Translate this page into:
Feasibility of Computed Tomography Pulmonary Angiography with Low Flow Rates
Address for correspondence: Dr. J. Gossner, Department of Clinical Radiology, Evangelisches Krankenhaus Göttingen- Weende, An der Lutter 24, Göttingen, Germany. E-mail: johannesgossner@gmx.de
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Computed tomography pulmonary angiography (CTPA) is the imaging test of choice in suspected pulmonary embolism. High flow rates for the administration of contrast medium are recommended, but these cannot be achieved in a number of patients due to poor peripheral venous access or when using certain central venous catheters. This small feasibility study has examined the CTPA data in a set of 22 patients in whom contrast medium was given at low flow rates (2.0 or 2.5 mL/s). Subjectively, all but one of the patients was judged to be diagnostic. Objectively, enhancement values ≥200 HU were reached in 92% of the examined central vessels (pulmonary trunk, main pulmonary arteries, and lobar arteries). In conclusion, even with a low injection rate CTPA is of diagnostic value in most patients.
Keywords
Computed tomography
contrast media
flow rate
pulmonary angiography
INTRODUCTION

Pulmonary embolism (PE) is a common disease entity that may present with a variety of symptoms ranging from mild dyspnea to cardiogenic shock. In patients with suspected PE, prompt investigation is mandatory, in order to facilitate adequate management.[1] Computed tomography pulmonary arteriography (CTPA) using multi-detector row scanners is the preferred imaging test and is an integral part of diagnostic algorithms and guidelines.[23] For optimal arterial enhancement, high flow rates of contrast media are recommended that use a large bore and proximally placed intravenous cannula. For example, a flow rate of 4 mL/s is achieved through an 18 G cannula in a vein of the antecubital fossa.[3] However, these high flow rates cannot be achieved in patients with poor peripheral venous status or fine bore central venous access. It appears unclear from published literature whether contrast enhancement and diagnostic quality may be acceptable when contrast medium is administered at low flow rates.
MATERIALS AND METHODS
The CTPA data in 22 patients (11 females, mean age 65.4 years) in whom only small bore intravenous cannulas (20 or 22 G) could be placed at the mid-forearm level or distal to this, due to poor venous access, were evaluated. All had undergone CTPA in accordance with the current guidelines for diagnosis of pulmonary embolism. Written informed consent was obtained from all. The cases presenting between July and August 2010 were prospectively included in this study. Contrast medium was administered at rates of 2.0 and 2.5 mL/s, using 60 mL of 350 mg/mL iodinated contrast medium (Imeron, Bracco Imaging, Konstanz, Germany), followed by a 20 mL bolus of physiological saline solution. The acquisition was triggered when a threshold of 90 HU was reached in the pulmonary trunk. Scan parameters were 120 kVp, automatic exposure control, 1 mm slice thickness, using a 16-slice CT-scanner (Activion®, Toshiba Medical Systems, Tokyo, Japan). Data sets were post-processed on a standard medical workstation (Vitrea 2, Vital Images, Minnetoka, U.S.A.).
A single consultant radiologist conducted an initial subjective assessment of the scans and recorded the findings. Scans that showed adequate opacification of the pulmonary arteries were considered diagnostic. Pulmonary arterial enhancement was then evaluated on the primarily reconstructed transverse-axial images, using regions of interest according to vessel size at the level of the pulmonary trunk, main pulmonary arteries, and lobar arteries, including the artery of the lingula. Enhancement values of ≥200 hounsfied units (HU) were considered diagnostic. Vessels affected by thromboembolism were not examined. Note was made of the CT- signs of right ventricular dysfunction: enlargement of the right ventricle on the axial sections in relation to the left ventricle and contrast medium reflux into the hepatic veins. Besides descriptive statistics, sub-group comparisons were made of flow rates, cannula size, and evidence of right ventricular dysfunction, using the chi square test.
RESULTS
Two patients were found to suffer from pulmonary embolism [9%, Figure 1]. Subjectively, only one scan was considered non-diagnostic, due to insufficient enhancement [95.4% diagnostic, Figure 2]. The mean contrast medium enhancement was 272 HU (168-506 HE). The mean enhancement in the pulmonary trunk, main arteries, and lobar arteries was 303, 293, and 281 HU, respectively. The threshold level of ≥200 HU was reached in 92.3% of all measurements. The central pulmonary vessels (pulmonary trunk, left and right pulmonary artery) showed a higher attentuation; here 98.5% of the vessels showed an enhancement ≥200 HU. No significant differences were found between the flow rates of 2.0 and 2.5 mL/s and between 20G and 22 G cannula sizes. However, patients with signs of right ventricular failure showed significantly reduced enhancement (P < 0.0001).
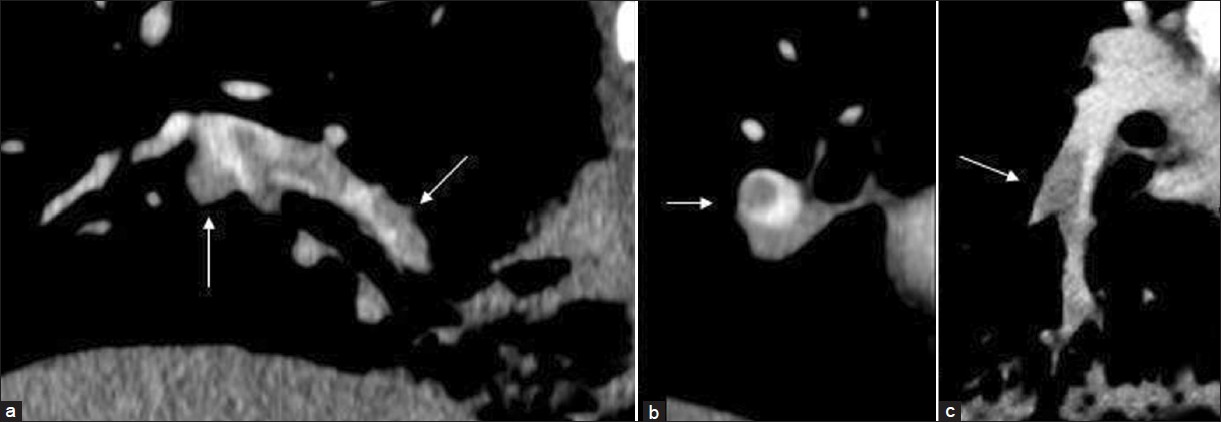
- Computed tomography pulmonary angiography with a flow rate of 2.0 mL/s in a patient with suspected pulmonary embolism. Different reformations (a,b and c) clearly show pulmonary emboli (arrows) in the right lower lobe.

- Computed tomography pulmonary angiography in two different patients with suspected pulmonary embolism. (a) With a flow rate of 2.5 mL/s and (b) with flow rate of 2.0 mL/s, Good vascular enhancement can be seen even in more peripheral vessels (arrows).
DISCUSSION
The data shown above indicates that even with a low injection flow rate CTPA, the enhancement of the central pulmonary arteries seem to be of diagnostic quality. This has important implications for everyday patient care. In patients with poor peripheral venous status the use of small bore canulas may be adequate. Especially in patients with cancer undergoing chemotherapy, it is sometimes almost impossible to insert large bore canulas. Transistory fine bore central venous devices in intensive care patients can also be used for CTPA with low flow rates. This is of importance with peripherally inserted central devices, in which flow rates up to 2.0 mL/s have been shown to be possible.[4] Most port catheter systems do not have an approval for power injectors. However, ‘off- label’ use of central devices with low flow rates (2.0 mL/s) is a common strategy in everyday clinical practice. This practice is supported by data from an in vitro study, in which all tested port catheters (none had an approval for power injectors) tolerated an injection rate of 2.0 mL/s.[5] Thus, it can be concluded that in these patients, CTPA can also be performed safely and with diagnostic quality using a low flow rate. A threshold for the vascular enhancement of ≥200 HU was used for good opacification. This threshold was chosen following the calculations used by Wittram, which was based on observations by Meanly et al.[36] They proposed a minimum contrast enhancement of pulmonary arterial blood of 93 HU to detect all acute emboli.[3] As contrast enhancement get worse toward the periphery, some researchers claim higher HU values for acute emboli. In this study, the needed minimum attenuation calculated by Wittram was doubled.[37] As in other studies, the measurement of opacification of segmental and subsegmental arteries was not performed. This is because accurate measurement of HU values in these vessels was difficult, due to partial volume averaging artifacts.[8] The comparison of our data with other published CTPA data is complicated because of the different protocols used, concentration of contrast media, and criteria of evaluation. Subjectively only one scan was considered non-diagnostic. This is in accordance with published data that indicate up to 10% of the CTPA examinations being of non-diagnostic value.[9] Keil et al., found a mean attentuation in the pulmonary trunk, using a flow rate of 4.0 mL/s, of around 350 HU. This was higher than the mean attentuation of 303 HU in our study.[10] This is not surprising, as the overall contrast enhancement was lower when compared to value obtained using higher flow rates. In this study, only two patients showed PE. This low incidence is a common finding on imaging studies. The low positive findings in imaging studies, nonspecific symptoms (dyspnea, thoracic pain), and the nonspecific finding of an elevated D- Dimer level is the reason for the reduced use of CTPA to rule out PE by clinicians.[11] An interesting option for the optimization of vascular opacification was the use of low kilovolt settings, and this could be used to counterbalance the observed small loss of contrast enhancement with the use of slow injection rates.[12] This feasability study had some inherent limitations: The small sample size and the lack of a control group. Also there was only one reader for the initial assessment of the quality of the examination. The findings need to be confirmed in a larger study.
CONCLUSION
Even with low injection flow rates of 2.0 or 2.5 mL/s, CTPA is of diagnostic value in most patients. This indicates low flow rates may be used in selected patients.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/57/100999
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Guidelines on the diagnosis and managment of acute pulmonary embolism: The Task Force for the Diagnosis and managment of acute pulmonary embolism of the European Society of Cardiology (ESC) Eur Heart J. 2008;29:2276-315.
- [Google Scholar]
- Power injection of contrast media via peripherally inserted central catheters for CT. J Vasc Interv Radiol. 2004;15:809-14.
- [Google Scholar]
- Contrast media pressure injection using a portal catheter system- results of an in vitro study] Rofo. 2005;177:1417-23.
- [Google Scholar]
- Detection of low-contrast in computed body tomography: An experimental study of simulated lesions. Radiology. 1980;134:149-54.
- [Google Scholar]
- Clincal usefulness of computed tomography study without contrast injection in the evaluation of acute pulmonary embolism. J Comput Assist Tomogr. 2005;29:6-12.
- [Google Scholar]
- Optimisation of contrast medium volume and injection- related factors in CT pulmonary angiography: 64- slice CT study. Eur Radiol. 2010;20:2100-7.
- [Google Scholar]
- The indeterminate CT pulmonary angiogramm: Imaging chaaracteristics and patient clinical outcome. Radiology. 2005;237:329-37.
- [Google Scholar]
- MDCT angiography of the pulmonary arteries: Intravascular contrast enhancement does not depend on iodine concentration when injecting equal amounts of iodine at standardizd iodine delivery rates. Eur Radiol. 2008;18:1690-5.
- [Google Scholar]
- Venous thromboembolism: Indirect CT venography during CT pulmonary angiography- should the pelvis be imaged. Radiology. 2008;246:605-11.
- [Google Scholar]
- Vascular enhancement and image quality of MDCT pulmonary angiography in 400 cases: Comparision of standard and low kilovoltage settings. AJR Am J Roentgenol. 2009;192:1651-6.
- [Google Scholar]






