Translate this page into:
Stent graft for a longstanding femoral artery pseudoaneurysm with arteriovenous fistula– A case report of the first infra-inguinal application of the upside-down gore excluder limb technique
-
Received: ,
Accepted: ,
How to cite this article: Premnath KPB, Saleh AT, Elsakhawy M, Kutlay M, Jacob S. Stent graft for a longstanding femoral artery pseudoaneurysm with arteriovenous fistula–A case report of the first infra-inguinal application of the upside-down gore excluder limb technique. J Clin Imaging Sci 2022;12:7.
Abstract
Pseudoaneurysm with arteriovenous fistula is a rare presentation of penetrating trauma, occurs when trauma involves major blood vessels, and is traditionally treated surgically. Recently, these are more commonly treated using endovascular techniques which include stent graft placement and parent artery occlusion. In this case report, we present a case of femoral artery pseudoaneurysm and arteriovenous fistula with severe size difference between the arterial segments proximal and distal to the fistula site, treated successfully by using the upside-down gore excluder limb technique.
Keywords
Arteriovenous fistula
Upside-down technique
Stent graft
INTRODUCTION
Penetrating trauma causing arterial wall disruption can cause a pseudoaneurysm. Additional injury of or pseudoaneurysm rupture into an adjacent vein can result in an arteriovenous fistula. Long-standing arteriovenous fistula can cause dolichoectasia of arteries proximal to the fistula and the draining veins; venous hypertension which may present with edema, varicose veins, stasis dermatitis, and venous ulceration; claudication; and high output cardiac failure.[1-3] Arterial injuries are treated most commonly with endovascular techniques which are less invasive than surgery and can be performed fairly easily under local anesthesia.[1,4] Vessel size difference at stent graft landing zones due to aneurysmal dilatation of supplying artery and reduced blood flow to distal vessels, if severe, can render the fistula unsuitable for endovascular stent-graft placement. Also, accessing the lesion using a contralateral retrograde femoral access can be very difficult or impossible when there is severe tortuosity of the supplying artery. In this case report, we present the treatment of a longstanding difficult femoral artery arteriovenous fistula with pseudoaneurysm using the upside-down Gore excluder limb technique, the infrainguinal usage of which has not been described previously.
CASE REPORT
A 60-year-old gentleman was referred to vascular surgery by the general practitioner with complaints of swelling and gradually increasing abnormal pulsation in the left mid-thigh, which the patient started to notice 4 years back. The patient also complained of palpitations on and off and gradually progressing calf claudication of moderate severity for the last 2 years. There was a history of penetrating trauma to the left mid-thigh 35 years back. On examination, the patient had an ill-defined pulsatile bulge in the medial aspect of the left thigh. There were no signs of venous stasis. His basal pulse rate was 96 beats per minute and blood pressure was 160/90 mm Hg.
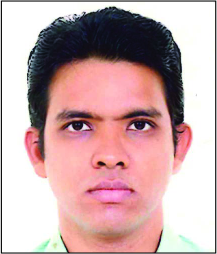
CT angiogram of the lower limbs showed a left mid-femoral artery large pseudoaneurysm measuring 4.2 cm draining into the adjacent femoral vein, severe tortuosity, and aneurysmal dilatation of the proximal iliofemoral arteries, and aneurysmal dilatation of the draining iliofemoral veins [Figure 1]. Arterial phase-contrast opacification of the distal femoral and proximal popliteal vein was seen in addition to the veins from the fistula site to the right atrium indicating deep venous reflux. The femoral artery proximal to the fistula site measured 14 mm in diameter and the artery distal to the fistula measured 7 mm. Also, at the level of the fistula, mid femoral extraosseous ossification representing chronic myositis ossificans was seen.
- A 60-year-old man with post-traumatic chronic femoral pseudoaneurysm with arteriovenous fistula. (a) CT angiogram of the pelvis and lower limbs 3D reformatted left anterior oblique view shows the pseudoaneurysm (asterisk), severely tortuous left common and external iliac arteries (white arrow), arterial phase opacified left lower limb veins. Also seen is an extraosseous left mid femoral ossified lesion at the site of the fistula representing myositis ossificans (arrowhead). (b) Curved multiplanar reformatted image of the femoral artery at the site of the pseudoaneurysm and fistula shows severe vessel size difference proximal and distal to the fistula site in the femoral artery measuring 14 and 7 mm in diameter respectively.
A tapered iliac limb extension used in endovascular aortic repair could be used to compensate for the vessel size difference. These extension grafts have a wide upper end and a tapered lower end. For this patient, we would need to deploy the stent-graft with tapered end inferiorly, which is possible by either introducing the stent-graft from a distal femoral or popliteal access or by inverting the graft before introduction to deploy it through antegrade femoral or retrograde contralateral femoral access. Popliteal access was not safe given that the graft would need a 12 F sheath, and a retrograde contralateral femoral access was not suitable since the tortuosity of the left iliac vessels would preclude navigation of the 12 F sheath and the rigid stent-graft to the fistula site; also standard 30–45 cm long sheaths which are designed to treat aortoiliac pathology would not be long enough to treat mid femoral disease through contralateral access. We chose to treat the fistula using left antegrade femoral access.
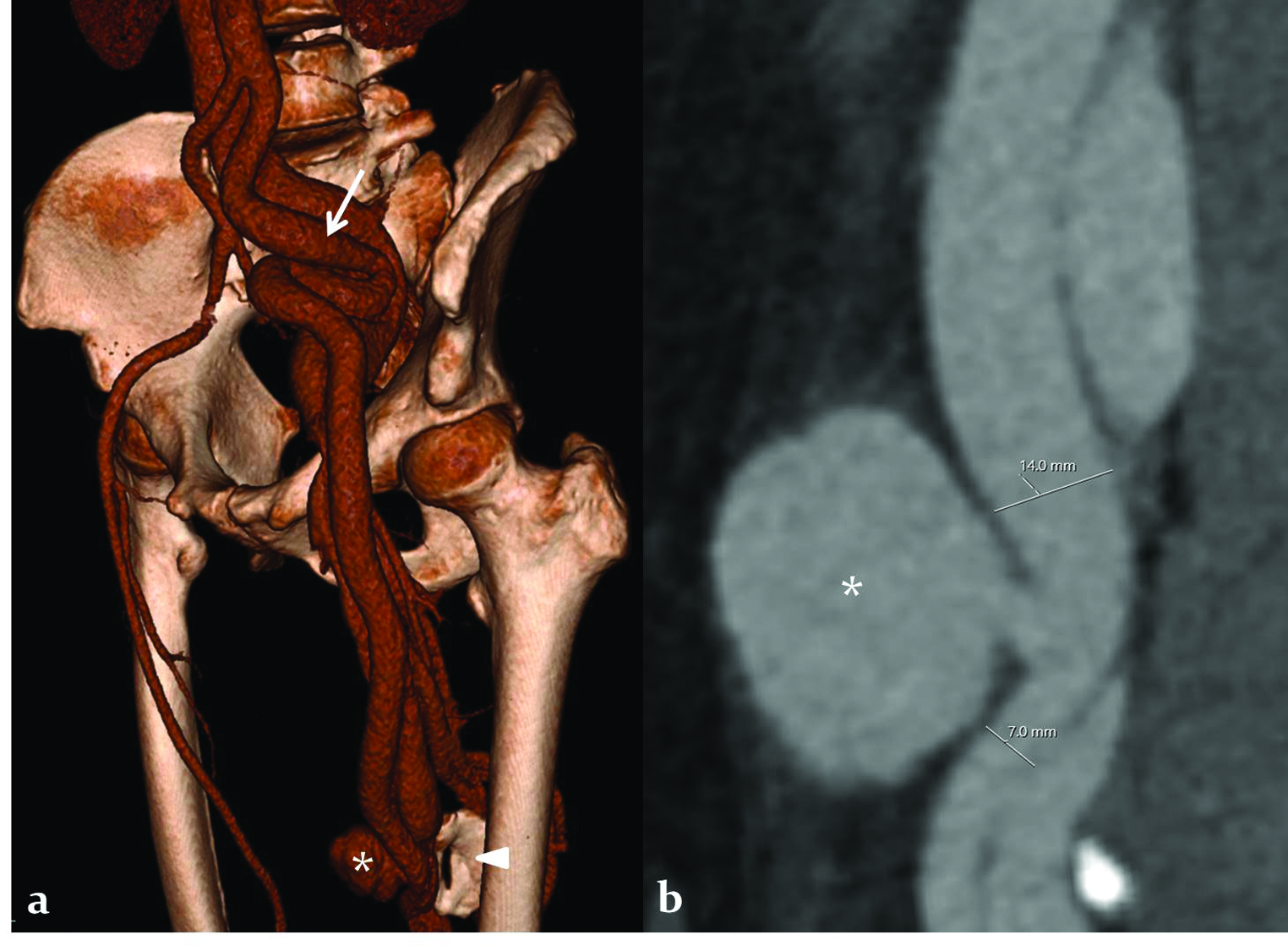
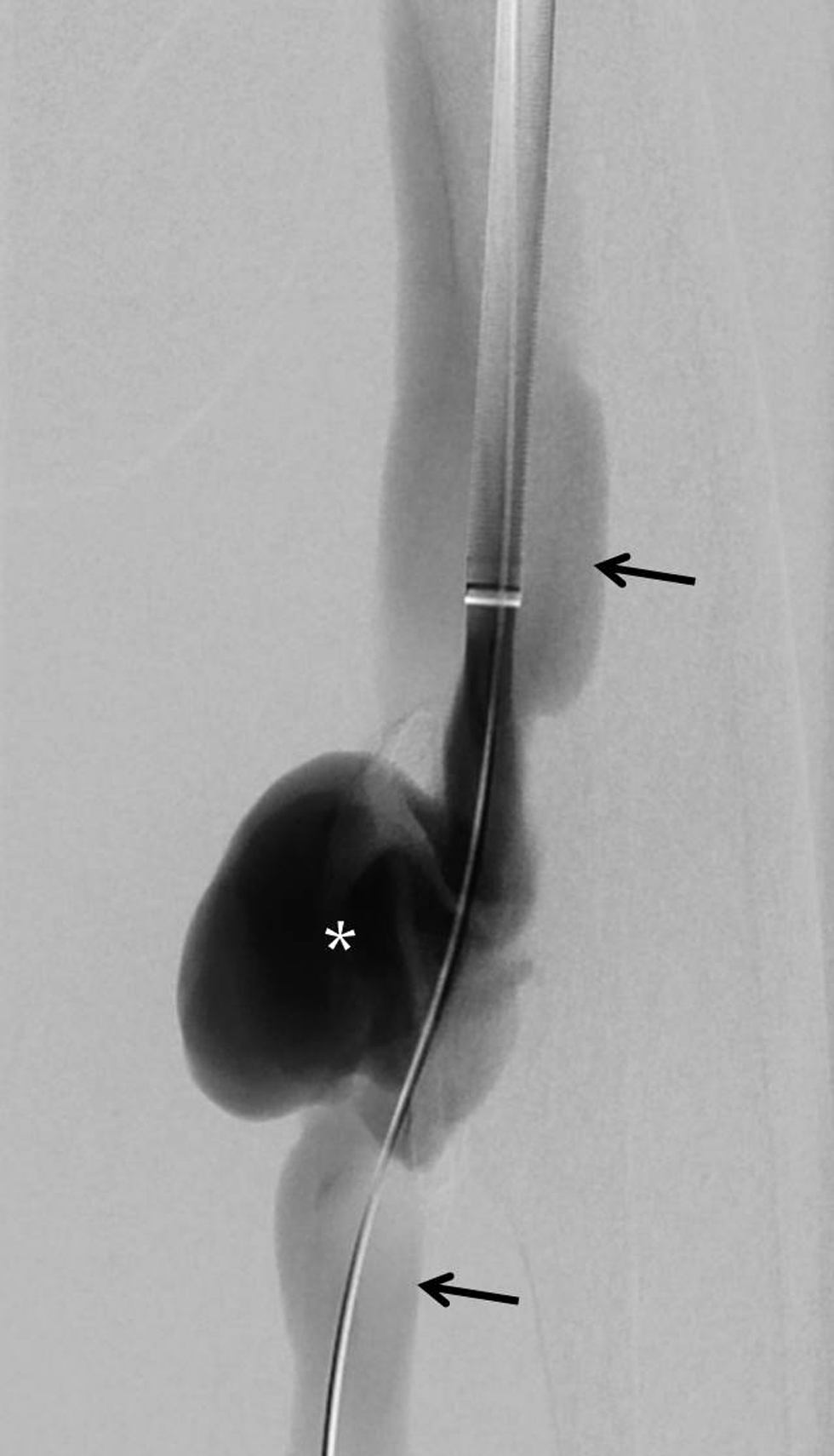
The patient was positioned supine, left femoral antegrade access was obtained and a 14 F sheath (W.L. Gore and Associates Inc.) was introduced antegrade after preparing the common femoral artery puncture site with two Perclose ProGlide sutures (Abbott Vascular, Redwood City, CA, USA). Digital subtraction angiogram confirmed the diagnosis of arteriovenous fistula and pseudoaneurysm. There was a severe steal phenomenon with no distal arterial blood flow [Figure 2]. The 14 F sheath was inserted till the distal end was inferior to the site of the fistula into the distal femoral artery. A 16–10 × 70 mm Gore Excluder stent-graft (W.L. Gore and Associates Inc., Flagstaff, AZ, USA) was used. The technique of inverting the stent-graft was the same as described previously in the literature.[5,6] The olive tip at the end of the stent-graft deployment system was detached by bending and breaking; the deployment line was cut close to the deployment knob after unscrewing the knob, and the stent-graft was slid off the delivery system. The stent-graft was inverted in such a way that the tapered tip was the advancing end, and inserted into the 16F sheath over a stiff guidewire. The stent-graft was positioned across the site of the fistula within the sheath by pushing it with a cut blunt end of the dilator of the 16F sheath, which was cut approximately 1 cm from the tip. The graft was deployed within the sheath by pulling the deployment suture, and then the graft was deployed across the fistula site by "unsheathing" it—keeping the graft stationary stabilizing it with the cut dilator, and pulling the sheath slowly over the dilator [Figure 3a,b]. Angiogram after stent graft deployment showed an endoleak [Figure 3c]. A coda balloon was used to achieve an optimal approximation of the stent-graft to the vessel wall. Post stent-graft deployment angiogram showed patent graft with good distal arterial flow, no opacification of the pseudoaneurysm, and no arteriovenous fistula [Figure 3d]. The patient had no claudication since the day after the procedure. One month after the stent-graft placement, the patient had a basal pulse rate of 78 beats per minute and blood pressure was 140/80 mm Hg. The patient had follow-up femoral Doppler studies at 3 and 6 months after the procedure and a CT angiogram of the lower limb 1 and 2 year after the procedure which showed optimal appearances with thrombosis and shrinkage of the pseudoaneurysm, patent stent graft, and no fistula.
- A 60-year-old man with post-traumatic chronic femoral pseudoaneurysm with arteriovenous fistula. Digital subtraction angiogram performed by contrast injection through the sheath showing the pseudoaneurysm (asterisk), antegrade and retrograde opacification of the veins (black arrows), and absent contrast flow in the arteries distal to the fistula site.
- A 60-year-old man with post-traumatic chronic femoral pseudoaneurysm with arteriovenous fistula. (a) Fluoroscopic image shows reversed Gore Excluder stent-graft (arrow head) pushed to the site of the fistula within the sheath (black arrows) by a cut-end dilator (white arrows). (b) Fluoroscopic image shows released Gore Excluder stent graft within the sheath. (c) Digital subtraction angiogram after deployment of the stent-graft at the site of the fistula shows a small contrast leak into the pseudoaneurysm (asterisk) and draining vein (arrows). (d) Post-procedure angiogram after modeling the stent-graft with a compliant balloon shows no residual leak, patent stent graft, and good flow to the femoral artery distal to the fistula (arrow).
DISCUSSION
Isolated traumatic pseudoaneurysms without arteriovenous fistula can be treated with prolonged manual compression, thrombin injection, or surgical repair. Pseudoaneurysms with or without an arteriovenous fistula involving an expendable artery can be treated with occlusion of the artery with embolic agents which can be coils, plugs, or liquid embolic agents like glue. These endovascular treatment options are not suitable for a pseudoaneurysm with an arteriovenous fistula involving a nonexpendable artery like the femoral artery. Endovascular treatment using a stent graft is considered an appropriate approach for such cases and is much more commonly performed compared to open surgical repair in most hospitals where such facilities are available.[1,4] Chronic fistula-induced changes including enlargement of veins, high flow high-velocity circulation, scarring from previous trauma, and presence of nerve damage can cause difficulty with surgical repair.[1-3] Covered stent placement across pseudoaneurysms or arteriovenous fistulas is known to be an easily performable procedure, has high technical success, and has low complication rates.[1,4]
Chronic fistula can cause stretching, tortuosity, and aneurysmal dilatation of the feeding vessel.[2,3] In the presence of a large-sized high flow fistula, there can be a steal phenomenon resulting in reduced flow to the circulation distal to the fistula, which may cause ischemic symptoms like claudication as in the case described. A combination of these factors can result in severe differences in vessel size proximal and distal to the fistula site which would be the stent-graft landing zones. Covered stents are available over a wide range of diameters and can be used with smaller vascular access sheaths of less than 8 F size; however, any particular self-expandable covered stent can be used only within a narrow range of vessel diameters. Overlapping stents of widely different diameters would result in excessive graft infolding, causing stenosis which may cause a permanent reduction in distal blood flow or gutter formation which may result in a leak between the grafts into the aneurysm/fistula. Also, no widely available covered stent is suitable for the large-sized feeding vessel as in the case described.
The only possible endovascular solution in our case was to use a tapered iliac extension stent graft which is commonly used as an iliac extension of limbs of endovascular aortic repair stent grafts. The stent graft had to be deployed from an ipsilateral antegrade femoral access with its tapered end caudal which would need reversal or turning upside-down of the stent-graft. Upside down stent-graft techniques have been described in aortoiliac pathologies with Gore excluder, Medtronic Endurant, and Cook Zenith iliac legs.[5-8] Upside down technique for Cook Zenith and Medtronic Endurant stent-grafts would need deployment of the stent-graft outside the body and re-sheathing the stent-graft into the deployment system which is cumbersome, increases operating time significantly, and could cause graft damage or stent fracture in the long term.[5,6] Gore Excluder stent-graft is constrained by a suture and is deployed by pulling on the suture line instead of unsheathing as in other grafts. So, the Gore Excluder iliac leg can be turned upside down without extracorporeal deployment making the procedure easy and less time-consuming.[5,6] With Gore Excluder stent-grafts, advancing end diameters from 10 to 23 mm can be achieved with a fixed end diameter of 16 mm. Upside down deployment is outside the standard instructions for use but is a good clinical skill to acquire and is documented to be very helpful in treating various aortic and iliac aneurysms where commercially available devices are inappropriate in either size or length.[5,6] The only disadvantage is the necessity of large vascular sheaths above 12 F size which require either a surgical cut down for access or vessel preparation with percutaneously placed suture based devices, compared to smaller sheaths lesser than 8F size suitable for most of the other covered stents available for peripheral arteries; however, these stents are not suitable for this patient due to aforementioned reasons.
CONCLUSION
To the best of our knowledge, upside-down deployment of stent-graft has not been described to treat infra-inguinal vessel pathology; and this technique is very useful for treating chronic high flow fistulas where there is severe vessel size difference proximal and distal to the fistula.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Endovascular stent graft for post-traumatic superficial femoral artery pseudoaneurysms with arteriovenous fistula: 6 months follow-up of 2 cases. J Radiol Case Rep. 2011;5:26-4.
- [CrossRef] [PubMed] [Google Scholar]
- Late complications of traumatic arteriovenous fistula. Am Surg. 1989;55:180-83.
- [PubMed] [Google Scholar]
- Traumatic arteriovenous fistula 52 years after injury. J Vasc Surg. 2010;51:1265-67.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular stent-graft treatment of traumatic arterial lesions. Ann Vasc Surg. 1999;13:121-29.
- [CrossRef] [PubMed] [Google Scholar]
- The upside down Gore Excluder contralateral leg without extracorporeal predeployment for aortic or iliac aneurysm exclusion. J Vasc Surg. 2011;53:1738-41.
- [CrossRef] [PubMed] [Google Scholar]
- The upside-down Gore Excluder limb and double-barrel sandwich technique for penetrating aortic ulcer and iliac aneurysm exclusion. Vasc Specialist Int. 2016;32:17-21.
- [CrossRef] [PubMed] [Google Scholar]
- The upside down Endurant iliac limb stent graft for treatment of a common iliac artery aneurysm. Vasc Endovascular Surg. 2014;48:58-60.
- [CrossRef] [PubMed] [Google Scholar]
- Use of the reversed Zenith iliac limb extension in the treatment of iliac artery aneurysms and various aortoiliac pathologies: outcome in midterm follow-up. J Endovasc Ther. 2011;18:762-67.
- [CrossRef] [PubMed] [Google Scholar]






