nodal dissection. The postoperative lymphadenectomy site may be followed up with ultrasonography to evaluate for local recurrence.[1]
About 2% of endobronchial masses represent endobronchial metastasis.[5] Endobronchial metastasis from an extrapulmonary malignancy is uncommon. Breast, colorectal, and renal cancers are the more likely extrapulmonary malignancies, while sarcoma, melanoma, and head and neck cancers are less likely malignancies.[5] Endobronchial metastasis is diagnosed on average 4 years after the initial cancer diagnosis. In our patient, this time interval was 3 ½ years.[5]
Imaging findings of an endobronchial mass are nonspecific; therefore, bronchoscopy and biopsy are required for further characterization.[2] Primary bronchogenic carcinoma, particularly squamous cell carcinoma, is the most common cause of an endobronchial mass in an adult, but a comprehensive differential diagnosis includes carcinoid, allergic bronchopulmonary aspergillosis (ABPA), lymphoma, and metastasis.[6789] Pulmonary carcinoid represents 1-5% of all lung cancers and often displays an endobronchial growth pattern; up to 92% of pulmonary carcinoid are centrally located.[7] On CT, carcinoid appears as a well-defined ovoid endobronchial nodule with punctate or diffuse calcifications, and demonstrates homogenous enhancement.[7] ABPA is seen more commonly in young patients with a history of chronic asthma or cystic fibrosis. Hyperdense tubular branching opacities and central bronchiectasis in the upper lobes on CT are pathognomonic of ABPA.[8] Lymphoma may present as an endobronchial mass, which occurs in 2% of Hodgkin's lymphoma cases and in 1.8% of non-Hodgkin's lymphoma cases.[1910] Mass-like consolidations and multiple pulmonary nodules may be seen on CT in patients with lymphoma.[910]
CONCLUSION
Although metastatic melanoma frequently involves the lungs, endobronchial metastases are uncommon. The differential diagnosis for an endobronchial mass in an adult includes primary bronchogenic carcinoma, carcinoid, allergic bronchopulmonary aspergillosis, lymphoma, and metastases (particularly from breast, colorectal, and renal cell carcinoma). Metastatic melanoma should be considered if an endobronchial or parenchymal mass is hyperdense on nonenhanced CT.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/7/127833
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Multimethod imaging, staging, and spectrum of manifestations of metastatic melanoma. Clin Radiol. 2011;66:224-36.
- [Google Scholar]
- Cranial computed tomography of malignant melanoma. AJR Am J Roentgenol. 1981;136:145-9.
- [Google Scholar]
- Endobronchial metastases: A clinicopathological analysis. Respirology. 2005;10:510-4.
- [Google Scholar]
- Bronchogenic carcinoma. A study of 109 cases. J Assoc Physicians India. 1989;37:379-82.
- [Google Scholar]
- Clinico-pathologic study of pulmonary carcinoid tumours: A retrospective analysis and review of literature. Respir Med. 2008;102:1611-4.
- [Google Scholar]
- Spectrum of pulmonary aspergillosis: Histologic, clinical, and radiologic findings. Radiographics. 2001;21:825-37.
- [Google Scholar]
- Non-Hodgkin's lymphoma presenting as an endobronchial tumor: Report of eight cases and literature review. Am J Hematol. 2008;83:416-9.
- [Google Scholar]
- Endobronchial presentation of Hodgkin's disease: A report of nine cases and review of the literature. Eur Respir J. 1994;7:1852-5.
- [Google Scholar]






