Translate this page into:
Hydronephrosis as an Unusual Cause of Acute Pancreatitis
Address for correspondence: Dr. Nata Pratama Hardjo Lugito, Department of Internal Medicine, Faculty of Medicine, Pelita Harapan University, Jendral Sudirman Boulevard, Lippo Karawaci, Tangerang, Banten - 15811, Indonesia. E-mail: nata.lugito@uph.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Acute pancreatitis is an inflammatory disease of the pancreas. The most common cause of acute pancreatitis is gallstone impacting the distal common bile–pancreatic duct (38%) and alcoholism (36%). There have been a few reports in the literature of acute pancreatitis associated with an obstructed urinary system. This case describes a 38-year-old male with acute pancreatitis occurring in the setting of hydronephrosis. A magnetic resonance cholangiopancreaticography (MRCP) showed right-sided severe hydronephrosis pushing the duodenum and head of pancreas anteriorly, thus obliterating distal segment of the common bile duct. There were also multiple right renal stones causing ureteral obstruction and hydronephrosis. Right nephrostomy was performed to release bile duct obstruction. However, sepsis and disseminated intravascular coagulation developed as a complication of acute pancreatitis, and the patient passed away. Although gallstone and alcoholism are the most common causes of acute pancreatitis, other causes should always be considered. Physicians should be aware of right hydronephrosis as one of the possible causes of acute pancreatitis in their workup of patients.
Keywords
Acute
hydronephrosis
pancreatitis
INTRODUCTION

Acute pancreatitis is an acute inflammatory disease of the pancreas that can involve peripancreatic tissues or remote organ systems, or both.[1] The diagnosis of acute pancreatitis is most often established by the presence of two of the following three criteria: Abdominal pain consistent with the disease, increased serum amylase and/or lipase greater than three times the upper limit of normal, and/or characteristic findings from abdominal imaging. Contrast-enhanced computed tomography (CECT) and/or magnetic resonance imaging (MRI) of the pancreas can be used to confirm the diagnosis.[23]
There are many causes of acute pancreatitis. The conditions most commonly associated with pancreatitis are obstruction of the common bile duct by stones (38%) and alcoholism (36%).[45] Other causes include tumor, infections, drugs (thiazide diuretics, furosemide, estrogen, methyldopa, sulfonamides), lipid abnormalities, postoperative pancreatitis (iatrogenic injury to pancreas), and trauma. About 20% of cases in adults remain idiopathic.[4]
The etiology and pathogenesis of acute pancreatitis have been intensively investigated, but the pathogenesis theories are still controversial. The predominant theory of pathogenesis relates to bile–pancreatic duct obstruction, which increases pancreatic duct pressure, bile reflux, trypsin activation, and pancreatic auto-digestion. Activation of digestive enzymes causes pancreatic injury and results in an inflammatory response. The acute inflammatory response itself causes substantial tissue damage and may progress beyond the pancreas to a systemic inflammatory response syndrome, multiple organ failure, and death.[45]
CASE REPORT
A 38-year-old man was admitted with a 2-month history of right-sided flank pain and intermittent epigastric pain, nausea, and vomiting. He had no history of alcohol use, took no medications, and had no family history of pancreatitis. On physical examination, epigastric tenderness and right-sided costovertebral angle tenderness without peritoneal signs were found.
Laboratory results showed that the renal function was not impaired (urea 27 mg/dl, normal 15–40 mg/dl; creatinine 1.24 mg/dl, normal 0.8–1.4 md/dl). The white cell count was 4200/μl and the liver function tests were normal. Urine output was adequate, and urinalysis was positive for leukocyte esterase, protein, and occult blood, consistent with urinary tract infection (UTI). An abdominal ultrasound showed hydronephrosis with right-sided multiple nephrolithiasis.
As the vomiting became severe, amylase and lipase were examined on the 3rd day of admission. The result showed elevated amylase (358 U/l, normal 53–123 U/l) and lipase (579 U/l, normal 0–160 U/l) levels. A magnetic resonance cholangiopancreaticography (MRCP) [Figure 1] revealed severe right-sided hydronephrosis due to multiple right renal stones which pushed the duodenum and head of pancreas anteriorly, obliterating distal segment of the common bile duct and causing dilation of proximal segment of the common bile duct and hepatic ducts. Neither stones nor space-occupying lesion was found in the biliary ducts.
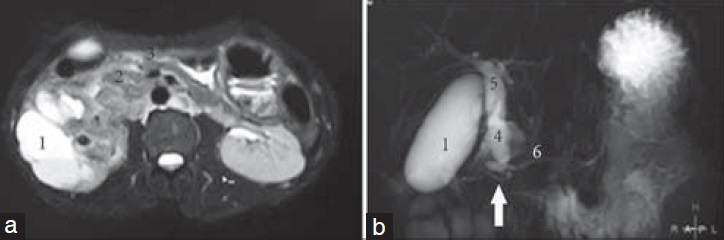
- 38-year-old man with right flank pain, nausea, and vomiting, diagnosed with acute pancreatitis due to right hydronephrosis. (a) Transverse section of the biliary tract and the right kidney on magnetic resonance cholangiopancreaticography (MRCP) showed grade 4 right hydronephrosis due to multiple renal stones (1) pushing the duodenum (2) and the head of pancreas (3) anteriorly. (b) Transverse section MRCP showed hydronephrosis obliterating the distal segment of the common bile duct (arrow) and dilatation of the proximal segment of common bile duct (4) and hepatic ducts (5). No dilatation of pancreatic duct (6) is seen.
When right-sided hydronephrosis was revealed as the cause of acute pancreatitis, the amylase and lipase had spiked to 1205 U/l and 804 U/l, respectively. Decompression of the obstructed urinary system via percutaneous nephrostomy was done only on the 10th day because of the unfavorable condition of the patient to undergo the procedures. The amylase and lipase levels decreased 14 days after nephrostomy to 592 U/l and 770 U/l, respectively. However, sepsis and disseminated intravascular coagulation developed as complications of acute pancreatitis, and the patient passed away.
DISCUSSION
Acute pancreatitis is an acute inflammatory disease of the pancreas that can involve peripancreatic tissues or remote organ systems, or both.[1] The diagnosis of acute pancreatitis is most often established by the presence of two of the following three criteria: Abdominal pain consistent with the disease, increased serum amylase and/or lipase greater than three times the upper limit of normal, and/or characteristic findings from abdominal imaging. CECT and/or MRI of the pancreas should be reserved for patients in whom the diagnosis is unclear or who fail to improve clinically within the first 48–72 h after hospital admission, or to evaluate complications.[23]
This patient was admitted for right-sided flank pain and intermittent epigastric pain, nausea, and vomiting. At first, it was presumed that he had renal colic and the gastrointestinal symptoms were caused by it. The ultrasound examination confirmed that the patient had right-sided hydronephrosis. But the symptoms were not consistent with other parameters, so there was suspicion of another disease entity. The abdominal pain consistent with the disease and increased amylase and lipase (greater than three times the upper limit of normal) confirmed the existence of acute pancreatitis. Subsequent investigations for the common causes of acute pancreatitis were not conclusive. The MRCP revealed that severe right-sided hydronephrosis was obliterating the distal segment of the common bile duct, dilating proximal segment of the common bile duct and hepatic ducts, and causing acute pancreatitis. Neither stones nor space-occupying lesion was found in the biliary ducts.
There are many causes of acute pancreatitis. The conditions most commonly associated with pancreatitis are obstruction of the common bile duct by stones (38%) and alcoholism (36%).[45] About 20% of cases in adults remain idiopathic.[4] Some reports mention the occurrence of pancreatic inflammation associated with renal hydronephrosis and pyelonephritis.[567] The etiology and pathogenesis of acute pancreatitis have been intensively investigated, but the pathogenesis theories are still controversial. The predominant theory of pathogenesis relates to bile–pancreatic duct obstruction, which increases pancreatic duct pressure, bile reflux, trypsin activation, and pancreatic auto-digestion. Activation of digestive enzymes causes pancreatic injury and results in an inflammatory response. The acute inflammatory response itself causes substantial tissue damage and may progress beyond the pancreas to a systemic inflammatory response syndrome, multiple organ failure, and death.[45] Based on another theory, the extravasation of infected urine from the obstructed right kidney into the surrounding tissues and subsequent irritation and inflammation of uncinate process, which lies anatomically close to the right ureter, gave rise to the acute pancreatitis. In this patient, both are possible mechanisms of acute pancreatitis.
The facts which confirmed that ureteric obstruction was the likely precipitating factor causing pancreatitis in this patient were: The pancreatic enzyme improved after decompression of the obstructed urinary system via percutaneous nephrostomy and the initial symptoms were right-sided flank pain before the onset of the epigastric pain, nausea, and vomiting. Moreover, other likely causes of acute pancreatitis were not found. The initial clinical picture was confusing, contributing to delayed diagnosis in this case, and showed non-specific and common presenting symptoms, i.e. right-sided flank pain, epigastric pain, nausea, and vomiting, which could occur in both pancreatitis and urinary tract obstruction. There have been a few reports in the literature of acute pancreatitis associated with an obstructed urinary system.[567] Some studies reported that it is not uncommon to find hydronephrosis on computed tomography (CT) scans of patients with pancreatitis.[8] All the studies of pancreatitis patients with obstructed urinary system showed right-side hydronephrosis as the cause of obstruction.[5678]
CONCLUSIONS
Although gallstone and alcoholism are the common causes of acute pancreatitis, other causes should always be considered. Physicians should be aware of right hydronephrosis as one of the possible causes of acute pancreatitis in their workup of patients.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/21/156123
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- American College of Gastroenterology. American college of gastroenterology guideline: Management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400-15.
- [Google Scholar]
- Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis-2012: Revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102-11.
- [Google Scholar]
- Acute pancreatitis: Etiology and common pathogenesis. World J Gastroenterol. 2009;15:1427-30.
- [Google Scholar]
- Ureteric obstruction as an unrecognized cause of acute pancreatitis in the emergency setting. JEPHC. 2009;7:1-6.
- [Google Scholar]
- Pyelonephritis complicating relapsing acute pancreatitis. Am J Nephrol. 1989;9:241-3.
- [Google Scholar]
- Right ureteral obstruction associated with pancreatitis. Urol Radiol. 1985;7:150-2.
- [Google Scholar]






