Translate this page into:
Aneurysmal Bone Cyst of the Calcaneus
Address for correspondence: Dr. Veysel Kaplanoğlu, Department of Radiology, Ankara Keçiören Training and Research Hospital, TR-06100, Ankara, Turkey. E-mail: hatice.altnkaynak@yahoo.com.tr
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aneurysmal bone cysts (ABCs) are benign, non-neoplastic, expansile, vascular, locally destructive lesions. The lesion may arise de novo (65%) or secondarily (35%) in pre-existing benign or malignant lesions (giant cell tumor, osteoblastoma, chondroblastoma, angioma, and others). The calcaneus is a rare localization for ABC, comprising only 1.6% of the cases. In this paper, we present a case of a female patient with a 3-month history of heel pain that got worse and was accompanied by swelling and difficulty in walking. The magnetic resonance images of the postero-lateral calcaneus showed a contrast-enhanced cystic lesion located in the medullary cavity; exophytic portion of the tumor extended into the soft tissue causing distinctive cortical thinning. Heterogeneous hyperintense septae formations and blood level components were also detected. After correlation with pathology results, the lesion was diagnosed as an ABC. Since an ABC of the calcaneus is a rarely seen phenomenon, we present the radiologic findings in this case and a review of the literature.
Keywords
Aneurysmal bone cyst
benign bone lesions
calcaneus
INTRODUCTION

Aneurysmal bone cysts (ABCs) account for 1% of primary bone tumors. They are more common in women than in men (1.04:1).[1] Eighty-five percent of the cases are younger than 20 years, very rarely being under the age of 5 years or over 50 years of age.[2] The average age of calcaneal ABC is 24 years.[3] ABCs are non-malignant vascular lesions.[1] The lesion may arise as a primary lesion (65%) or secondary (35%) to pre-existing benign or malignant lesions (giant cell tumor, osteoblastoma, angioma, and frequently in the chondroblastoma of the calcaneus, but in rare cases in fibrous dysplasia, chondromyxoid fibroma, simple bone cyst, fibrous histiocytoma, eosinophilic granuloma, radiation osteitis, osteosarcoma, trauma, and fibrosarcoma).
Despite being reported in almost every bone of the body, it is most commonly encountered on the metaphyses of the long bones, especially on the distal part of the femur, proximal part of the tibia, and the vertebrae.[24] Calcaneus is a rare localization, comprising 1.6% of ABCs.[4] Therefore, we present our case where the lesion was diagnosed as ABC and provide radiography, ultrasonography (US), computerized tomography (CT), and magnetic resonance imaging (MRI) findings.
CASE REPORT
A 17-year-old female patient presented with a 3-month history of pain in her left heel. However, the pain had increased in the preceding 2-3 weeks. She had developed edema, and found it difficult to walk. The patient did not have any history of trauma or infection. On the lateral foot X-ray, there was an expanding radiolucent mass on the postero-lateral part of the calcaneus [Figure 1]. CT scan showed a lytic lesion with soft tissue density leading to erosion and expansion of the bone cortex, located on the postero-lateral part of the calcaneus [Figure 2]. MRI showed a cystic mass lesion on the postero-lateral part of the calcaneus. The lesion was causing prominent cortical thinning and destruction. It was located in the medullary cavity, and on the T2-weighted (T2W) sequence, a significant hypointense sclerotic rim surrounding the medullar component was visible. The T1-weighted (T1W) sequence showed heterogeneous hyperintense septae formations. T2W MRI also revealed heterogeneous hyperintense septae formations, blood level components, with contrast enhancement on the surrounding tissue and septae [Figure 3]. A surgical curettage and bone grafting was performed. On microscopic evaluation, cavernous cavities of different dimensions filled with blood without endothelial sequence and separated by collagenous tissue were seen throughout the specimen. The cavernous cavities contained fibroblasts, macrophages, and osteoclastic giant cells. The patient was diagnosed with ABC.

- 17-year-old female with pain in the left heel diagnosed as due to an aneurysmal bone cyst. Lateral X-ray of the left foot shows radiolucent lesion (arrow) leading to expansion on the postero-lateral part of the calcaneus.

- 17-year-old female with pain in the left heel diagnosed as due to an aneurysmal bone cyst. CT scans of the left foot a) sagittal and b) coronal views show lytic mass lesion (arrow), 35 × 25 mm in dimension, localized postero-laterally, leading to cortical bone erosion, expansion, and destruction.
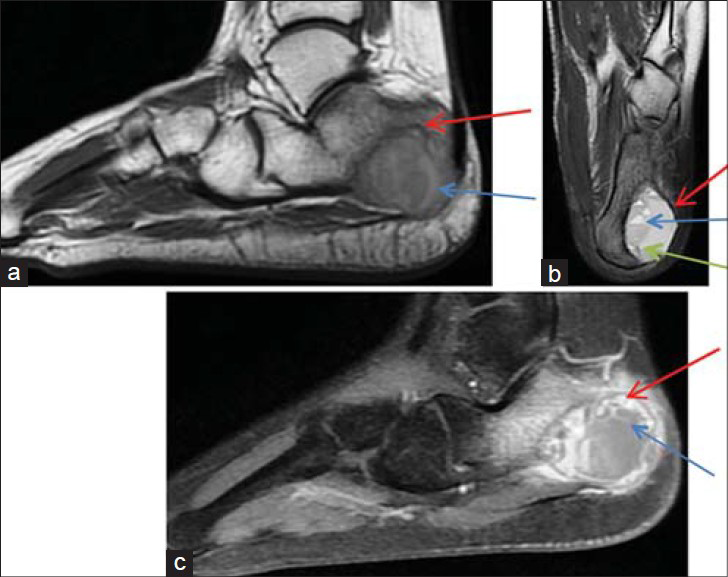
- 17-year-old female with pain in the left heel diagnosed due an aneurysmal bone cyst. MRI on the postero-lateral part of the calcaneus shows a cystic mass lesion in the medullary cavity. a) T1W and b) T2W sequences show heterogeneous hyperintense sclerotic rim (red arrow) surrounding the medullar component and central heterogeneous hyperintense septae formations (green arrow). T2W sequence shows blood level components (blue arrow). c) Image following intravenous contrast media administration shows contrast enhancement surrounding the lesion (red arrow) and in the septae formations (blue arrow).
DISCUSSION
An ABC was first described in 1893, with the first histological description given in 1925. The term “aneurysmal bone cyst” was first used in 1942 by Jaffe and Lichtenstein on ABC lesions seen on direct radiographic images.[3] An ABC is classified as a primary lesion or a secondary lesion. Pre-existing arteriovenous malformations are of the primary type and are seen in children. A history of accompanying lesion or trauma is not present in children. However, in adults, a history of trauma is present. The secondary type is accompanied by cyst, tumor, and degeneration of fibro-osseous lesion.[2] Eighty-five percent of the cases are under 20 years of age. It is very rarely seen in patients younger than 5 years or older than 50 years of age, because it appears in bones that continue growing. Primary ABC (65%) is seen in children and adolescents.[3] According to the literature, the mean age of ABC of the calcaneus is 24 years.[3] It is more common in females than in males (1.04:1).[1]
Despite being reported in almost every bone of the body, it is commonly encountered in the metaphyses of the long bones, especially the distal part of the femur, proximal part of the tibia, and vertebrae.[24] Sixty percent of the cases originate from metaphyses, while 28% originate from the meta-epiphyseal and subchondral parts.[3] ABC comprises about 1% of primary bone tumors.[125] According to reports in the literature, ABC is rarely seen on the calcaneus, which comprises approximately 1.6% of all ABCs.[4] An ABC located on the calcaneus is often symptomatic with patients mostly presenting with heel pain after minor trauma, walking discomfort, and sometimes swelling. Heel pain is often of a chronic nature and worsens with time following the trauma. Fractures of the calcaneus are rare. Nonspecific clinical findings give rise to a suspicion of ABC and the diagnosis is primarily made radiologically.[4]
On X-ray, ABC is seen as an expansile osteolytic lesion causing cortical thinning or destruction of the calcaneus, as in our case.[4] It is an eccentrically placed foamy-shaped lesion, widening the periosteum with the border of the thin cortical roof usually being preserved.[14] CT is useful to display the anatomical integrity of the lesion on the calcaneus. An ABC is usually seen as cortical erosion; however, in our case, no cortical erosion was seen on X-ray, but it was evident on the CT. The lesion density helps differentiate the cavity. Densities over 70 Hounsfield Units (HU) may represent solid lesions such as fibrous dysplasia. The image of blood and serum as a layer of fluid-fluid level is also defined as a feature of ABC. The densities of these layers vary between 16 and 47 HU.[1] The MRI images of ABC on T1 and T2 typically show a non-homogenous cystic lesion and multiple fluid-fluid levels surrounded by a rim with low signal.[4] The fluid-fluid levels are better evaluated on a T2W MRI. In the current case, the fluid-fluid levels and internal septae were also visualized better on MRI. Fluid-fluid levels may also be seen in giant cell tumors, telangiectatic osteosarcomas, and chondroblastomas. The patient's age, localization of the lesion, and radiological images of the lesion can be of help in differential diagnosis. Ultrasound can be of help when showing fluid-fluid levels.[1] In the case reported here, a complex lesion containing fluid-fluid levels, formation of septae, and solid fields were seen.
In the differential diagnoses of calcaneal ABC, simple bone cyst, chondroblastoma, and rarely, osteosarcoma are considered. Simple bone cysts that are not seen often in the body are very commonly encountered as benign tumors/tumor-like lesions of the calcaneus, comprising 41% of these lesions. They are asymptomatic and incidentally encountered on X-ray images.[4] Chondroblastomas are rarely encountered benign lesions, comprising 15% of the secondary ABC cases. This relation is important because the relapse of chondroblastoma in the presence of ABC is approximately 100%. Chondroblastoma is more often seen in the long bones and only 7% of the cases are calcaneal. Pain is a common feature. On imaging, lesion with good margins surrounded by reactive bone and calcification is seen.[3] Osteosarcoma is rarely encountered, and this is important in differential diagnosis. It is found in similar age group as ABC and the symptoms are also similar. On X-ray, in particular, telangiectatic osteosarcoma may imitate ABC and biopsy is crucial for definite diagnosis since this condition is much more aggressive and has a progressive course.[4]
CONCLUSION
Even though the calcaneus is a rare localization for an aneurysmal bone cyst, it should be considered in the differential diagnosis. For an appropriate diagnosis, correlation of the clinical presentation, anatomical localization, radiological profile, and histological evaluation are required.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/60/143732
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Aneurysmal bone cyst: Concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol. 1995;164:573-80.
- [Google Scholar]
- Pathologic fracture of a calcaneal aneurysmal bone cyst. J Foot Ankle Surg. 2011;50:727-32.
- [Google Scholar]
- Treatment of pelvic aneurysmal bone cysts in two children: Selective arterial embolization as an adjunct to curettage and bone grafting. Diagn Interv Radiol. 2007;13:49-52.
- [Google Scholar]






