Translate this page into:
Imaging of the Bursae
Address for correspondence: Dr. Zameer Hirji, Department of Radiology, McMaster University Medical Centre, 1200 Main Street West, Hamilton, Ontario Canada, L8N 3Z5 E-mail: zameer.hirji@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
When assessing joints with various imaging modalities, it is important to focus on the extraarticular soft tissues that may clinically mimic joint pathology. One such extraarticular structure is the bursa. Bursitis can clinically be misdiagnosed as joint-, tendon- or muscle-related pain. Pathological processes are often a result of inflammation that is secondary to excessive local friction, infection, arthritides or direct trauma. It is therefore important to understand the anatomy and pathology of the common bursae in the appendicular skeleton. The purpose of this pictorial essay is to characterize the clinically relevant bursae in the appendicular skeleton using diagrams and corresponding multimodality images, focusing on normal anatomy and common pathological processes that affect them. The aim is to familiarize radiologists with the radiological features of bursitis.
Keywords
Bursae
computed tomography
imaging
interventions
magnetic resonance
ultrasound
INTRODUCTION

A bursa is a synovial-lined sac overlying the bony surfaces at areas of tendon friction. Bursae are located where tendons move against each other or glide over a bony surface. They are classified according to their location: subcutaneous, subfascial, subtendinous, and submucosal.[1] Bursae can also be classified as communicating or noncommunicating. When a bursa is located adjacent to a joint, the synovial membrane of the bursae may communicate with the joint.[2] This bursa is termed a communicating bursa. Some examples are the iliopsoas bursa lateral to the hip and the gastrocnemius-semimembranosus bursa posteromedial to the knee. In certain locations, communication between the joint and the bursa is abnormal. An example is the subacromial-subdeltoid (SASD) bursa that lies superior to the rotator cuff and inferior to the acromion. Most of the bursae are potential spaces and are not normally visualized on imaging.
In pathological conditions such as excessive local friction, infection, arthritides or direct trauma, fluid and debris collect within the bursa or fluid extends into the bursa from the adjacent joint. The walls of the bursa thicken as the bursal inflammation becomes longstanding. The term bursitis refers to pathological enlargement of the bursa. If the abnormally distended bursa is superficially located, it can be visualized by ultrasound as the ultrasound beam is able to penetrate through this region. The bursa is seen as a fluid-filled anechoic structure lined by a hyperechoic wall. Deep-seated bursae are depicted on magnetic resonance imaging (MRI) or computed tomography (CT). On MRI, the bursa is seen as a high T2 fluid-filled structure. CT shows the inflamed bursa as hypodense with an enhancing wall. Clinically, bursitis mimics several peripheral joint and muscle abnormalities. Therefore, it is important for the radiologist to identify bursal pathology and direct management geared toward bursitis.
SHOULDER
The normal shoulder joint has the following bursae surrounding the joint [Figure 1]:
-
Subacromial-subdeltoid bursa
-
Subscapular recess
-
Subcoracoid bursa
-
Coracoclavicular bursa
-
Supra-acromial bursa
-
Medial extension of SASD bursa
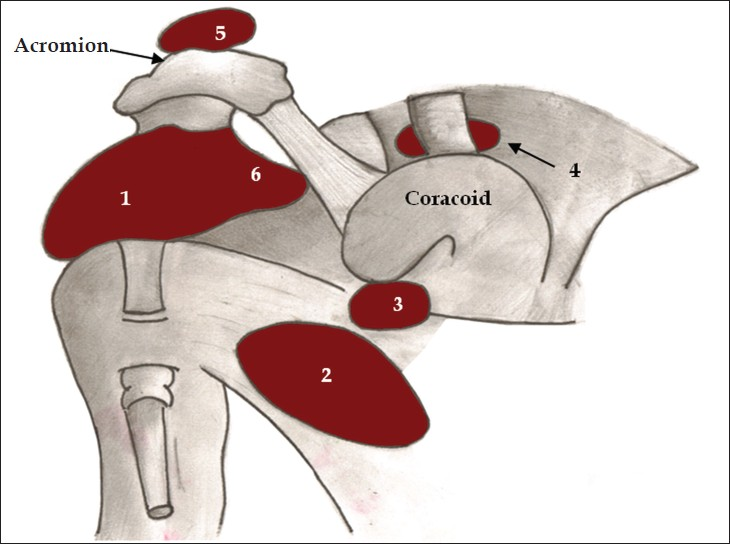
- Diagram of normal bursae surrounding the shoulder joint: (1) subacromial-subdeltoid bursa, (2) subscapular recess, (3) subcoracoid bursa, (4) coracoclavicular bursa, (5) supra-acromial bursa and (6) medial extension of subacromial-subdeltoid bursa.
Subacromial-subdeltoid bursa
The subacromial-subdeltoid (SASD) bursa comprise of two bursae that lie between the rotator cuff tendons and the undersurface of the acromion. They are located deep in the deltoid muscle and acromioclavicular joint (AC joint) and overlie the bicipital groove and rotator cuff.
The causes of SASD bursal fluid include: rotator cuff tears, impingement, septic bursitis, and reactive bursitis from glenohumeral joint disease, such as calcium deposition arthropathy.[3] In full-thickness tears of the rotator cuff, fluid from within the glenohumeral joint tracks through the tear into the bursa. Communication with the joint is abnormal in this location. This abnormal communication is best depicted on an MR arthrogram. Intraarticular gadolinium outlines the tear and extends into the bursa [Figure 2]. On MRI, the abnormal collection of fluid is seen as a low T1, high T2 signal within the bursa, either due to bursal inflammation or from a full-thickness rotator cuff tear. On ultrasound, the fluid-filled bursa overlies the rotator cuff and is clearly depicted as a fluid-filled anechoic structure both on longitudinal and transverse planes [Figure 3].
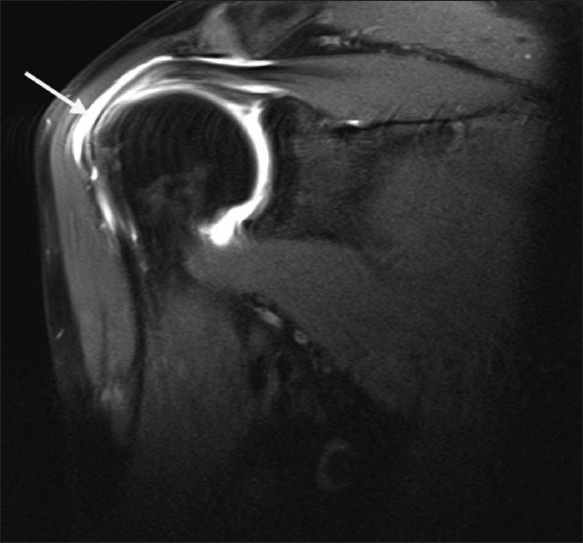
- Coronal magnetic resonance arthrogram depicting gadolinium in the SASD bursa from a full-thickness rotator cuff tear.
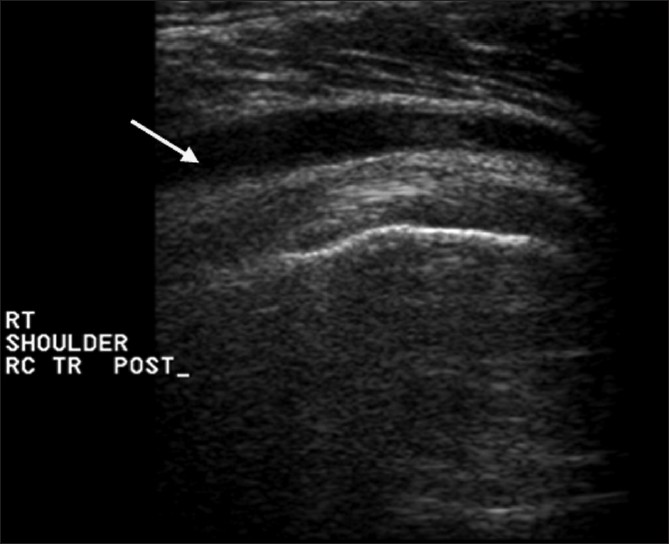
- Transverse ultrasound image of the rotator cuff depicting acute subacromial-subdeltoid bursitis.
Subcoracoid bursa
The coracoid and combined tendons of the short head of the biceps and coracobrachialis outline the superior aspect of the subcoracoid bursa. The subscapularis tendon lies inferior to this bursa [Figure 4].[4] It reduces friction and facilitates movement between the subscapularis tendon and the tendons of the short head of biceps and coracobrachialis during the arc of rotation of the humeral head.
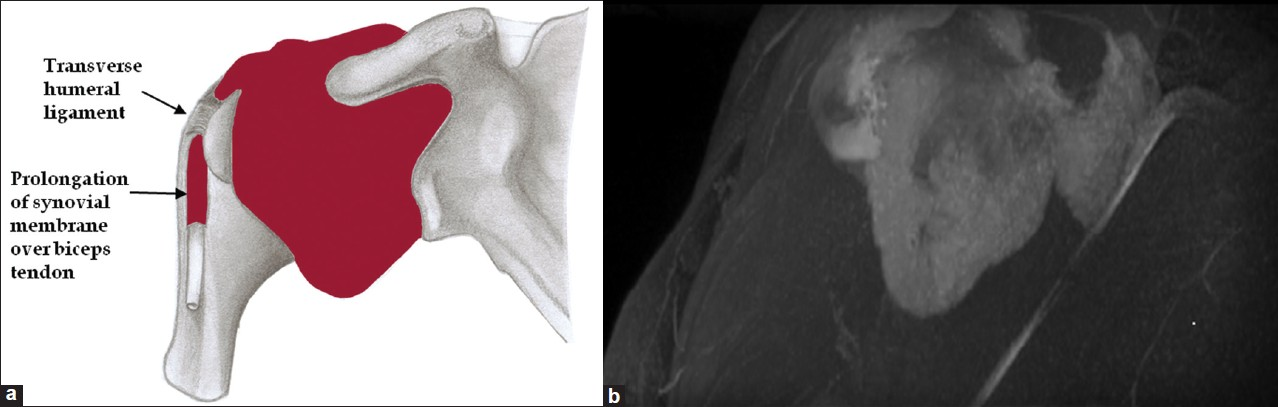
- (a) Line diagram and (b) corresponding magnetic resonance arthrogram of the subcoracoid bursa.
KNEE
Infrapatellar bursa
The superficial infrapatellar bursa is located in the subcutaneous fat between the distal third of the patellar tendon and the overlying skin [Figures 5 and 6].[5] Bursitis can be caused by chronic trauma due to occupational kneeling (Clergyman's knee) and direct trauma.[6] The bursa has been found in 55% of the cases in a cadaveric investigation.[7]

- Line diagram showing the superficial and deep infrapatellar bursae. (1) Superficial infrapatellar bursa, (2) deep infrapatellar, femur (F), Hoffa's fat pad (HF), patella (P), patellar tendon (PT) and tibia (T).

- Sagittal magnetic resonance T2 fat sat image depicting the superficial infrapatellar bursa.
The deep infrapatellar bursa is shaped as an inverted triangle, with the apex situated inferiorly between the patellar tendon anteriorly and the tibial margin posteriorly; its superior limit is the Hoffa's fat pad [Figures 5, 7 and 8].[5] Bursitis usually results from overuse of the extensor mechanism of the knee, especially with excessive running and jumping. Gout, septic bursitis, ankylosing spondylitis, and Osgood-Schlatter disease may also affect bursitis.[6]

- Sagittal magnetic resonance T2 gradient showing deep infrapatellar bursal fluid.
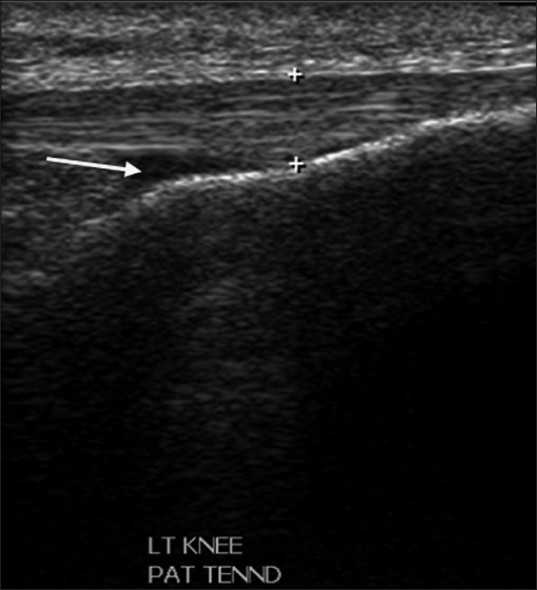
- Ultrasound in the longitudinal plane showing deep infrapatellar bursal fluid.
Prepatellar bursa
The prepatellar bursa is a tricompartmental structure [Figure 9].[8] The superficial compartment lies between the subcutaneous tissue and an extension of the fascia lata. The intermediate compartment is situated between the transverse superficial fascia and an intermediate oblique fascia formed by fascial extension of the vastus lateralis and vastus medialis muscles. The deep compartment lies between the intermediate oblique fascia and the deep longitudinal fibers of the rectus femoris tendon. Inflammation of this bursa occurs from repetitive trauma from kneeling, as seen with housemaids, carpet-layers, and wrestlers. It is also seen in inflammatory conditions such as gout [Figures 10 and 11].[9]

- Line diagram showing compartmentalization of the prepatellar bursa. SCCT - subcutaneous cellular tissues; QT - quadriceps tendon; PT - patellar tendon; F - femur; P, patella; (1) superficial compartment; (2) intermediate compartment; (3) deep compartment.

- Sagittal magnetic resonance T2 fat sat image showing high-signal fluid intensity within the prepatellar bursitis.

- Axial magnetic resonance T2 fat sat image depicting Baker's cyst with its neck between the semimembranosus and the medial gastrocnemius tendons. Image also depicts prepatellar bursitis.
Suprapatellar bursa
The suprapatellar bursa lies between the distal rectus femoris tendon and the femur. In the fifth fetal month, a septum (suprapatellar plica) that lies between the knee joint and the bursa perforates and results in a communication. This situation occurs in 85% of the adults.[10] The suprapatellar bursa is an example of bursae normally communicating with joints. On routine ultrasound and MR imaging, fluid in the suprapatellar bursa is a common finding in individuals with joint effusion [Figures 12 and 13]. In patients with a noncommunicating bursa and bursitis, fluid is localized only to the suprapatellar bursa.

- Longitudinal ultrasound image demonstrating fluid within the suprapatellar bursa.

- Sagittal magnetic resonance T2 gradient image demonstrating fluid within the suprapatellar bursa.
Semimembranosus-gastrocnemius bursa
The semimembranosus bursa is an inverted horseshoeshaped bursa medial to the semimembranosus tendon [Figures 14–16].

- Axial magnetic resonance T2 fat sat image showing semimembranosus bursa.

- Coronal magnetic resonance T2 Short TI Inversion Recovery (STIR) image showing semimembranosus bursa.

- Sagittal magnetic resonance gradient T2 image showing semimembranosus bursa.
Baker's cyst
The popliteal cyst or Baker's cyst lies along the posteromedial aspect of the knee and consists of intraarticular fluid extending through a slit into the bursa. The Baker's cyst has its neck between the semimembranosus muscle and medial head of the gastrocnemius tendons [Figure 11].[11] They are present in more than 50% of the population.[12] The cyst has been shown to be associated with internal derangement (81%), joint effusion (77%) and degenerative arthropathy (69%).[13] The cyst can be complex, with internal septae, debris and loose bodies. These cysts may rupture and the fluid flows into adjacent structures, simulating symptoms of thrombophlebitis.[14]
Pes anserine bursa
The pes anserine bursa lies between the conjoined tendons of the sartorius, semitendinosus, gracilis, and the tibial condyle [Figure 17a].[15] The bursa does not communicate with the knee joint.[16] Atypical meniscal cysts and synovial cysts also occur in this location. Although these cysts communicate with the knee joint, it is often difficult to make this distinction.[16] Anserine bursitis results from overuse, especially in runners, and is manifested by medial knee pain and swelling that may mimic medial meniscal tears or injury of the medial collateral ligament (MCL) [Figure 17b].[17]
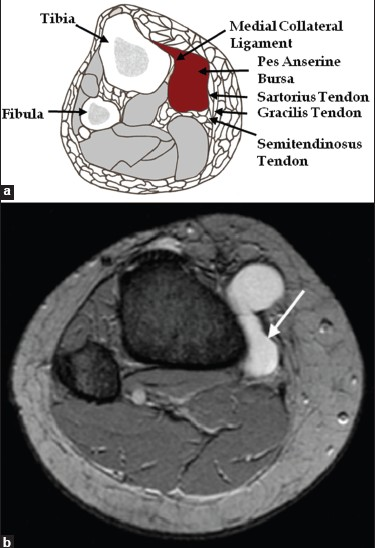
- (a) Axial line diagram and (b) axial magnetic resonance image showing pes anserine bursitis
Medial collateral ligament bursa
This bursa is found in approximately 93% of the patients.[18] It lies between the medial meniscus and the MCL at the level of the knee joint.[2] The medial supporting structures of the knee can be divided into three layers. Layer I consists of the crural fascia, Layer II is made up of the superficial portion of the MCL and Layer III is made up of the joint capsule and the deep portion of the MCL, which includes the meniscotibial and the meniscofemoral extensions. Along the posterior third of the medial side of the knee, the superficial and deep portions of the MCL are fused and tend to fold rather than glide when the knee is flexed [Figures 18 and 19].[19]

- Coronal magnetic resonance T2 fat sat image showing fluid within the medial collateral ligament bursa.

- Axial magnetic resonance T2 fat sat image showing fluid within the medial collateral ligament bursa.
ANKLE
Retrocalcaneal bursa
The retrocalcaneal bursa is a saddle-shaped bursa situated between the calcaneus and the Achilles tendon.[20] It assists in decreasing friction during plantar flexion.[21] Retrocalcaneal bursitis is common and is caused by Reiter disease, psoriasis, ankylosing spondylitis and, often, with calcaneal fractures [Figure 20].[10]
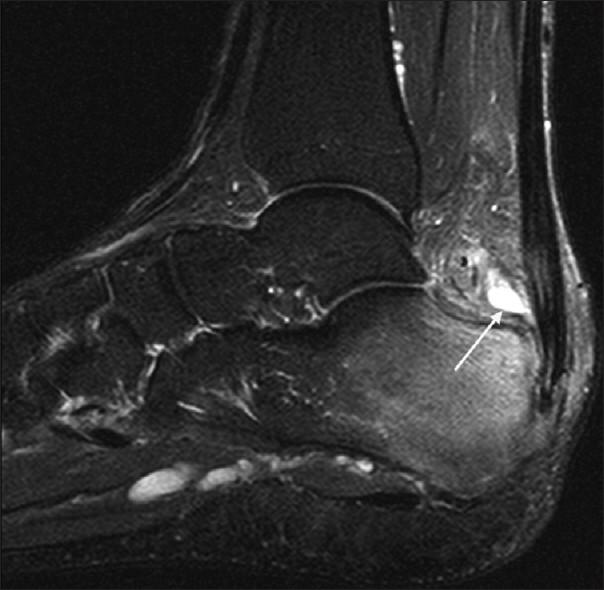
- Sagittal magnetic resonance T2 fat sat image showing retrocalcaneal bursitis with a thick synovial wall.
Superficial retrocalcaneal bursa
A second more superficial bursa lies between the Achilles tendon and the overlying subcutaneous fat [Figure 21].[4] Inflammation results from poorly fitting shoes. When superficial retrocalcaneal bursitis occurs in the setting of Achilles tendinopathy, a diagnosis of Haglund syndrome is made.
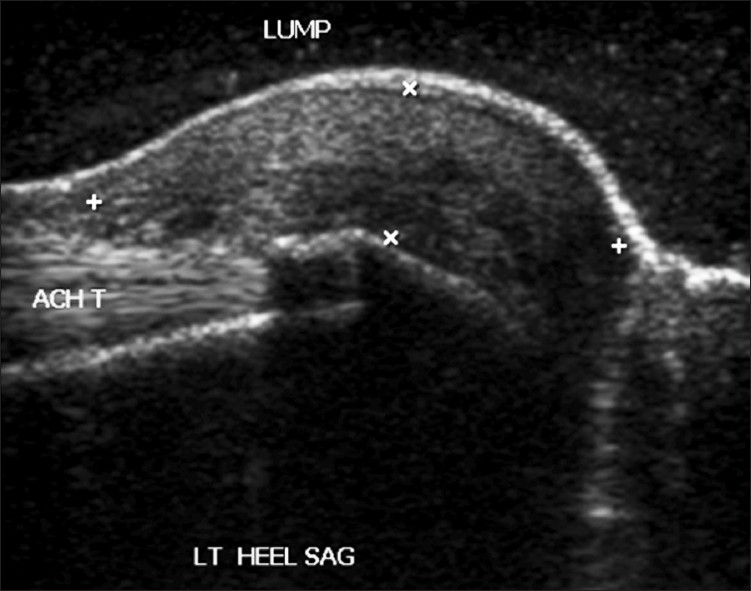
- Longitudinal ultrasound image showing superficial retrocalcaneal bursa.
HIP
Iliopsoas bursa
The iliopsoas bursa is the largest bursa around the hip joint (average size, 6 cm × 3 cm) and is situated beneath the musculotendinous portion of the iliopsoas muscle, anterior to the hip joint capsule and lateral to the femoral vessels [Figure 22].[22] It is found in about 98% of the subjects, and communicates with the cavity of the hip joint in about 15% of the cases.[23] Normally collapsed, distension of the bursa is usually caused by overproduction of synovial fluid in an arthritic hip leading to increased intraarticular pressure and extension of fluid into the potential space of the bursa.

- (a) Axial magnetic resonance T2 and (b) coronal magnetic resonance T2 STIR images of the left hip demonstrate a fluid-filled structure deep to the iliopsoas muscle in the expected location of the iliopsoas bursa. The iliopsoas tendon can be seen medial to the bursa and the femoral vessels can be seen further medially
Iliopsoas bursa distension in association with disease has been described in trauma, osteoarthritis, avascular necrosis, rheumatoid arthritis, synovial chondromatosis, pigmented villonodular synovitis, gout, and pyogenic infection.[2324] The differential diagnosis of an enlarged iliopsoas bursa includes inguinal or femoral hernia, neoplasm, lymphadenopathy, undescended testis, hematoma, psoas abscess, femoral aneurysm, and arteriovenous fistula.[24]
Trochanteric bursa
Pfirrmann and colleagues describe three major bursae about the greater trochanter.[25] The trochanteric bursa is the largest of the three. It covers the posterior facet, deep to the gluteus medius tendon and the proximal part of the vastus lateralis insertion. It is located beneath the gluteus maximus muscle and the iliotibial tract [Figure 23]. This bursa does not extend over the anterior border of the lateral facet. It is lined by a small layer of fat on both sides. Therefore, it can be routinely identified on nonenhanced coronal MR images as a fine linear structure paralleling the posterior facet [Figure 24]. Trochanteric (subgluteus maximus) bursitis is a common cause of hip pain, and is associated with obesity, trauma, inflammatory arthritides, and in patients with total hip arthroplasty.[2]

- Coronal line diagram of the trochanteric bursa overlying the posterior facet of the greater trochanter deep to the gluteus medius tendon.

- Coronal magnetic resonance T2 STIR image of the right trochanteric bursitis.
Subgluteus medius bursa
The subgluteus medius bursa is deep in the distal gluteus medius tendon. This bursa covers an area of the superior part of the lateral facet. Its superior extent is marked by the tip of the trochanter; its anterior extent, by the lateral facet; and its posterior and inferior extent, by the tendinous insertion of the gluteus medius muscle [Figure 25].

- Coronal magnetic resonance T2 STIR image of the bilateral subgluteus medius bursitis, larger on the right side.
Subgluteus minimus bursa
The subgluteus minimus bursa is in the area of the anterior facet. It lies beneath the gluteus minimus tendon, medial and superior to its insertion [Figure 26].

- Coronal magnetic resonance STIR image of the right subgluteus minimus bursitis.
ELBOW
The olecranon bursa is a subcutaneous bursa that provides almost frictionless motion between the skin, the subcutaneous tissues and the olecranon [Figure 27]. Because of its superficial location, it is a common site for injury, inflammation and infection. Repeated work-related trauma results in bursitis as seen in “student's elbow” or “miner's elbow.”[26]
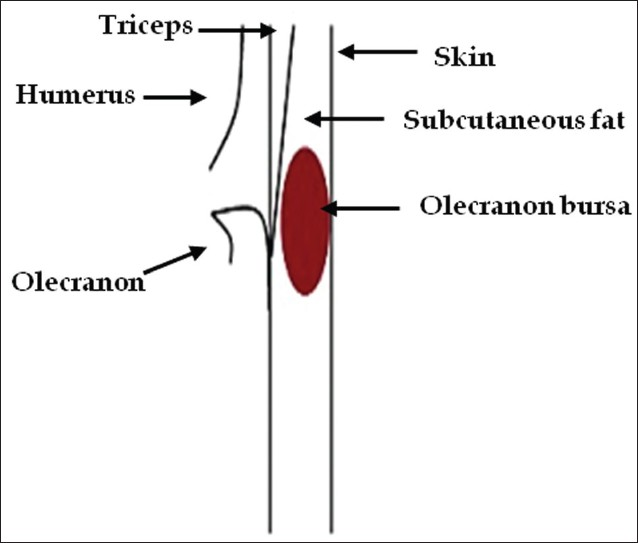
- Line diagram depicting location of the olecranon bursa.
Olecranon bursitis is identified by clinical diagnosis, and imaging is rarely performed in this context. In patients with advanced infection, MRI is sometimes requested to evaluate abscesses or osteomyelitis. Incidental diagnosis of olecranon bursitis on ultrasound and MRI is frequent from concomitant inflammation and effusion in the olecranon bursa secondary to trauma, rheumatoid arthritis and other inflammatory diseases [Figures 28 and 29].[27]

- Magnetic resonance T2 fat sat image with fluid in the olecranon bursa.
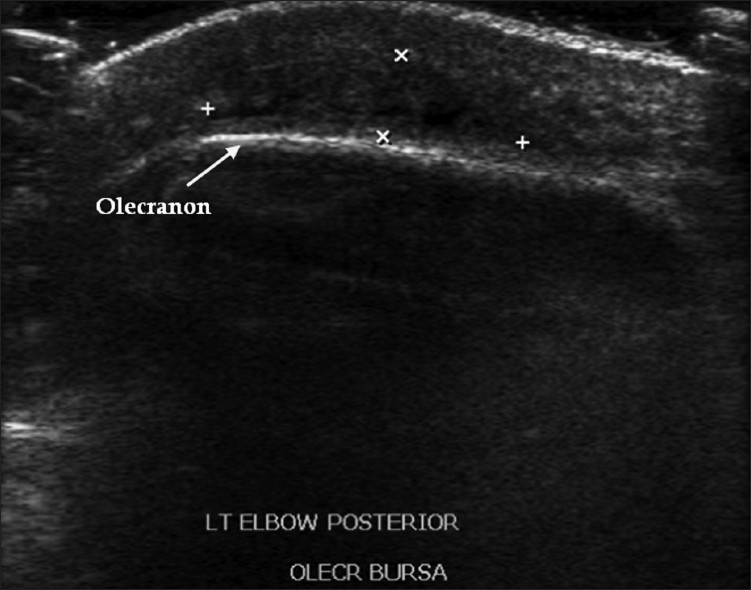
- Longitudinal ultrasound image demonstrating fluid and debris in the olecranon bursa.
Diagnostic and therapeutic interventions
Percutaneous aspiration/drainage/injection can be performed for diagnostic and therapeutic purposes under image guidance utilizing ultrasound, fluoroscopy or CT based on accessibility to the bursa [Figures 30 and 31].

- (a) Enhanced axial computed tomography of the right iliopsoas bursitis and (b) ultrasound-guided drainage.

- (a) Ultrasound- and (b) fluoroscopy-guided trochanteric bursal injection.
CONCLUSION
Familiarity with the normal anatomy, pathology, and imaging characteristics of bursae is important as bursitis can mimic pain related to joints, periarticular tendons, and muscles. Distinguishing bursitis from other causes of joint, periarticular tendon and muscle pain will direct the clinician toward focused management of bursitis, including image-guided therapeutic injections utilizing steroid and long-acting local anesthetics.
ACKNOWLEDGMENTS
The authors would like to thank Akhila Rachakonda of Hillfield Strathallan College for the line diagrams.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/22/80374
REFERENCES
- Diagnosis of Bone and Joint Disorders. (3rd ed). Philadelphia (PA): W.B. Saunders; 1995. p. :667-8.
- [Google Scholar]
- Common bursae around the body: A review of normal anatomy and magnetic resonance imaging findings. Radiologist. 2002;9:209-11.
- [Google Scholar]
- An anatomical study of the role of long thoracic nerve and the related scapular bursae in the pathogenesis of local paralysis of the serratus anterior muscle. Anat Rec. 1938;71:375-86.
- [Google Scholar]
- The MRI appearance of cystic lesions around the knee. Skeletal Radiol. 2004;33:187-209.
- [Google Scholar]
- Deep and superficial infrapatellar bursae: Cadaveric investigation of regional anatomy using magnetic resonance after ultrasound-guided bursography. Skeletal Radiol. 2007;36:41-6.
- [Google Scholar]
- The prepatellar bursa: Cadaveric investigation of regional anatomy with MRI after sonographically guided bursography. AJR. 2007;188:355-8.
- [Google Scholar]
- Gastrocnemio-semimembranosus bursa and its relation to the knee joint. Anatomy and Histology. Acta Radiol. 1977;18:497-512.
- [Google Scholar]
- A clinical and anatomic study of the semimembranosus bursa in relation to popliteal cyst. J Bone Joint Surg Am. 1938;20:963-84.
- [Google Scholar]
- MR imaging of Baker cysts: Association with internal derangement, effusion and degenerative arthropathy. Radiology. 1996;201:247-50.
- [Google Scholar]
- Neoplastic and tumorlike lesions detected on MR Imaging of the knee in patients with suspected internal derangement. Entities Am J Roentgenol. 2002;178:595-9.
- [Google Scholar]
- Runner's injuries: Part two. Evaluation and treatment of specific injuries. Am J Sports Med. 1980;8:287-9.
- [Google Scholar]
- The supporting structures and layers on the medial side of the knee: An anatomical analysis. J Bone Joint Surg Am. 1979;61:56-62.
- [Google Scholar]
- The os calcis, the tendo-Achilles and the local bursae. Bull Hosp Jt Dis. 1966;27:76-89.
- [Google Scholar]
- Sonography of the iliopsoas tendon and injection of the iliopsoas Bursa for diagnosis and management of the painful snapping hip. Skeletal Radiol. 2006;35:565-71.
- [Google Scholar]
- Symptomatic snapping hip: Targeted treatment for maximum pain relief. Phys Sports Med. 2004;32:25-31.
- [Google Scholar]
- Greater Trochanter of the hip: Attachment of the abductor mechanism and a complex of three bursae-MR imaging and MR bursography in cadavers and MR imaging in asymptomatic volunteers. Radiology. 2001;221:469.
- [Google Scholar]
- Septic olecranon bursitis : Recognition and treatment. J Am Board Fam Pract. 1995;8:217-20.
- [Google Scholar]






