Translate this page into:
Elastography in Distinguishing Benign from Malignant Thyroid Nodules
Address for correspondence: Dr. Deniz Alis, Department of Radiology, Cerrahpasa Medical Faculty, Istanbul University, Istanbul, Turkey. E-mail: drdenizalis@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
The aim of this study is to test the diagnostic success of strain elastography in distinguishing benign from malignant thyroid nodules.
Materials and Methods:
The size, echogenicity, and halo integrity of 293 thyroid nodules and the presence of microcalcification in these nodules were evaluated on gray-scale examination. Doppler characteristics and elastography patterns were also evaluated and recorded. Nodules were classified in four categories (patterns 1–4) based on elastographic examination.
Results:
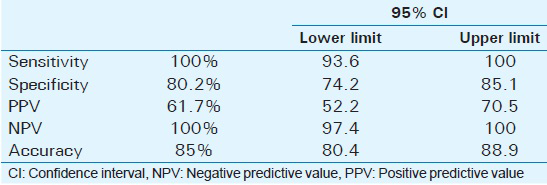
According to the cytopathological findings, 222 nodules were benign, and 71 nodules were malignant. The risk of a nodule to be malignant was 3.8 times increased by hypoechogenicity, 7.7 times increased by the presence of microcalcification, and 11.5 times increased by the absence of halo. On Doppler patterns, the presence of central vascularity increased the malignancy risk of a nodule by 5.8 times. According to the receiver operating characteristic analysis, patterns 3 and 4 were malignant, and patterns 1 and 2 were benign. The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of elastography were 100%, 80.2%, 61.7%, 100%, and 85%, respectively.
Conclusion:
Strain elastography can be used as a noninvasive method in distinguishing benign from malignant thyroid nodules and in identifying the patients who would undergo surgery.
Keywords
Benign
elastography
malignant
thyroid nodule
INTRODUCTION
Thyroid nodules are widely encountered in population, and they are usually benign. Its prevalence rates differ according to the population and the method used. It has also been reported that the prevalence of thyroid nodules is gradually increasing.[1] The risk factors for thyroid nodules include female gender, advanced age, iodine deficiency, and previous head and neck radiation. The prevalence of thyroid nodules has been reported to be detected 2%–6% by palpation, 19%–35% by ultrasonography (US), and 8%–65% in autopsy data.[2] Although palpation has an important place in the diagnosis of thyroid nodules during physical examination, ultrasonography is the most accurate and cost-effective method.[2] Fine-needle aspiration biopsy (FNAB) is mandatory in the preoperative diagnosis of thyroid nodules and in distinguishing benign from malignant nodules. High-resolution thyroid ultrasonography and real-time elastography are adjuvant tools to be benefited from in order to decide whether the patient in question should undergo surgery, especially if the patient has indeterminate or nondiagnostic cytology.[1]
Elastography is a method recently being used in the evaluation of thyroid nodules by comparing tissue elasticity.[3] Strain and shear-wave elastography (SWE) are two types of elastography still being used in clinical practice.[4] Two kinds of elasticity can be assessed by strain elastography. First, colors around and within the nodules were evaluated and visually scored according to the 4–5-scale scoring systems. Second, regions of interest are specified as the target region and the adjacent reference region. Later, elastograph calculates strain ratio automatically. Higher strain ratio leads to a high probability of malignancy.[4] A quantitative elastic value can be obtained by SWE depending on the acoustic pulse of an ultrasound probe, which stimulates tissues; accordingly, a real-time elastogram can be provided. The supersonic shear wave and acoustic radiation force impulse methods are used for the clinical assessment of thyroid nodules.[4]
The aim of the present study was to evaluate both gray-scale and Doppler US characteristics and strain elastographic findings in a large series of thyroid nodules, which were also confirmed cytopathologically. Moreover, the diagnostic success of strain elastography was also tested in distinguishing benign from malignant nodules.
MATERIALS AND METHODS
In the present study, the size, echogenicity, and halo integrity of 293 nodules and the presence of microcalcification in these nodules were evaluated on gray-scale examination. Moreover, Doppler characteristics and elastography patterns of the nodules were also evaluated and recorded. Ultrasonographic examination was performed by the Siemens Antares device (Siemens, Erlangen, Germany) using 9 L4 linear transducer. Elastographic findings of nodules were evaluated in the same protocol by two examiners, who were unaware of each other and of biopsy results. Written and verbal consents of the patients and the Ethics Committee approval were obtained.
Central vascularity of the nodules was evaluated and recorded during Doppler examination regarding coexistence of peripheral vascularization. Nodules were classified into four categories based on elastographic evaluation.[5] In pattern 1, the presence of softer tissue strain over the entire surface of the nodule was compared with values of surrounding thyroid tissue. In pattern 2, nodule was mainly soft but with the presence of harder areas (blue) which did not appear as a constant feature during real-time examination. In pattern 3, the presence of ample areas of hard strain (blue) was prevalently arranged in a constant manner at the periphery or at the center of the nodule. In pattern 4, nodule was totally made up of harder tissue strain compared with values of surrounding thyroid tissue [Figure 1].

- Schematic presentation of elastography. (a) A 33-year-old woman with hypoechogenic nodule in the left thyroid lobe (arrow). Strain elastography demonstrates the presence of softer tissue strain over the entire surface of the nodule compared with values of surrounding thyroid tissue (pattern 1). (b) Strain elastography examination of the same patient. Nodule (arrow) mainly soft, but with the presence of harder areas (blue), which did not appear as a constant feature during real-time examination (pattern 2). (c) A 44-year-old woman with hypoechogenic nodule in the right thyroid lobe (arrow). Strain elastography of the patient shows ample areas of hard strain (blue) prevalently arranged in a constant manner at the periphery or at the center of the nodule (pattern 3). (d) A 45-year-old woman with hypoechogenic nodule in the left thyroid lobe. Strain elastography of the patient shows totally made up of harder tissue strain compared with values of surrounding thyroid tissue (pattern 4).
Cytopathological examination findings of the nodules were obtained by FNAB, which was performed at the same center. According to the cytopathological findings, of 293 nodules, 222 were benign and 71 were malignant.
Statistical method
Data were analyzed using the Predictive Analytics Software (SPSS Inc., Chicago, IL, USA) for Windows version 18.0. Descriptive statistics were expressed as number and percentage for categorical variables and as mean, standard deviation, median, and minimum-maximum for numerical variables. In comparison of two independent groups, Mann–Whitney U-test was used for nonnormally distributed numerical variables. For categorical variables, Chi-square test was used, and when Chi-square condition was not met, Monte Carlo simulation was used for multiple comparisons. Kappa statistics were performed to assess agreement for categorical variables. The receiver operating characteristic (ROC) curve was used to determine the predictive cutoff value for elastography. Level of statistical significance was accepted as P < 0.05.
RESULTS
The characteristics of benign (n = 222) and malignant (n = 71) nodules are demonstrated in Table 1. No significant difference was determined between the benign and malignant groups in terms of nodule size. The absence of halo and the presence of microcalcification and the rate of hypoechogenicity in the malignant nodules were found to be significantly higher than those in the benign nodules. There were significant differences between the benign and malignant nodules in terms of Doppler patterns and elastography characteristics; the rates of pattern 4 and central vascularity were higher in the malignant group [Table 1].
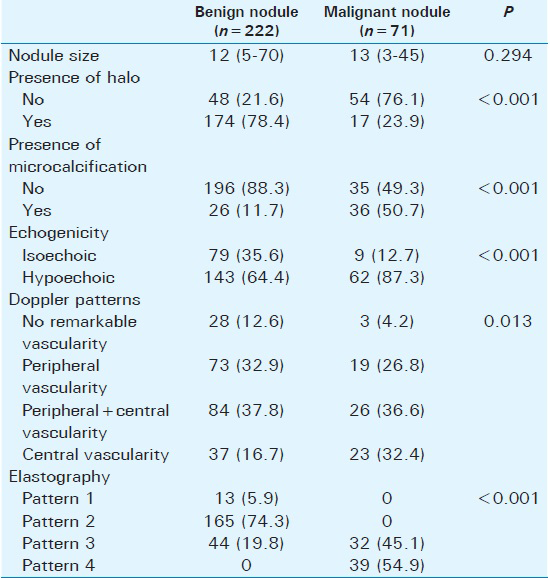
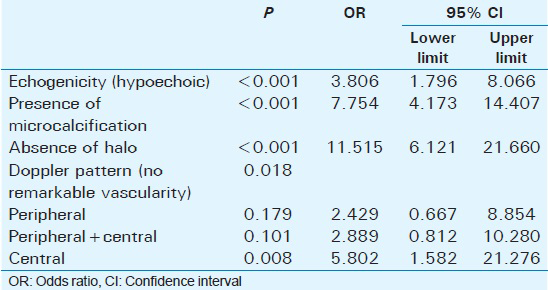
The risk of a nodule to be malignant was 3.8 times increased by hypoechogenicity, 7.7 times increased by the presence of microcalcification, and 11.5 times increased by the absence of halo. When the absence of remarkable vascularity on Doppler pattern was considered as a reference, central vascularity increased the malignancy risk of a nodule by 5.8 times [Table 2].
When the agreement between the examiners’ scores and the final scores in elastography examination was analyzed, the kappa value was 0.835 (P < 0.001) for the first examiner and 0.815 (P < 0.001) for the second examiner, with a significantly perfect (almost perfect) agreement.
ROC analysis, which was performed to determine a predictive cutoff value for malignant nodule on elastography examination, revealed patterns 3 and 4 to be malignant and patterns 1 and 2 to be benign (area under the curve; 95.5%, P < 0.001; Figure 2). Accordingly, the distribution of nodules is presented in Table 3, and the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of elastography are presented in Table 4.
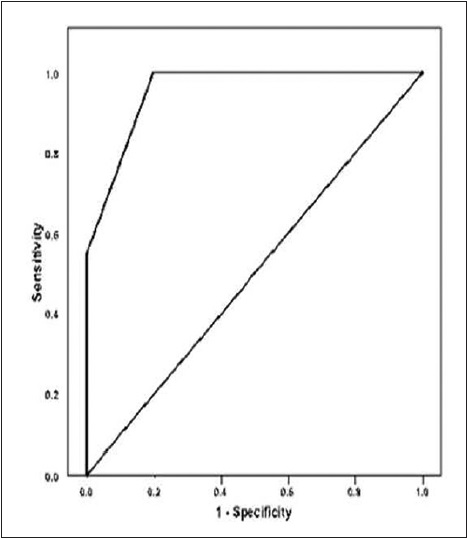
- Receiver operating characteristic analysis in elastography (area under the curve = 95.5%, 95% confidence interval: 93.5%–97.6%; P < 0.001).
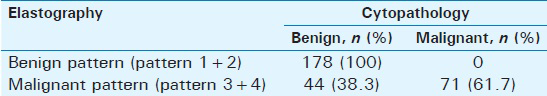
All of the nodules determined to be benign (pattern 1 + 2) on elastography were also cytopathologically benign, whereas 61.7% of the malignant nodules (pattern 3 + 4) on elastography were cytopathologically malignant.
DISCUSSION
Ultrasonography is the primary diagnostic tool in detection and examination of thyroid nodules. It has been reported that Doppler US has high sensitivity in differential diagnosis of malignant nodules particularly when performed by experienced professionals.[6] The presence of certain characteristics such as hypoechogenicity, microcalcifications and the absence of halo, hypervascularity, irregular borders, and mass growth pattern anterior–posterior being larger than medial–lateral (taller than wider on the transverse images of the thyroid lobe) in a thyroid nodule raise doubt about malignancy, and the presence of more than one characteristic in the same nodule increases the probability of malignancy. It has been reported that these characteristics, which are detectable through US, are sensitive but not sufficiently specific.[6] It has been stated that stiffness of thyroid nodules is an independent predictor of thyroid cancers.[7] Moreover, it has also been reported that elastography, which assesses nodule stiffness and has been recently put into practice, enhances specificity by overcoming the limitations of conventional B-mode and Doppler US and thereby is promising in identifying malignant lesions.[8] While strain elastography provides operator-dependent results because of subjective interpretation, SWE is operator independent; nevertheless, further studies are needed for validation of the method.[6]
After Rago et al.,[9] reported utilization of elastography in 2007 as a new technique with great potential for diagnosing thyroid cancers, in the literature to date, there have been several retrospective and prospective studies evaluating thyroid nodules by elastographic methods using different scoring systems and comparing with pathology or FNAB results among different patient groups.[1011121314151617181920212223] The primary goal of these studies is to demonstrate availability, benefits, and predictive values of noninvasive methods such as elastography to reduce the number of patients, for whom invasive diagnostic methods would be referred to or who would undergo surgery.
In the present study, in which strain elastography was performed, four classes of pattern approach recommended by Rubaltelli et al.,[5] and frequently used in the studies. Interobserver variability is a matter of concern in the evaluation by elastography. Ko et al.,[24] evaluated the effect of physician's experience in distinguishing malignant thyroid nodules from benign nodules using elastography and reported that experienced physicians had superior specificity compared to inexperienced physicians. In another study, for interobserver agreement, Cantisani et al.,[25] reported the highest Cohen's kappa coefficient for the strain ratio measurements (0.95) and the lowest Cohen's kappa coefficient for the echogenicity score (0.83). In their study conducted with three independent operators, Ragazzoni et al.,[26] found a good agreement among the operators (kappa test: 0.64, P < 0.0001). In the present study, the agreement between two examiners’ scoring was almost perfect compared to the final scoring (kappa values 0.835 for the first examiner and 0.815 for the second examiner).
There are studies investigating specificity and sensitivity of elastography. Ragazzoni et al.,[26] conducted a study with 132 nodules (92 benign and 40 malignant) using elastography and reported 77 out of 92 benign nodules were categorized as score 1 or 2 and 34 out of 40 malignant nodules were categorized as score 3 or 4 (sensitivity 85%, specificity 83.7%, PPV 69.3%, and NPV 92.7%). Asteria et al.,[27] evaluated 17 malignant and 69 benign lesions and found the sensitivity, specificity, PPV, NPV, and accuracy of elastography to be 94.1%, 81%, 55.2%, 98.2%, and 83.7%, respectively. Ferrari et al.,[28] evaluated 23 thyroid nodules and reported that 78% of benign nodules were patterns 1–2 and 88% of malignant nodules were patterns 3–4. In the same study, the sensitivity, specificity, PPV, NPV, and diagnostic accuracy of elastography were determined to be 88%, 78%, 72%, 91%, and 82%, respectively. Moreover, Cantisani et al.,[29] prospectively evaluated 97 patients and found the sensitivity and specificity of elastography to be 97.3% and 91.7%, respectively, and reported that the lesions with strain ratio ≥2 were quite likely in malignant nature. In another study by Cantisani et al.,[30] they evaluated 89 benign and 58 malignant cases who underwent thyroidectomy and found the sensitivity and specificity to be 93% and 89%, respectively, when the cutoff value for elastography score was considered to be 2. According to the result of that particular study, it was reported that elastography provided more accurate findings compared to US and color Doppler US. Shweel and Mansour[31] found the sensitivity, specificity, PPV, NPV, and accuracy of elastography to be 75.4%, 85.5%, 71.4%, 90.5%, and 86.7%, respectively, and reported that diagnostic performance of elastography increased when it was used together with high-resolution US.
Bojunga et al.,[32] performed a meta-analysis by evaluating the studies which were conducted on real-time elastography for distinguishing benign from malignant thyroid nodules and reported that elastography was beneficial for the patients undergoing surgery. In that meta-analysis, 8 studies including a total of 639 nodules were analyzed, and it was revealed that the overall mean sensitivity and specificity for the diagnosis of malignant thyroid nodules were 92% confidence interval (CI), 88–96 and 90% CI, 85–95, respectively. In another meta-analysis performed by Ghajarzadeh et al.,[33] 12 studies, which evaluated 1180 thyroid nodules, were systematically reviewed, and diagnostic accuracy of sonoelastography in detecting malignant nodules was investigated. They concluded that the highest sensitivity was achieved by a threshold elasticity score of between 1 and 2 as 98.3% (95% CI, 96.2%–99.5%). They also reported that it was not necessary for the patients with elasticity score of 1 to undergo further invasive examinations. Akcay et al.,[34] evaluated 110 nodules by stiffness score using US elastography and found the sensitivity, specificity, PPV, and NPV to be 100%, 95%, 40%, and 100%, respectively, when the cutoff value for malignancy was considered to be score 4; they recommended biopsy for all score 4 nodules but not for score 1. In the present study as well, all of the patterns 1 and 2 nodules on strain elastography were found to be benign, whereas 61.7% of patterns 3 and 4 nodules were malignant. “Our study had a larger number of the population compared to studies in the literature.” The sensitivity, specificity, PPV, NPV, and accuracy of elastography were found to be 100%, 80.2%, 61.7%, 100%, and 85.0%, respectively.
The main limitation of the present study was the use of strain mode since only it was available at the time of study. Another limitation was that the definite diagnosis of the patients was performed cytopathologically as the thyroid nodules were monitored without surgery unless they were malignant according to the FNAB or unless there was another indication.
CONCLUSION
To the results of the present study as well as the findings from the literature review, strain elastography could be used as a noninvasive method for distinguishing benign thyroid nodules from malignant thyroid nodules and for identifying the patients undergoing surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/51/197074
REFERENCES
- Epidemiology of thyroid nodules. Best Pract Res Clin Endocrinol Metab. 2008;22:901-11.
- [Google Scholar]
- Ultrasound elastography for thyroid nodules: Recent advances. Ultrasonography. 2014;33:75-82.
- [Google Scholar]
- Differential diagnosis of benign and malignant thyroid nodules at elastosonography. Ultraschall Med. 2009;30:175-9.
- [Google Scholar]
- Ultrasound elastography in the evaluation of thyroid nodules for thyroid cancer. Curr Opin Oncol. 2013;25:1-5.
- [Google Scholar]
- Performance of elastography for the evaluation of thyroid nodules: A prospective study. Thyroid. 2013;23:734-40.
- [Google Scholar]
- Conventional ultrasound integrated with elastosonography and B-flow imaging in the diagnosis of thyroid nodular lesions. Int J Surg. 2014;12(Suppl 1):S117-22.
- [Google Scholar]
- Elastography: New developments in ultrasound for predicting malignancy in thyroid nodules. J Clin Endocrinol Metab. 2007;92:2917-22.
- [Google Scholar]
- Real-time ultrasound elastography in the differential diagnosis of benign and malignant thyroid nodules. J Ultrasound Med. 2009;28:861-7.
- [Google Scholar]
- Shear wave elastography: A new ultrasound imaging mode for the differential diagnosis of benign and malignant thyroid nodules. J Clin Endocrinol Metab. 2010;95:5281-8.
- [Google Scholar]
- Differentiation of benign from malignant thyroid lesions: Calculation of the strain ratio on thyroid sonoelastography. J Ultrasound Med. 2011;30:663-9.
- [Google Scholar]
- Comparison of the diagnostic accuracy of combined elastosonography and BRAF analysis vs. cytology and ultrasonography for thyroid nodule suspected of malignancy. Clin Endocrinol (Oxf). 2012;77:608-14.
- [Google Scholar]
- Application of real-time ultrasound elastography in diagnosing benign and malignant thyroid solid nodules. Cancer Biol Med. 2012;9:124-7.
- [Google Scholar]
- Does elastography reduce the need for thyroid FNAs? Clin Endocrinol (Oxf). 2013;78:942-9.
- [Google Scholar]
- Quantitative assessment of shear-wave ultrasound elastography in thyroid nodules: Diagnostic performance for predicting malignancy. Eur Radiol. 2013;23:2532-7.
- [Google Scholar]
- Comparison of diagnostic value of conventional ultrasonography and shear wave elastography in the prediction of thyroid lesions malignancy. PLoS One. 2013;8:e81532.
- [Google Scholar]
- Comparison of strain ratio with elastography score system in differentiating malignant from benign thyroid nodules. Clin Imaging. 2013;37:50-5.
- [Google Scholar]
- Value of strain-ratio on thyroid real-time sonoelastography. Radiol Med. 2014;119:149-55.
- [Google Scholar]
- Shear wave elastography versus real-time elastography on evaluation thyroid nodules: A preliminary study. Eur J Radiol. 2014;83:1135-43.
- [Google Scholar]
- Elastography in the differential diagnosis of thyroid nodules in Hashimoto thyroiditis. Med Oncol. 2014;31:97.
- [Google Scholar]
- Solid hypo-echoic thyroid nodules on ultrasound: The diagnostic value of acoustic radiation force impulse elastography. Ultrasound Med Biol. 2014;40:2020-30.
- [Google Scholar]
- The value of acoustic radiation force impulse (ARFI) in the differential diagnosis of thyroid nodules. Eur J Radiol. 2013;82:e686-90.
- [Google Scholar]
- Diagnostic performance of ultrasound and ultrasound elastography with respect to physician experience. Ultrasound Med Biol. 2014;40:854-63.
- [Google Scholar]
- Q-elastosonography of solid thyroid nodules: Assessment of diagnostic efficacy and interobserver variability in a large patient cohort. Eur Radiol. 2014;24:143-50.
- [Google Scholar]
- High diagnostic accuracy and interobserver reliability of real-time elastography in the evaluation of thyroid nodules. Ultrasound Med Biol. 2012;38:1154-62.
- [Google Scholar]
- US-elastography in the differential diagnosis of benign and malignant thyroid nodules. Thyroid. 2008;18:523-31.
- [Google Scholar]
- Ultrasound examination using contrast agent and elastosonography in the evaluation of single thyroid nodules: Preliminary results. J Ultrasound. 2008;11:47-54.
- [Google Scholar]
- Prospective evaluation of multiparametric ultrasound and quantitative elastosonography in the differential diagnosis of benign and malignant thyroid nodules: Preliminary experience. Eur J Radiol. 2012;81:2678-83.
- [Google Scholar]
- Prospective evaluation in 123 patients of strain ratio as provided by quantitative elastosonography and multiparametric ultrasound evaluation (ultrasound score) for the characterisation of thyroid nodules. Radiol Med. 2013;118:1011-21.
- [Google Scholar]
- Diagnostic performance of combined elastosonography scoring and high-resolution ultrasonography for the differentiation of benign and malignant thyroid nodules. Eur J Radiol. 2013;82:995-1001.
- [Google Scholar]
- Real-time elastography for the differentiation of benign and malignant thyroid nodules: A meta-analysis. Thyroid. 2010;20:1145-50.
- [Google Scholar]
- Diagnostic accuracy of sonoelastography in detecting malignant thyroid nodules: A systematic review and meta-analysis. AJR Am J Roentgenol. 2014;202:W379-89.
- [Google Scholar]
- The value of ultrasound elastography in differentiation of malignancy in thyroid nodules. Clin Imaging. 2014;38:100-3.
- [Google Scholar]






