Translate this page into:
Initial Experience with a Cone-beam Breast Computed Tomography-guided Biopsy System
Address for correspondence: Dr. Posy J Seifert, Elizabeth Wende Breast Care, LLC, 170 Sawgrass Drive, Rochester, NY 14620, USA. E-mail: pseifert@ewbc.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
To evaluate our initial experience with a cone-beam breast computed tomography (BCT)-guided breast biopsy system for lesion retrieval in phantom studies for use with a cone-beam BCT imaging system.
Materials and Methods:
Under the Institutional Review Board approval, a phantom biopsy study was performed using a dedicated BCT-guided biopsy system. Fifteen biopsies were performed on each of the small, medium, and large anthropomorphic breast phantoms with both BCT and stereotactic guidance for comparison. Each set of the 45 phantoms contained masses and calcification clusters of varying sizes. Data included mass/calcium retrieval rate and dose and length of procedure time for phantom studies.
Results:
Phantom mass and calcium retrieval rate were 100% for BCT and stereotactic biopsy. BCT dose for small and medium breast phantoms was found to be equivalent to or less than the corresponding stereotactic approach. Stereotactic-guided biopsy dose was 34.2 and 62.5 mGy for small and medium breast phantoms, respectively. BCT-guided biopsy dose was 15.4 and 30.0 mGy for small and medium breast phantoms, respectively. Both computed tomography biopsy and stereotactic biopsy study time ranged from 10 to 20 min.
Conclusion:
Initial experience with a BCT-guided biopsy system has shown to be comparable to stereotactic biopsy in phantom studies with equivalent or decreased dose.
Keywords
Breast biopsy
breast cancer
breast computed tomography

Introduction
Image-guided biopsy was developed by breast imagers to diagnose lesions with minimally invasive technology to benefit the patient and lower health-care costs.[1] Definitive diagnosis with percutaneous needle core biopsy of breast lesions found at imaging has proven to be extremely beneficial for surgical planning when malignancy is diagnosed.[23] Percutaneous needle core biopsy has also proven to save medical dollars when benign breast lesions are diagnosed, eliminating the need for expensive open surgical biopsy.[4]
A breast lesion may only be visible on a specific imaging modality, such as mammography, ultrasound, or magnetic resonance imaging (MRI), necessitating the biopsy to be performed under such guidance. Many studies have been performed over the years to prove the efficacy of image-guided breast biopsy. Parker et al., led the way in a study that described their early work in 1990 involving both a stereotactic biopsy just before needle localization and subsequent open surgical biopsy.[5] The results discussed the early failures due to insufficient needle size and inexperience, as well as successes with increased experience and the use of larger gauge needles, which resulted in a 97% agreement with surgical pathology. The study concluded that large-gauge percutaneous needle biopsy may be an alternative to open surgical biopsy. Today, most nonpalpable mammographically identified abnormalities can reliably be biopsied stereotactically with the exception of a very thinly compressed breast with a negative stroke margin or a patient who exceeds the weight limit of the table.
Similarly, for breast MRI, a multicenter study published in 2002 by Perlet et al., evaluated a dedicated MRI-guided vacuum breast biopsy device.[6] The study results indicated that MRI-guided vacuum-assisted biopsy, used in combination with a dedicated breast biopsy coil, offered the possibility of accurate diagnosis of very small lesions only visualized by MRI. Currently, MRI biopsy is widely used for MRI-identified abnormalities that do not have an ultrasound or mammographic correlate.
Cone-beam breast computed tomography (BCT) is a novel three-dimensional (3D) tomographic imaging technique. To date, at least two research cone-beam BCT prototypes have been developed for patient studies by Lindfors and Boone and Chen and Ning, with the latter receiving the Food and Drug Administration (FDA) approval for diagnostic breast imaging.[78] Boone et al., in 2006 described initial subject study images as having excellent anatomical detail with exquisite visualization of the soft tissue components of tumors in comparison to surrounding adipose tissue.[9] In 2008, the California group, Lindfors and Boone, reported on continued experience with the technology stating that computed tomography (CT) was equal to screen film mammography for visualization of breast lesions, significantly better for the visualization of masses; however, at the time, screen film mammography outperformed CT in the visualization of microcalcifications.[7] The subjects imaged found that the CT examination was significantly more comfortable than mammography due to lack of compression and table comfort.[7] Studies published in 2010 and 2012 by O'Connell et al., also reported better lesion conspicuity on the cone-beam BCT images verses mammography due to the breast being scanned in its natural, uncompressed state, avoiding structure, and tissue overlap, thus allowing the breast to be seen in its true, 3D state.[1011] This study on normal screening patients reported 100% mass detectability and 86.5% calcification detectability. The authors found that mammography was better at depicting the details of calcifications due to the beam hardening artifact inherent with CT scans. However, they found that BCT was better than mammography at identifying the location of the calcifications in the breast.[10] The author's most recent diagnostic study in 2012 reported that the detail of microcalcifications was similar when comparing BCT to mammography and the distribution was better characterized with BCT, due to the ability to remove tissue overlap.[11]
As BCT continues to be studied and implemented into the breast imaging paradigm, where it will fit in remains to be seen. Currently, only one BCT device is FDA approved for diagnostic imaging only, not yet for screening. As with any adjuvant imaging test, the possibility exists that additional findings not identified by other imaging methods will occur. What that percentage ultimately is and what specific lesion types, remains to be seen as the technology is incorporated into clinical use. It would likely be useful in patients who have contraindications to breast MRI. To be clinically useful and practical, the cone-beam BCT technology should have a biopsy method and apparatus incorporated for nonpalpable masses and calcifications only seen with BCT for definitive diagnosis. This would be comparable to stereotactic breast biopsy use for nonpalpable lesions found by mammography and MRI-guided biopsy use for abnormalities seen on MRI only. The BCT-guided biopsy system commercial-prototype reported in this study includes a novel biopsy bracket and 3D guidance procedure which enables the localization, targeting, and successful retrieval of lesions with BCT 3D visualization. The purpose of this study was to report on our experience in the evaluation of a BCT-guided biopsy system prototype for lesion retrieval in phantom studies.
Materials and Methods
After the Institutional Review Board approval, a phantom biopsy validation testing study was initiated and performed from August 2011 to February 2012. Study imaging was performed with the Koning BCT unit, with a weight limit of 440 pounds (200 kg) (Model CBCT1000, Koning Corporation, West Henrietta, New York, USA).
Breast computed tomography biopsy apparatus design
A biopsy bracket was developed as an attachment to the existing cone-beam BCT system by mounting to the bottom of the patient table. The biopsy grid and back compression plate design [Figure 1] allows for firm but comfortable compression of the breast (manually compressed in ~1 mm increments) and has a quick compression release. The simple design is constructed from low X-ray attenuation material and can rotate 360° around the breast before compressing the breast to obtain the shortest skin-to-lesion distance for biopsy [Figure 2]. The design is intended for use with an FDA-approved commercially available biopsy grid, needle block, and introducer set.
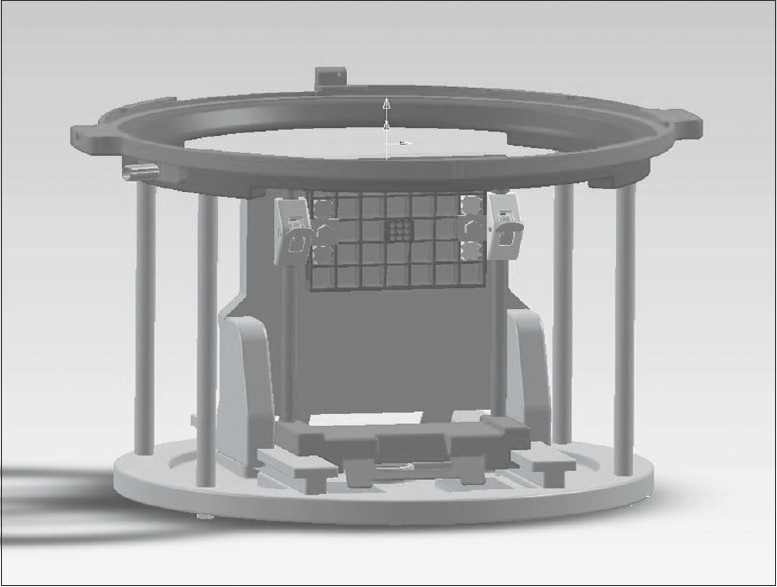
- Three-dimensional solid model of breast computed tomography biopsy bracket.
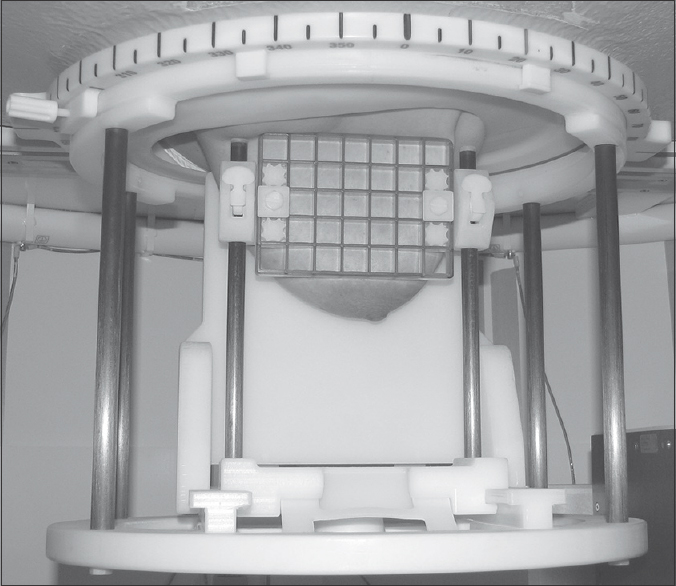
- Subject's breast compressed in the breast computed tomography biopsy bracket.
Phantom design
Three anthropomorphic breast biopsy phantoms (small [~500 cc], medium [~1000 cc], and large [~1250 cc]) were designed with a 50/50 adipose to glandular tissue-equivalent background composition for biopsy device testing. Each phantom contained 15 lesions: 10 mass lesions consisting of material with density equivalent to a mass (2 each of sizes 10–15, 8–10, 6–8, 4–6 and 2–4 mm), randomly placed within the phantom and 5 calcification clusters (CaCO3, size: 0.21-0.25 mm), with cluster sizes of 3, 5, 7, 9, and 11 mm ± 1 mm randomly placed. Phantoms were designed to be compressible, similar to an actual breast. Phantoms were manufactured and supplied by Computerized Imaging Reference Systems, Inc. (Tissue Simulation and Phantom Technology, Norfolk, Virginia, USA).
Phantom design confirmation
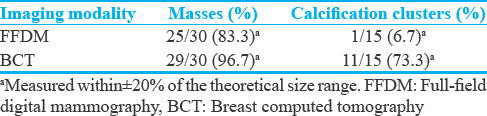
Before phantom biopsy testing, phantom lesion visualization comparison between Full-Field Digital Mammography (FFDM) and BCT was conducted. Both FFDM and BCT phantom imaging was performed to identify, measure, and document that all 30 masses and 15 calcification clusters in each phantom set (small, medium, and large phantom) were visible. All phantoms were compressed (comparable to breast compression) and imaged by a registered radiologic technologist under the supervision of a licensed medical physicist with both the BCT system and FFDM to document the size and the position of the “lesions” within the phantom.
After phantom lesion confirmation was obtained, the first phase of the biopsy study was to perform BCT-guided biopsy of all masses and calcification clusters in each of the small, medium, and large breast phantoms. There were 10 masses and 5 calcification clusters randomly placed in each breast phantom for a total of 45 BCT biopsies. The next phase was to perform the 45 stereotactic biopsies with the breast phantoms (15 biopsies of all lesions in each of the small, medium, and large breast phantoms). Faxitron® (Faxitron Bioptics, LLC, Tucson, Arizona, USA) imaging of the biopsy samples was used for verification of successful biopsy by imaging the specimen to confirm target retrieval.
Fifteen 9-gauge (9 g) vacuum biopsies were performed on each of the three phantoms with the use of the Hologic vacuum-assisted biopsy system (ATEC Pearl) and standard disposables. The phantom biopsy study testing consisted of both BCT-guided biopsy [Figures 3–5] and stereotactic-guided biopsy.
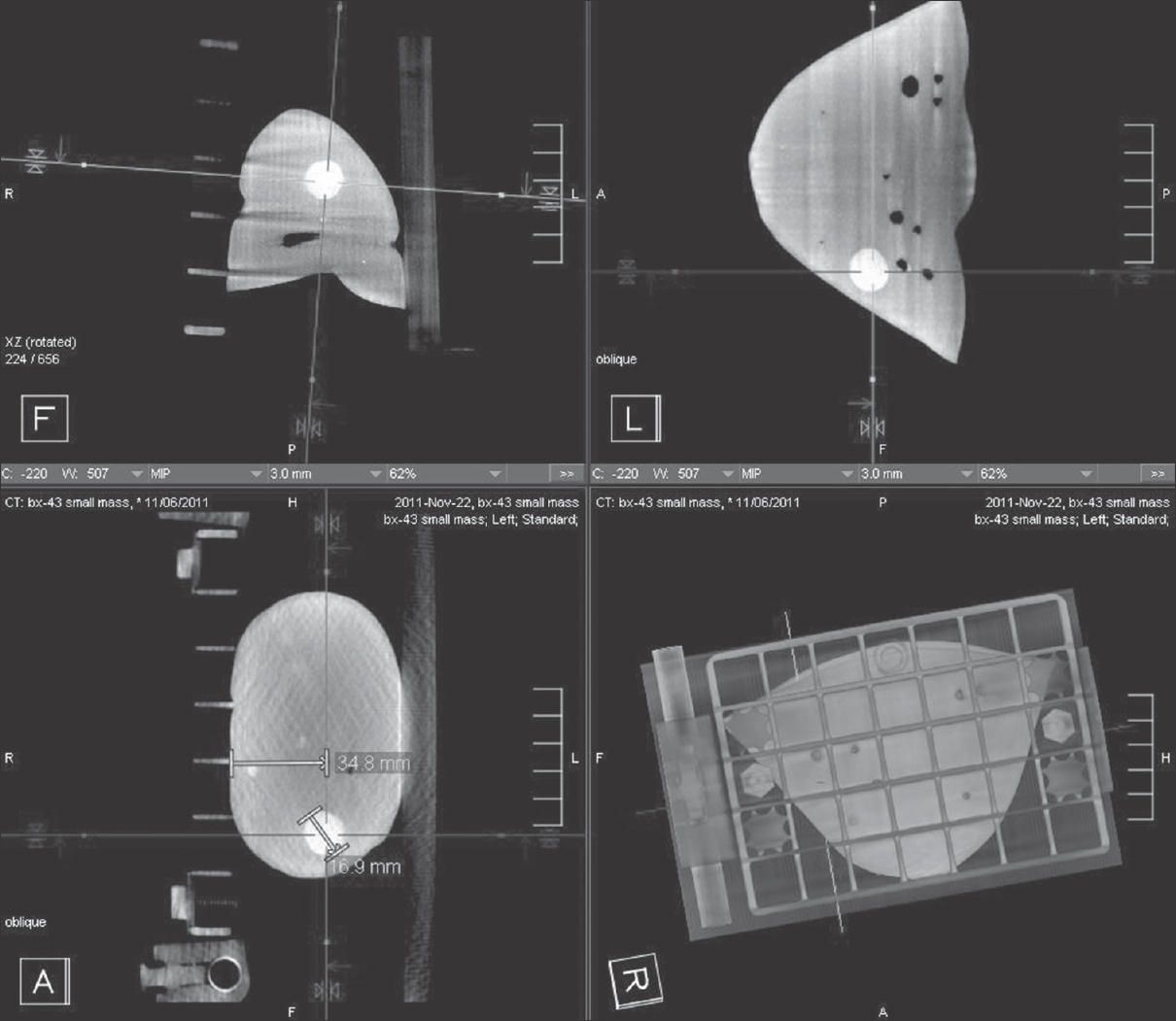
- Multiplanar breast computed tomography images of phantom with mass for lesion localization.

- Prebiopsy phantom imaging.
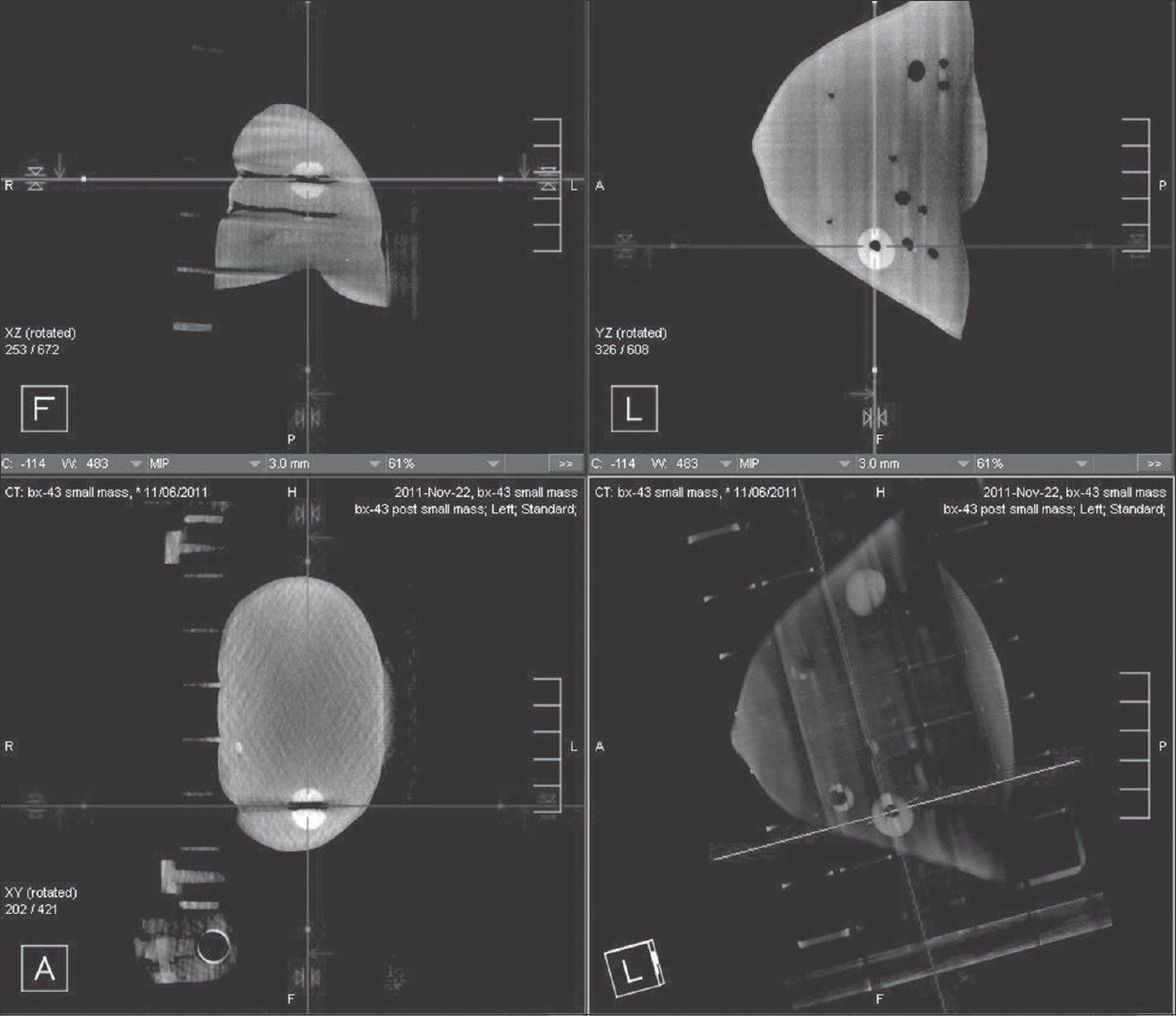
- Postbiopsy phantom imaging. The dark circular area within the white lesion corresponds with the biopsy site sampled.
All 45 phantom lesions (30 masses and 15 calcifications) were biopsied with both the BCT-guided biopsy system utilizing the Koning CT unit and stereotactic guidance utilizing the Hologic MultiCare™ Platinum prone breast biopsy table (Hologic Inc., Bedford, MA, USA). Phantom biopsies were performed by a registered radiologic technologist with 20 years of experience in mammography, 19 years of experience in stereotactic biopsy, 5 years of experience in BCT imaging, and a licensed medical physicist with over 15 years of experience in radiological and CT imaging. Data from the phantom lesion biopsies were collected and recorded on a case report form, which included lesion visualization, lesion location and depth, success and failure rate, and procedure time.
Breast computed tomography-guided phantom biopsy protocol
The phantom BCT-guided biopsy imaging protocol consisted of two low-dose (~0.01 mGy each) orthogonal scout views and four 3D 360° BCT scans. The scout images were obtained to determine the dose necessary to produce optimal quality images; the dose was automatically determined from the scout images by the BCT control program for the specific breast phantom size and density. A 3D 360° BCT and a prebiopsy 3D targeting scan of the phantom were then performed. From this scan, the optimal grid block location and needle-guide opening were determined that gave the best trajectory of the biopsy needle to the lesion. The shortest skin-to-lesion depth was determined from the 3D BCT imaging. Breast phantom thickness, posterior to the targeted lesion, was also measured to ensure that there was sufficient material (simulated tissue) beyond the target so that the biopsy needle would not pass through the posterior portion of the breast phantom. Once this was achieved, the needle guide block was inserted into the appropriate block of the grid. An introducer stylet was inserted and hubbed to the introducer sheath; a 'depth stop' on the introducer sheath was placed in the appropriate location based on the skin-to-lesion depth determined from the BCT 3D imaging. The introducer sheath with the introducer stylet was inserted into and through the needle guide to the depth stop. The stylet was removed from the introducer sheath leaving the introducer sheath in place. The localizing obturator was inserted into the introducer sheath.
A prebiopsy 3D BCT scan was performed to confirm accuracy of the position of the tip of the obturator in 3D (where biopsy harvesting of tissue would take place). Once the position was confirmed, the localizing obturator was removed, a 9 g suros ATEC biopsy needle was inserted and the area of interest was biopsied, retrieving at least six samples from the lesion, as per normal vacuum-assisted biopsy procedure. Once the biopsy was completed, the ATEC biopsy hand piece was removed (leaving the introducer sheath in place). Postacquisition BCT imaging was performed to confirm biopsy of the targeted area in 3D. Postbiopsy phantom specimen radiograph imaging with Faxitron® was performed for radiographic evidence that the harvested tissue (mass or calcifications) was obtained.
The stereotactic phantom biopsy imaging protocol consisted of 9 images: scout, stereo targeting acquisition (+/-15°) (2 images), pre-fire stereo acquisition (+/-15°) (2 images), post-fire stereo acquisition (+/-15°) (2 images), and post-biopsy stereo acquisition (+/-15°) (2 images). Postbiopsy phantom specimen radiograph imaging with Faxitron® was performed for radiographic evidence of the harvested tissue (mass or calcifications) for the stereotactic phantoms.
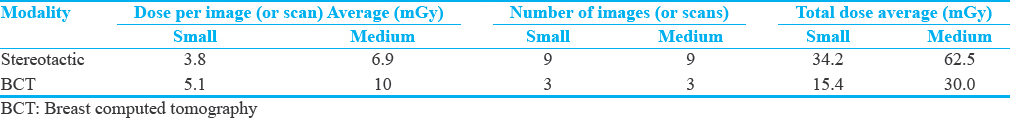
Phantom dose
The mean glandular dose for the stereotactic-guided biopsy imaging was determined by the radiographic parameters used (kVp, mAs). This was controlled by the Automatic Exposure Control (AEC), and indicated on the modality after exposure. At least nine images were generally required for the stereotactic-guided biopsy procedure. For BCT-guided biopsy, the average absorbed dose per scan (±20%) depended on the mA used (as determined by phantom studies and Monte Carlo calculations, kVp, and time are constant). This was determined from the “Best mA” procedure on the BCT console which is calculated from the scout images. As indicated above, three scans were required for this procedure [Table 1]. This was based on phantom CTDI measurements and Monte Carlo-based estimates. Two low-dose projection images (at 0 and 90°) are initially taken to verify positioning and calculate best mA based on size and density of the breast (or breast phantom). These are approximately 0.01 mGy each.

Only the average values of dose for the small and medium phantoms are listed. This was due to the fact that the stereotactic AEC system reached the maximum exposure time set by the unit when imaging the large phantom. Therefore, dose for the large phantom could not be accurately recorded. Arbitrary, manually chosen kVp and mAs values were selected to achieve the optimally penetrated images required to perform the large phantom biopsies. From the two low-dose scout views, BCT selected and used the maximum current of 200 mA for the large phantom.
Results
Phantom lesion visualization between full-field digital mammography and breast computed tomography
Before phantom biopsy testing, a comparison of phantom lesion visualization between FFDM and BCT was conducted by the medical physicist. All 30 masses and 15 calcification clusters in each phantom set were imaged and measured on both FFDM and BCT. The results are shown in Table 2.
Breast computed tomography-guided biopsy phantom testing
One of two identical sets of small, medium, and large phantoms underwent BCT-guided biopsy. The other set underwent stereotactic-guided biopsy. The total procedure time for BCT-guided phantom biopsy ranged from 10 to 20 min which was similar to that of the stereotactic phantom biopsy (range 10–20 min).
There was 100% retrieval success rate for all 15 calcification clusters in each phantom set (both the BCT-guided biopsy and stereotactic-guided biopsy). There was also 100% retrieval rate for all 30 masses in each phantom set. Evidence of mass lesion and calcification retrieval was documented by review of postbiopsy specimen radiography.
The results of the dose comparison are shown in Table 3. The stereotactic phantom biopsy imaging protocol consisted of 9 images: scout, stereo targeting acquisition (+/-15°) (2 images), pre-fire stereo acquisition (+/-15°) (2 images), post-fire stereo acquisition (+/-15°) (2 images), and post-biopsy stereo acquisition (+/-15°) (2 images). For stereotactic biopsy, nine images were acquired (scout, stereo targeting acquisition [±15°], prefire stereo acquisition [±15°], postfire stereo acquisition [±15°], and postbiopsy stereo acquisition [±15°]) The total stereo biopsy dose was the sum of the nine exposures, as reported by the modality. For BCT biopsy, three scans were required (scout, prebiopsy, and postbiopsy).
Discussion
BCT is a true, isotropic 3D tomographic modality that allows improved visualization of lesions due to the elimination of overlapping breast anatomy. As BCT imaging continues to be studied and implemented clinically in breast imaging, it is important to have a BCT biopsy apparatus and procedural method in place for lesions that are only visualized by BCT.
Initial phantom testing described in this study utilizing the Koning BCT system indicates that the BCT-guided biopsy system is a reliable and safe method for biopsy. This preliminary investigation is important as there is no published work to date on a dedicated BCT-guided biopsy apparatus system and procedure. Based on the results of this phantom study, we believe that this true 3D BCT-guided biopsy technique should now be studied clinically to provide the clinician confidence in locating and harvesting samples from breast lesions. Future BCT-guided biopsy subject studies should demonstrate an accurate and time-efficient biopsy method based on the preliminary phantom work.
As breast MRI became increasingly used and demonstrated the ability to detect mammographic, sonographic, and clinically occult lesions, the need for MRI-guided biopsy became apparent. The MRI biopsy technique was studied and implemented as described in a study by Liberman.[12] The authors concluded that their technique using vacuum-assisted biopsy was fast, safe, and an accurate alternative to open surgical biopsy for MRI-detected lesions. Another study published in 2005 by Liberman et al., reported their experience with MRI-guided 9 g breast biopsy of 112 nonpalpable, mammographically occult MRI-detected breast lesions.[13] The authors stated comparable findings to the previous study; that the procedure is a fast and safe alternative to surgical biopsy, as concordance with imaging was achieved in all but nine lesions. Moreover, researchers working with breast-specific gamma imaging (BSGI) have developed biopsy capabilities to access lesions which are occult on other conventional breast imaging modalities and seen only on BSGI.[14] With more research and as clinical data are compiled on BCT imaging, the breast imaging community will learn the rate at which BCT detects abnormalities not identified with standard imaging. In these instances of BCT only findings, BCT-guided biopsy will be necessary for definitive diagnosis.
Knowing the necessity for definitive diagnosis of lesions seen only by a specific modality, Raylman et al. published several papers discussing their work with positron emission tomography/mammography (PET/PEM) imaging and biopsy-guided device phantom work.[1516] Similar to our study, their initial work began with simulated biopsies using breast phantoms. Once the phantom studies showed potential for accuracy and precision, the studies advanced to human subjects. Kalinyak et al., reported the results from a prospective multicenter study of 24 PEM-biopsied lesions seen on PET imaging.[17] Study results showed that PEM-guided breast biopsy was both safe and effective for the sampling of lesions demonstrated on PET imaging. With the next phase for BCT-guided biopsy, it is logical for human subjects to be enrolled in studies to confirm imaging and histopathological concordance to prove its efficacy for diagnosis of breast abnormalities.
There were definite limitations with our BCT-guided biopsy study. The phantom included 50/50 adipose to glandular tissue composition used for biopsy device testing would be considered a limitation. We understand that conducting biopsies of suspended masses and calcium clusters in a homogeneous phantom may have resulted in artificially high detectability, but we believed this testing was a necessity before human subject testing. Our results are comparable to preliminary research published on breast PET/PEM. We anticipate similar results with human studies as clinical BCT-guided biopsy studies are performed and observed. This will be necessary to prove the techniques ability before real-world clinical implementation. Once these noncontrast studies are obtained and confirmed, contrast-enhanced BCT clinical trials with the use of the BCT-guided biopsy system can be conducted to address all BCT imaging needs.
The radiation dose was not a limitation; however, it was a concern as we strive to image wisely and should be closely observed when conducting human studies.
As indicated in Table 3, dose from the phantom studies was less than half of that used for stereotactic guidance.
BCT is a true isotropic modality, allowing greater conspicuity of lesions due to the elimination of tissue overlap. A feasibility study of BCT imaging in the evaluation of malignant lesions conducted by Seifert et al., demonstrated BCT's accuracy at identifying malignant lesions.[18] The study also reported on the visualization of lesions by BCT, not seen by other imaging modalities. This study demonstrated that BCT-guided biopsy will be necessary in such situations.
BCT-guided biopsy can be performed with the advantage of visualizing a lesion in three planes (a 3D relationship of the breast tissue). In addition, the option of a BCT-guided biopsy may be advantageous as an alternative method for breast tissue diagnosis, or for lesions difficult to reach on stereotactic or MRI-guided biopsy (posterior and medial lesions). Further, BCT-guided biopsy can serve as an alternative biopsy method for those patients with contraindications for stereotactic biopsy or MRI-guided biopsy, such as weight limitations, claustrophobia, and those with implantable devices. In addition, BCT may not need contrast enhancement, as is needed with MRI biopsy, to visualize lesions due to the high-resolution images.
Our study demonstrated that lesion visualization and size measurement utilizing breast phantoms are at least equivalent between BCT and FFDM. Our initial observations found that BCT-guided biopsy has at least equivalent biopsy accuracy compared to stereotactic biopsy, and in addition, the dose of BCT-guided biopsy was found to be less than half that of stereotactic-guided biopsy. Although BCT-guided biopsy is in its early stages, it should be easily adopted into routine practice by breast imagers due to its incorporation of familiar techniques and commercially available equipment.
Financial support and sponsorship
This project was supported by the Koning Corporation's grant from the U.S. Army Medical Research and Material Command, Grant W81XWH-09-1-0441.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/1/199055.
References
- The cost-effectiveness of fine-needle aspiration cytology and 14-gauge core needle biopsy compared with open surgical biopsy in the diagnosis of breast carcinoma. Cancer. 1998;82:1867-73.
- [Google Scholar]
- Percutaneous large-core breast biopsy: A multi-institutional study. Radiology. 1994;193:359-64.
- [Google Scholar]
- Impact of stereotaxic core breast biopsy on cost of diagnosis. Radiology. 1995;195:633-7.
- [Google Scholar]
- Multicenter study for the evaluation of a dedicated biopsy device for MR-guided vacuum biopsy of the breast. Eur Radiol. 2002;12:1463-70.
- [Google Scholar]
- Computed tomography for imaging the breast. J Mammary Gland Biol Neoplasia. 2006;11:103-11.
- [Google Scholar]
- Cone-beam CT for breast imaging: Radiation dose, breast coverage, and image quality. AJR Am J Roentgenol. 2010;195:496-509.
- [Google Scholar]
- Dedicated cone-beam breast computed tomography and diagnostic mammography: Comparison of radiation dose, patient comfort, and qualitative review of imaging findings in BI-RADS 4 and 5 lesions. J Clin Imaging Sci. 2012;2:7.
- [Google Scholar]
- Fast MRI-guided vacuum-assisted breast biopsy: Initial experience. AJR Am J Roentgenol. 2003;181:1283-93.
- [Google Scholar]
- MRI-guided 9-gauge vacuum-assisted breast biopsy: Initial clinical experience. AJR Am J Roentgenol. 2005;185:183-93.
- [Google Scholar]
- Detection of occult foci of breast cancer using breast-specific gamma imaging in women with one mammographic or clinically suspicious breast lesion. Acad Radiol. 2010;17:735-43.
- [Google Scholar]
- The positron emission mammography/tomography breast imaging and biopsy system (PEM/PET): Design, construction and phantom-based measurements. Phys Med Biol. 2008;53:637-53.
- [Google Scholar]
- Evaluation of malignant breast lesions in the diagnostic setting with cone beam breast computed tomography (Breast CT): Feasibility study. Breast J. 2014;20:364-74.
- [Google Scholar]






