A case of spinal melorheostosis

*Corresponding author: Alban Wei Shern Leong, Trust Grade, Watford General Hospital, Vicarage Rd, Watford, WD18 0HB, Hertfordshire, United Kingdom. alban.leong@nhs.net
-
Received: ,
Accepted: ,
How to cite this article: Leong AWS, Langdon J, Malhotra V, Mandalia U. A case of spinal melorheostosis. J Clin Imaging Sci 2022;12:8.
Abstract
Melorheostosis is a rare bone dysplasia of unknown etiology with an incidence of 0.9 cases per million. It typically affects the upper or lower limbs and can cause severe deformity and functional impairment. Diagnosis is radiological and is often described as a “flowing candle wax” appearance on the radiograph. Treatment is individualized depending on the site and severity of symptoms. We report a rare case of spinal melorheostosis. We demonstrate the imaging features of melorheostosis on CT and MRI. We discuss the classification, genetics, and management of this condition.
Keywords
Melorheostosis
Asymptomatic
MAP2K1
INTRODUCTION
Melorheostosis is a rare bone dysplasia that was first described by Leri and Joanny in 1922, with an incidence of 0.9 cases per million.[1,2] The disease affects both men and women equally, with symptom onset during childhood or adolescence.[3] It is regarded as a disease of unknown etiology and was previously suggested that a LEMD3 mutation can result in disorders that increase bone density, including melorheostosis.[4] However, a more recent genetic study done in 2018 identified somatic mosaic MAP2K1 oncogene mutations in affected bones of eight patients with melorheostosis. Furthermore, four of the five patients with overlying skin lesions also had mosaicism detected in the skin.[5] Clinical presentation can vary depending on the site, extent, and whether there is an associated soft tissue or joint involvement, and not all patients are symptomatic.
We present a case of spinal melorheostosis in the lower thoracic spine involving the T10 and T11 vertebrae. Melorheostosis typically affects the upper or lower extremities, and it is unusual for it to affect the spine.[6] There have been a few case reports of melorheostosis of the spine, and some of these patients presented with myelopathy or radiculopathy features.[7,8] Our patient, however, was incidentally diagnosed and did not have any clinical features to suggest a diagnosis of melorheostosis.
CASE REPORT
A 41-year-old lady first presented to the hospital with right upper quadrant pain and vomiting. She has a past medical history of asthma, for which she was on regular Salbutamol and Beclometasone inhalers. Blood tests showed deranged liver function tests with a bilirubin of 38, alanine aminotransferase of 234, and alkaline phosphatase of 50. Albumin and International Normalised Ratio were normal. Adjusted calcium 2.39 mmol/L, Phosphate 0.9 mmol/L, Urea 4.1 mmol/L, Creatinine 66 µmol/L, Potassium 4.2 mmol/L, Sodium 141 mmol/L, C-Reactive Protein 11 mg/L. She had a CT abdomen and pelvis on admission which showed gallstones in the gallbladder and distal common bile duct. She was treated with a short course of antibiotics, following which, she underwent an uneventful ERCP and laparoscopic cholecystectomy.
Her CT abdomen and pelvis incidentally showed a dense sclerotic lesion at T10 and T11 with involvement of the costovertebral joint at that level and the adjacent ribs [Figures 1A–G]. The patient was asymptomatic with regards to the lesion, with no restriction of movement, and no associated radiculopathy. There was no joint deformity or overlying skin changes. The lesion was considered indeterminate but likely benign as it had a narrow zone of transition, showed no evidence of bone destruction and no periosteal reaction. One of the differentials for this appearance was sclerotic metastases, as a result, a CT scan of her neck and chest was performed to complete staging workup. There was no evidence of underlying malignancy on imaging. The findings were discussed at the spinal multidisciplinary meeting, and the nodular exostoses and dense sclerosis were considered characteristic of the flowing candle wax appearances of melorheostosis. An MRI scan was subsequently performed which showed the lesion to be dense sclerotic in nature with no evidence of associated edema or soft tissue component. The appearances were considered typical of melorheostosis and as the patient was asymptomatic no further investigation or treatment was considered at this stage.
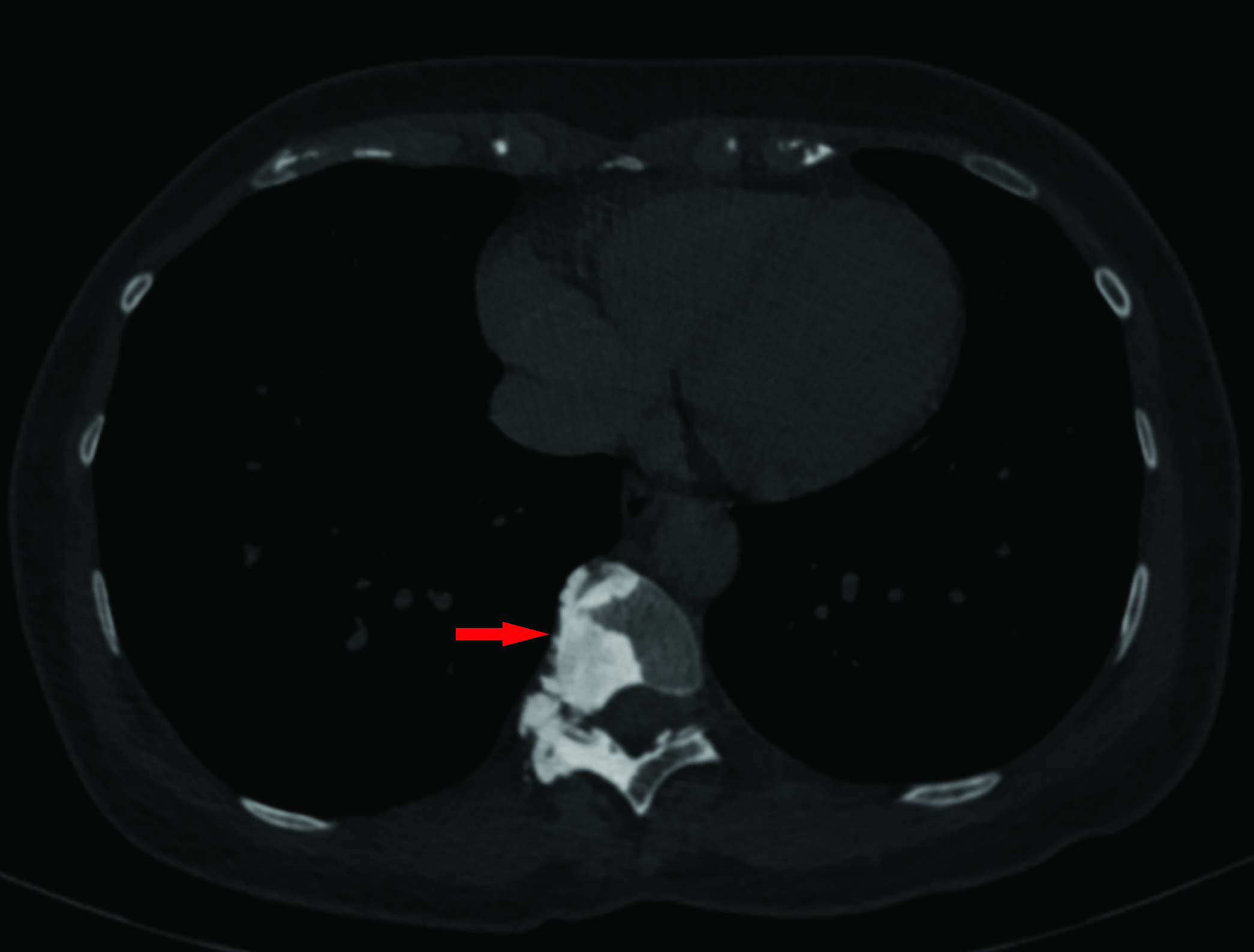
- Axial CT image of the thorax in bone windows, showing a dense osteosclerotic lesion eccentrically located to the right of the T10 vertebral body with involvement of the right lamina. There is associated bone expansion with narrowing of the right neural exit foramen.
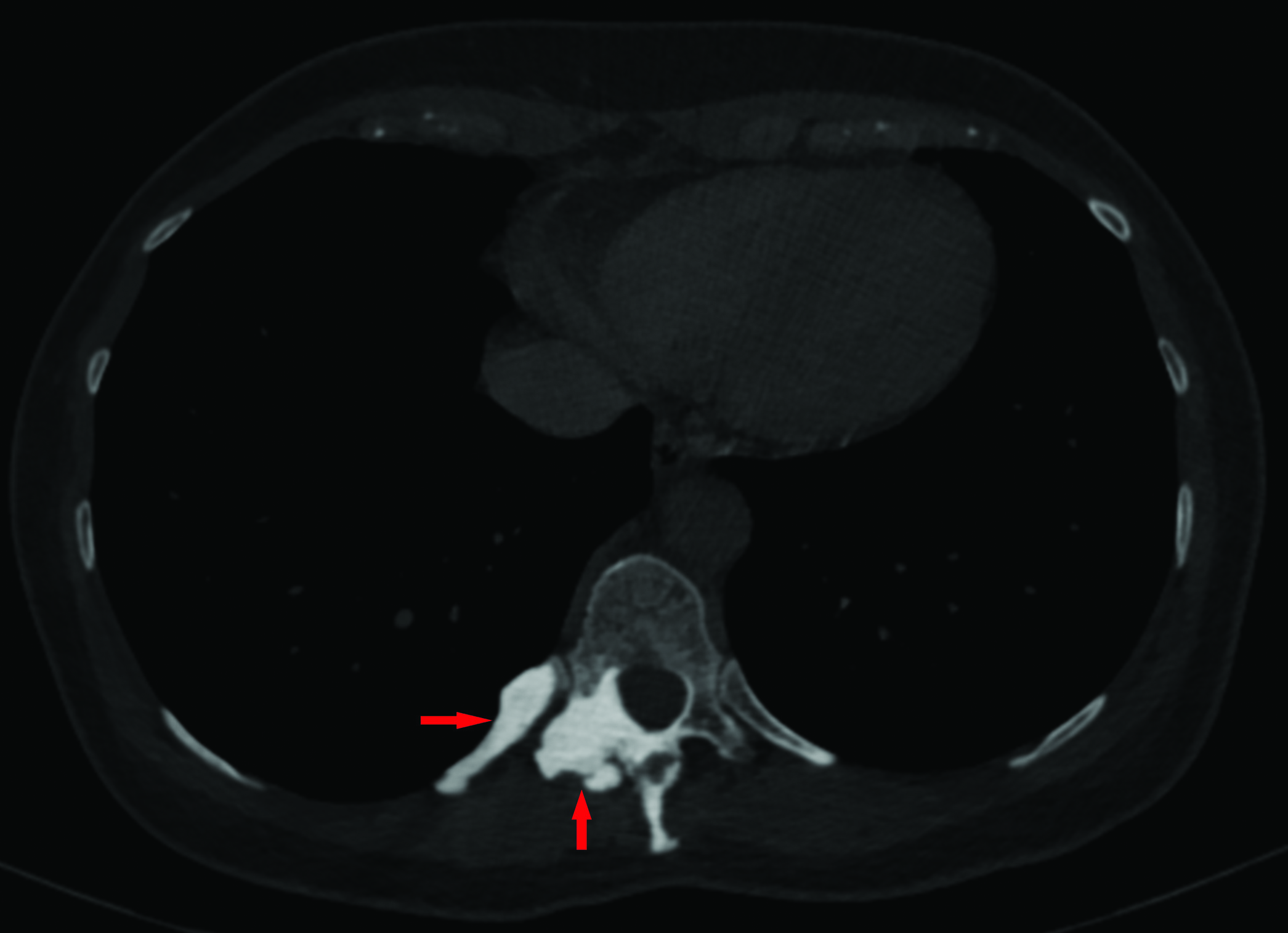
- Axial CT image at a lower position compared to Figure 1A, also in bone windows, shows dense sclerotic changes also involving the adjacent T10 rib.

- Sagittal CT image of the lower thorax, in bone windows, demonstrates contiguous osteosclerotic changes of the T10 and T11 vertebral bodies with mild bone expansion of the spinous process of T11.
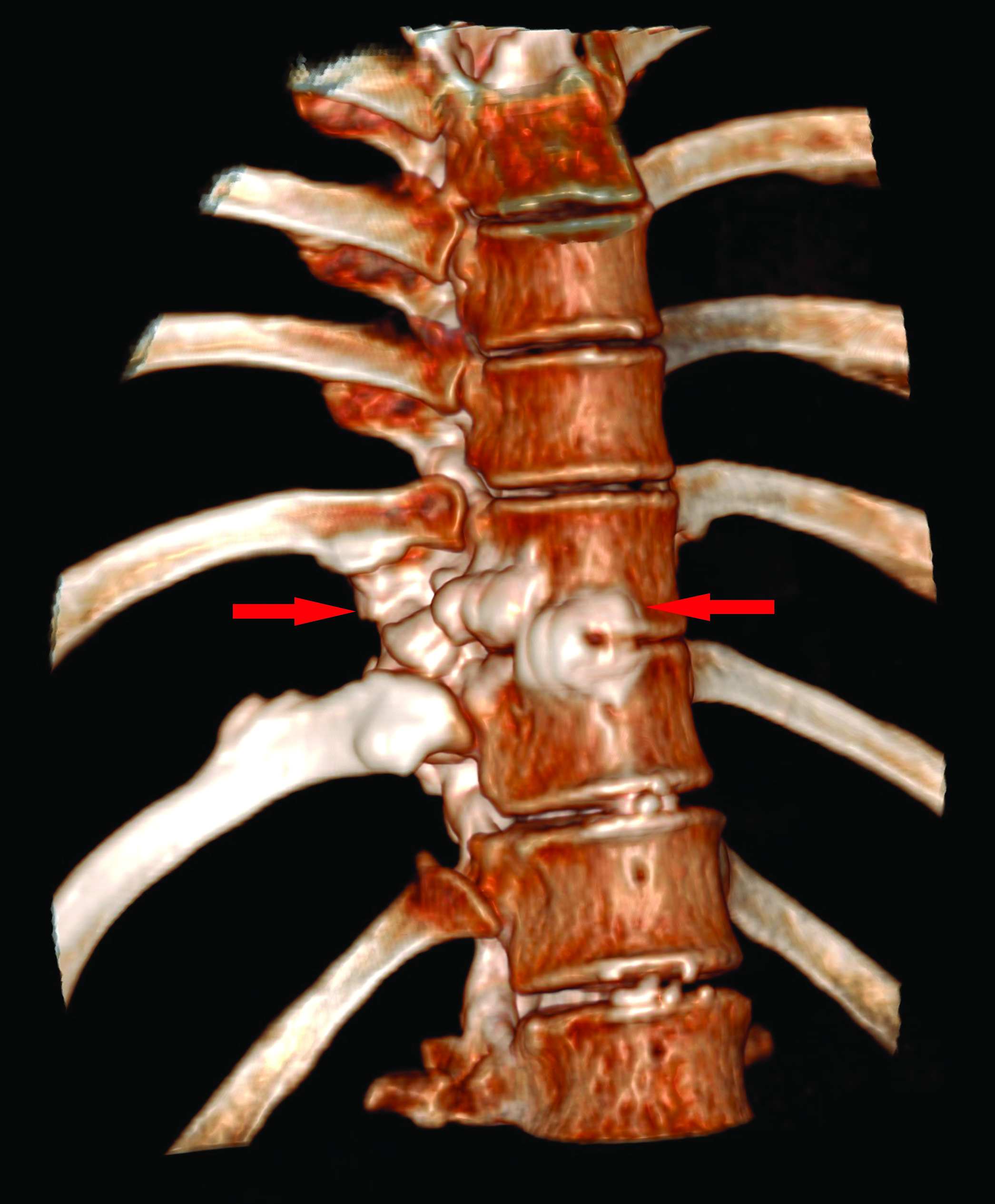
- Volume rendered CT image of the lower thoracic spine, shows the bony expansion of the vertebral bodies and ‘dripping candle wax’ appearance of the vertebra.
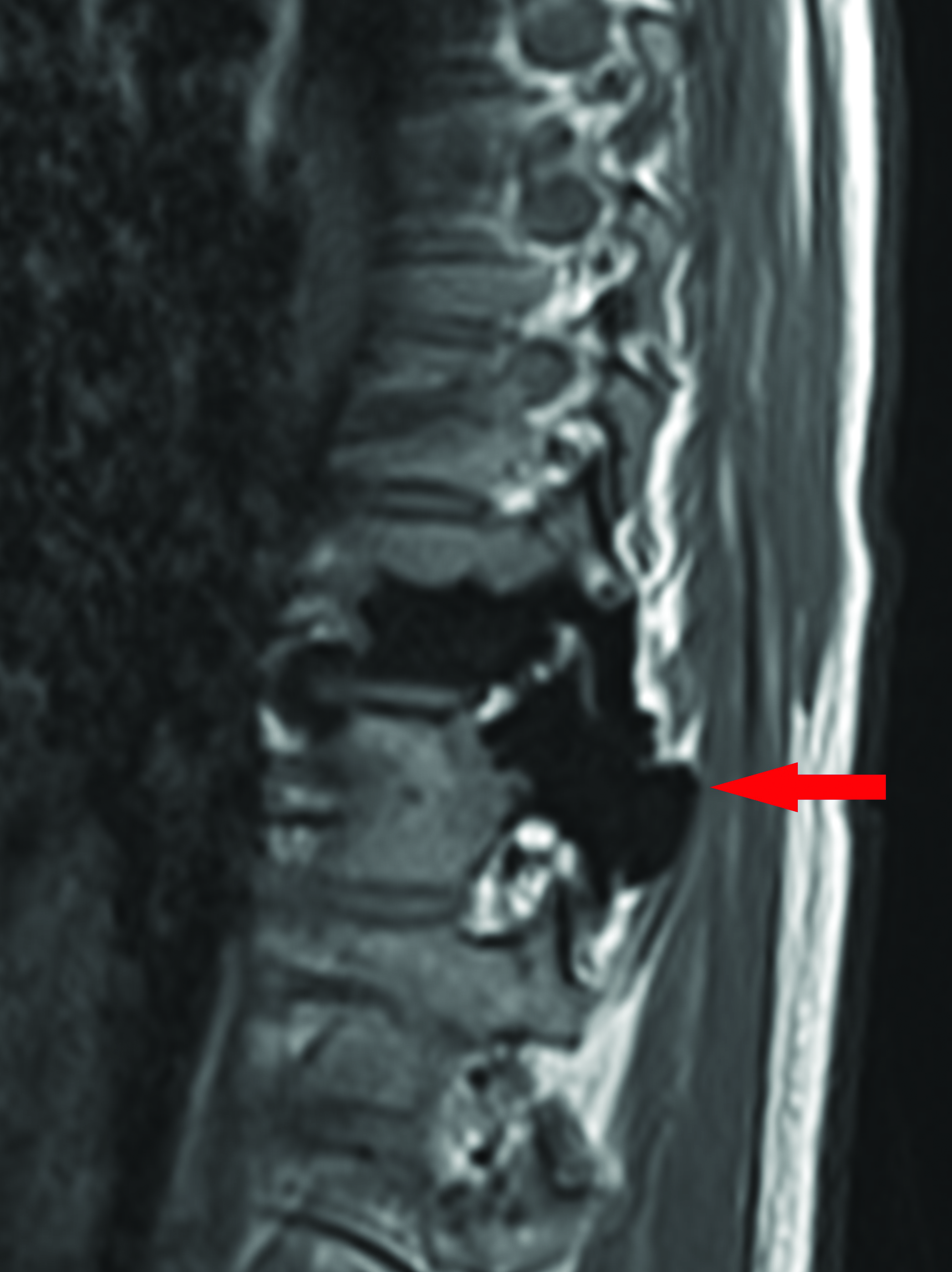
- Sagittal T1 weighted images of the lower thoracic spine, demonstrating low signal change in the spine on both sequences, Figure 1E and 1F, consistent with a dense osteosclerotic bone lesion. There is involvement of the posterior elements and evidence of mild expansion.

- Sagittal T2 weighted images of the lower thoracic spine, demonstrating low signal change in the spine on both sequences, Figure 1E and 1F, consistent with a dense osteosclerotic bone lesion. There is involvement of the posterior elements and evidence of mild expansion.
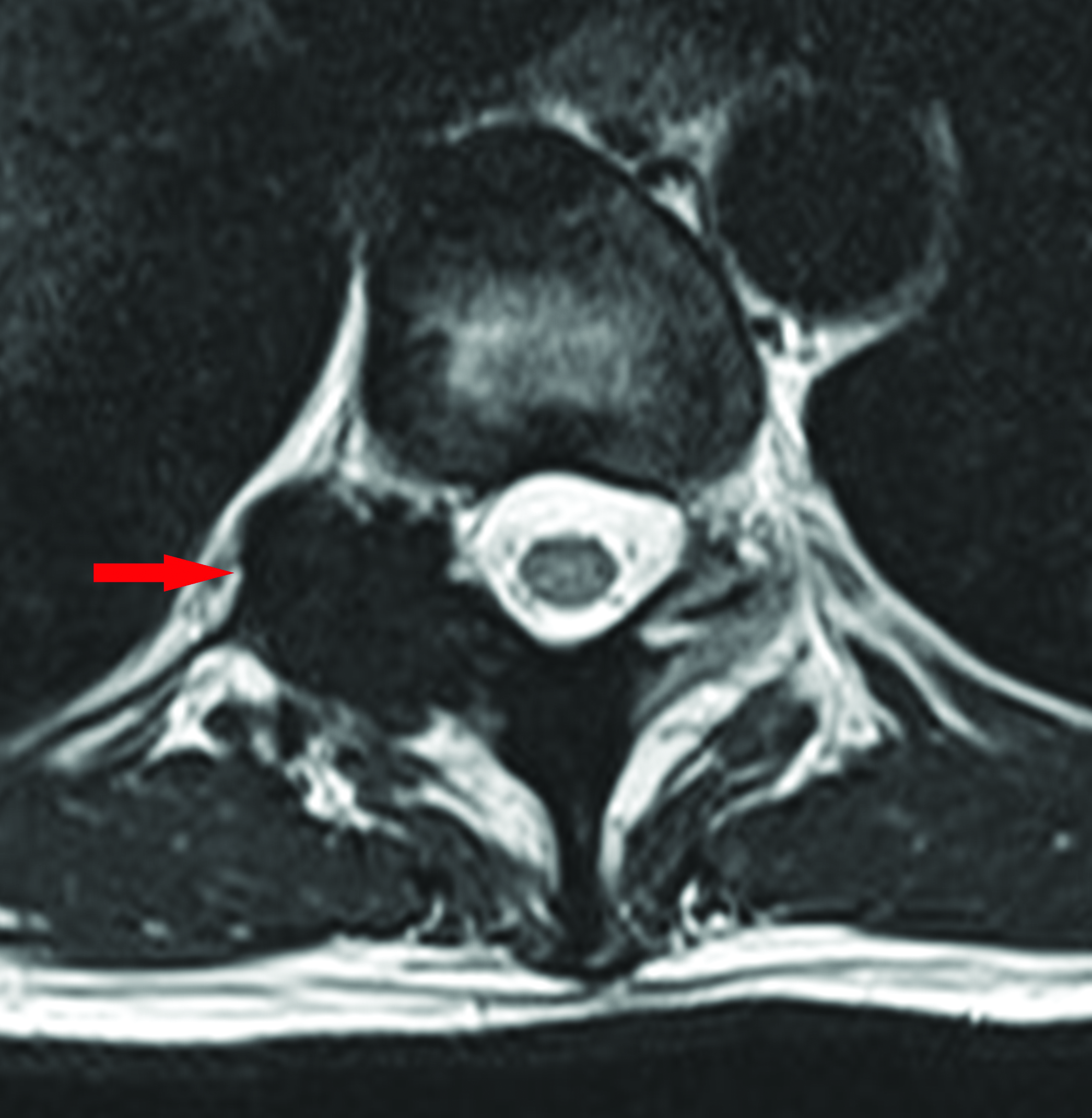
- Axial T2 weighted image at the level of the T10-11 disc, shows loss of signal in the right posterior elements of T11 with bony expansion and narrowing of the right neural exit foramen.
DISCUSSION
Melorheostosis is a rare bone dysplasia with an incidence of 0.9 cases per million.[2] There is insufficient data to support a specific ethnic predisposition. The etiology is unknown and was initially thought to be due to a LEMD3 mutation.[4] A more recent genetic study of the disease suggests that a MAP2K1 mutation leads to disease. Mutation of the MAP2K1 oncogene identified in affected individuals showed an increased MEK1 signaling activity, resulting in increased osteoblast proliferation.[5]
The disease has an insidious onset, and typically affects the appendicular skeleton.[6] Clinical features include asymmetry of the affected limbs, vascular anomalies, abnormal skin pigmentation, muscle contractures, and wasting and sclerodermatous lesions over the bony lesions.[9,10] Histological features are not identical in all cases, but they include dense bone without distinctive cellular abnormalities, variable degrees of cortical thickening, adjacent fibrocartilage with irregular surface fibrillation, and more rarely a cartilage cap. Soft tissue components include osseous, chondroid, vascular, and fibrocartilaginous tissue substrates.[10]
Radiologically, melorheostosis is classically described as dense cortical longitudinal hyperostosis of the affected bone and has the classical features of a “flowing candle wax” appearance.[9,11] While a diagnosis can usually be reached through plain radiographs or computerized tomography, there have been some cases that report increased metabolic activity on nuclear imaging.[12] If there is any diagnostic doubt, nuclear imaging has the added advantage of differentiating melorheostosis from other bone dysplasias such as osteopoikilosis and osteopathia striata - melorheostosis showed focal increased uptake in involved bones that isn’t present in the other two bone dysplasia.[13] For patients who have been diagnosed with melorheostosis, we do not recommend extensive imaging of other parts of the body that do not exhibit symptoms as this would lead to excessive radiation exposure, particularly in the context of benign lesions. However, in the context of multiple bone lesions, nuclear medicine studies may be appropriate for identifying all the affected regions. One of the reasons for presenting this case is to illustrate the features of this benign condition to obviate the need for further investigation. We hope for radiologists to feel more confident in making diagnoses of benignity.
A review of 23 cases of melorheostosis further subdivides the radiological features into five different types. Type A: Osteoma-like appearance. Type B: (Classic) Dripping or flowing candle wax. Type C: Predominant myositis ossificans-like pattern. Type D: Osteopathia striata-like pattern. Type E: Mixed pattern. Of these, only five of the 23 cases displayed the classical features.[6] Our patient did have the classical appearance, hence it falls into the Type B category.
Treatment revolves around symptomatic relief and should be individualized depending on the age, site, and extent of disease. This involves physiotherapy, analgesia, bisphosphonates, manipulation, casting, braces, and nerve blocks. In more severe cases, surgical intervention can be considered to relieve the pressure exerted by abnormal bone or to correct limb length and restore function.[10,11] In other case reports of spinal melorheostosis, those patients had severe symptoms that eventually required surgical decompression. These patients went on to have good functional recovery with improvement of symptoms.[7,8] It is also interesting to consider targeted MEK1 inhibition in the future as a potential treatment option.[5] Although our patient did have significant foraminal narrowing caused by bone overgrowth, she did not complain of neuropathic symptoms. This may be due to the slow-growing chronic nature of the abnormality or the site of the lesion within the thoracic rather than lumbar spines. Hence, she was treated conservatively with clinical monitoring under orthopedics.
CONCLUSION
Spinal melorheostosis is an unusual occurrence as melorheostosis typically affects the upper or lower limbs. This case report presents a patient in her early forties who had incidental T10 and T11 melorheostosis. Melorheostosis is typically described to have a flowing candle wax appearance, which was exhibited in this case. She did not require any treatment as she was asymptomatic.
Declaration of patient consent
Patient consent is not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Une afection non décrite des os hyperostose “en coulée” sur toute la longeur d’un member ou “melorhéostose”. Bull Mem Soc Med Hop Paris. 1922;46:1141-45. French
- [Google Scholar]
- Severe Melorheostosis Involving the Ipsilateral Extremities. Clin Orthop Relat Res. 2009;467:2738-43.
- [CrossRef] [Google Scholar]
- Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet. 2004;36:1213-18.
- [CrossRef] [PubMed] [Google Scholar]
- Somatic activating mutations in MAP2K1 cause melorheostosis. Nat Commun. 2018;9:1390.
- [CrossRef] [PubMed] [Google Scholar]
- Melorheostosis: a review of 23 cases. Eur Radiol. 2001;11:474-79.
- [CrossRef] [PubMed] [Google Scholar]
- Melorheostosis causing lumbar radiculopathy: a case report and a review of the literature. Spine J. 2013;13:27-29.
- [CrossRef] [PubMed] [Google Scholar]
- Myelopathy associated with melorheostosis: A case report. Arch Phys Med Rehabil. 2005;86:1495-97.
- [CrossRef] [PubMed] [Google Scholar]
- Grainger & Allison’s Diagnostic Radiology Vol 1. (5th ed). Netherlands: Elsevier; 2020.
- [Google Scholar]
- Melorheostosis: Clinicopathological features, diagnosis, and management. Orthopedics. 2009;32:512..
- [CrossRef] [PubMed] [Google Scholar]
- The dripping candle wax sign of melorheostosis. SAGE Open Med Case Rep. 2020;8:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Extensive melorheostosis of the ribs demonstrated on 18F-Fluoride PET/CT. Eur J Nucl Med Mol Imaging. 2014;42:533-34.
- [CrossRef] [PubMed] [Google Scholar]
- 99mTc-Pyrophosphate bone imaging in osteopoikilosis, osteopathia striata, and melorheostosis. Radiology. 1978;127:439-43.
- [CrossRef] [PubMed] [Google Scholar]
- Melorheostosis and osteopoikilosis: A review of clinical features and pathogenesis. Calcif Tissue Int. 2019;104:530-43.
- [CrossRef] [PubMed] [Google Scholar]






