Translate this page into:
Acute Renal Artery Occlusion with Prolonged Renal Ischemia: A Case of Successful Treatment with Stent Placement and Catheter-directed Thrombolysis
Address for correspondence: Dr. Mohammad Arabi, Department of Radiology, University of Michigan, 1500 East Medical Center Drive, CVC 5582 / SPC 5868, Ann Arbor, MI 48109-5868, USA. E-mail: marabi@med.umich.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We present a case of acute renal artery occlusion caused by a high-grade stenosis associated with in-situ thrombosis. Endovascular renal artery stent placement combined with catheter-directed thrombolysis reversed the renal ischemia with restoration of renal function despite the prolonged ischemia.
Keywords
Renal ischemia
revascularization
thrombolytic therapy
INTRODUCTION

Acute renal artery occlusion is a rare clinical condition that occurs as a result of renal artery embolism or less commonly in-situ renal artery thrombosis from various etiologies.[1] Unless the underlying lesions are treated expeditiously, renal ischemia will invariably lead to infarction.[2–4] In addition to the antihypertensive management and systemic anticoagulation, endovascular therapy has been reported in treating patients with acute renal ischemia.[34]
The outcome of treatment in acute renal ischemia depends on the etiology and interval between the onset of symptoms and initiation of therapy.[2–4]
This case illustrates the potential benefits of renal artery revascularization in the setting of acute renal artery occlusion despite prolonged ischemia.
CASE REPORT
A 47-year-old female had undergone liver transplantation for cryptogenic cirrhosis and hepatorenal syndrome two years prior to the present hospitalization. Her post-operative course was complicated by acute tubular necrosis (ATN) that required temporary hemodialysis. Her baseline glomerular filtration rate (GFR) was 47 ml/min prior to her presentation.
She presented to the Emergency Department complaining of pain on the left side of the abdomen. A contrast-enhanced abdominal computed tomography (CT) scan demonstrated multiple wedge-shaped low-attenuation areas, involving large proportion of the left kidney, associated with a filling defect in the left main renal artery [Figure 1].
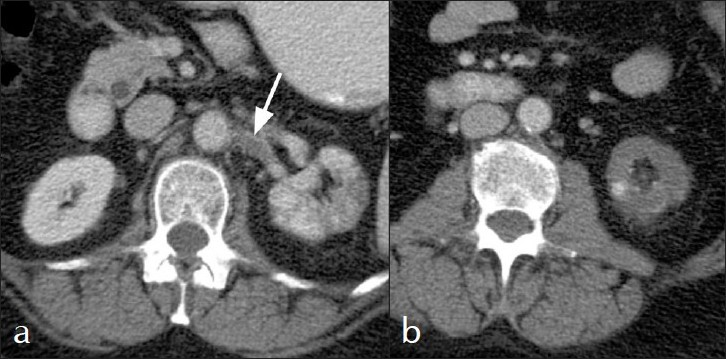
- Contrast-enhanced CT scan of the abdomen demonstrates (a) left renal artery thrombus (arrow) and (b) heterogenous cortical enhancement and wedge shaped cortical hypodensities in the lower pole of the left kidney.
Her vital signs and physical examination were unremarkable except for mild tenderness in the left upper quadrant. Laboratory studies revealed a creatinine level of 1.4 mg/dl and Glomerular Filtration Rate (GFR) of 43 ml/min (normal >59 ml/min). Urinalysis was positive for leukocyte esterase.
Twenty-two hours after the onset of symptoms the patient underwent a CO2 digital subtraction aortogram that revealed a proximal left renal artery stenosis with post-stenotic dilatation. Selective renal angiography demonstrated a thrombus immediately distal to the stenosis [Figure 2]. The renal perfusion was significantly reduced secondary to the combination of the stenosis and in-situ thrombus. In order to improve the blood flow in the renal artery, the stenosis was stented with a 6 mm × 15 mm balloon expandable Palmaz stent (Cordis, Warren, NJ). Renal angiogram after stent placement showed a widely patent main renal artery and distal embolization of the thrombus into the inferior segmental branch [Figure 3a]. Therefore, a 4-Fr Glide Cobra catheter with side holes (Terumo, Leuven, Belgium) was placed in the renal artery distal to the stent and intra-arterial thrombolysis was initiated using 0.25 units per hour of reteplase (Retavase® ; PDL BioPharma, Inc. Fremont, CA, USA).
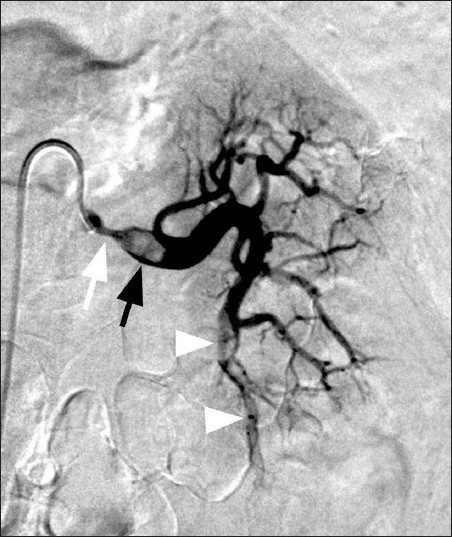
- Selective left renal angiogram shows a proximal high-grade stenosis (white arrow) with a thrombus in the post stenotic segment of the renal artery (black arrow) and several emboli in the inferior segmental renal branches (arrowheads).
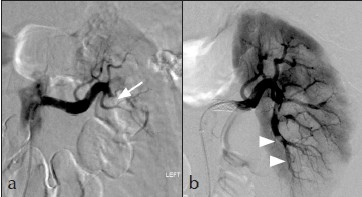
- (a): After stent placement the renal artery is widely patent with improved blood flow in the renal artery. Stent placement had resulted in distal embolization of thrombus into the inferior renal branch (arrow). (b) Renal angiogram following 22 hours of thrombolysis showed small residual emboli in the inferior branches (arrowheads) with significant improvement of the cortical perfusion.
After 22 hours of thrombolysis, a repeat angiogram revealed near complete resolution of the segmental renal artery thrombus [Figure 3b]. No immediate post thrombolysis complications were encountered.
After completion of thrombolysis the patient was placed on heparin infusion for one day. The patient was then discharged on aspirin 81 mg daily. One month later, 99mTc MAG3 renal scintigraphy showed slightly reduced renal uptake in the lower pole of the left kidney and a borderline decreased split renal function at 38% [Figure 4]. Her laboratory findings returned to baseline values seen prior to presentation.
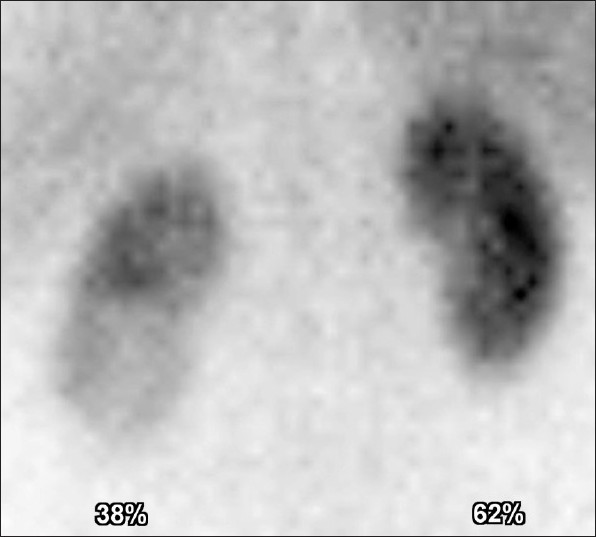
- Renal isotope scan one month later revealed slightly reduced cortical uptake in the lower pole of the left kidney with borderline reduced split renal function of 38%.
DISCUSSION
Acute renal artery occlusion is a rare clinical condition that commonly manifests as persistent abdominal/flank/lower back pain.[1]
The two major causes of renal infarction are thromboemboli, that usually originate from a thrombus in the heart or aorta, and the less common in-situ thrombosis of a renal artery.[1] Other less common causes include trauma, congenital vascular disorders, fibromuscular dysplasia,[5] hypercoagulable states, aortic dissections, and iatrogenic etiologies mainly caused by endovascular interventions.[1]
Diagnosis of acute renal infarction is often delayed or missed due to both the rarity of the disease and its non-specific clinical presentation. In addition to the acute onset of abdominal pain, patients may present with acute hypertension. Laboratory findings include elevated white cells count, serum creatinine, LDH , and hematuria.[6]
Due to the non-specific nature of the clinical presentation, imaging is often performed to rule out other etiologies, most commonly renal stones.[6] CT has a much higher sensitivity for renal infarct when compared to ultrasound.[6]
Renal angiography remains the gold standard to establish the diagnosis and determine the etiologies leading to renal infarction.
Many factors may play a role in the restoration of the renal function after revascularization procedures including the interval between the onset of symptoms and initiation of therapy, etiology of the acute renal artery occlusion, and the presence of the intra renal arterial occlusion.[2–4]
Successful revascularization of the main renal artery does not predict the outcome of the involved kidney.[34] Salam et al., reported restoration of the renal function, after successful revascularization in only 3 out of 7 patients.[3]
On the other hand, Ouriel et al., found that restoration of the renal function after successful revascularization is dependent on the etiology.[2] They reviewed 35 patients with acute renal artery occlusion. They found that revascularization of embolic arterial occlusion was successful in the relief of hypertension but was ineffective in the restoration of renal function; while in patients with thrombotic occlusion, thrombectomy, and aortorenal bypass it was successful in both the reduction of blood pressure and the restoration of renal function. Traumatic renal occlusion did not benefit from revascularization despite early intervention.[2]
Few reports indicate the restoration of the renal function after successful revascularization in patients with acute renal failure and anuria.[7]
The maximum duration between the onset of symptoms and intervention is variable, according to reports, ranging between 3 hours to 5 weeks.[348]
The exact role of endovascular therapy remains controversial and uncertain in the literature. However, the main goal of endovascular therapy remains to re-establish blood flow to the ischemic kidney that may preserve the remaining renal function. The endovascular options include intra-arterial fibrinolytic therapy, pharmacomechanical thrombectomy, and aspiration thrombectomy with or without angioplasty. These treatment options should be reserved for those who do not have prolonged ischemia time, cortical atrophy, and contraindication for thrombolysis.
Blum et al., reviewed fourteen patients with acute embolic renal artery occlusion treated with local low-dose thrombolysis that achieved successful revascularization in 13 of 14 patients.[4] They concluded that thrombolytic therapy in acute embolic renal artery occlusion does not restore renal function and is therefore not indicated once the ischemic tolerance of the kidney (approximately 90 minutes) has been exceeded.[4]
On the other hand, Piffaretti et al., reported 4 cases of acute renal infarction treated with intra-arterial fibrinolytic therapy (n = 4) and 2 cases of stent angioplasty (n = 2). Normal renal function was restored in all patients at a mean follow-up of 22 months.[8]
The endovascular treatment techniques for renal artery are not standard and several fibrinolytic agents have been utilized for variable lytic therapies. Angioplasty has been performed based on the etiology and the response to thrombolytic therapy.[348] Percutaneous embolectomy[9] and rheolytic therapy[10] are additional options.
In our case, although the estimated ischemic proportion of the kidney was greater than 50% based on the initial diagnostic CT scan, we elected to proceed to attempt renal artery revascularization despite the 22 hours window, considering the pre-existing baseline renal dysfunction any further renal parenchymal damage may have compromised the renal function and necessitated hemodialysis. Nevertheless, we made the decision of stenting the renal artery prior to initiation of thrombolysis, as opposed to thrombolysis followed by stenting, to instantaneously restore the blood flow to the kidney and improve the efficacy of the fibrinolytics. Interventionalists should keep in mind the potential acute reperfusion injury that could happen following immediate revascularization and the possibility of distal embolization into the segmental branches that may reduce the perfusion to the renal parenchyma. The success of the endovascular treatment in the presented case prevented further deterioration of the renal function. The pre-existing high-grade stenosis with long standing renal ischemia and collateral formation may have contributed to the renal function preservation in this case.
In conclusion, this case illustrates that the lack of concrete evidence of the benefit of renal artery revascularization in the setting of acute renal ischemia should not preclude attempts at renal revascularization whenever clinically possible. The risks to the patient should be weighed against the benefits of the procedure when making the management decision. Endovascular options with intra-arterial thrombolysis offer a relatively safe method that may help in salvaging the remaining renal parenchyma and restoration of renal function.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp? 2011/1/11/76689
REFERENCES
- Acute renal infarction.Clinical characteristics of 17 patients. Medicine (Baltimore). 1999;78:386-94.
- [Google Scholar]
- Acute renal artery occlusion: when is revascularization justified? J Vasc Surg. 1987;5:348-55.
- [Google Scholar]
- Local infusion of fibrinolytic agents for acute renal artery thromboembolism: report of ten cases. Ann Vasc Surg. 1993;7:21-6.
- [Google Scholar]
- Effect of local low-dose thrombolysis on clinical outcome in acute embolic renal artery occlusion. Radiology. 1993;189:549-54.
- [Google Scholar]
- Renal arterial fibromuscular dysplasia: acute renal infarction in three patients with angiographic evidence of medial fibroplasia. Br J Radiol. 1992;65:81-4.
- [Google Scholar]
- Acute renal embolism.Forty-four cases of renal infarction in patients with atrial fibrillation. Medicine (Baltimore). 2004;83:292-9.
- [Google Scholar]
- Percutaneous revascularization of occluded renal arteries in the setting of acute renal failure. Vasc Med. 2009;14:365-9.
- [Google Scholar]
- Catheter-directed thrombolysis for acute renal artery thrombosis: report of 4 cases. Vasc Endovascular Surg. 2008;42:375-9.
- [Google Scholar]
- Successful endovascular treatment of bilateral renal artery paradoxical embolus by a modified standard technique. Nephrol Dial Transplant. 2006;21:2315-7.
- [Google Scholar]
- Acute renal artery thrombosis treated by percutaneous rheolytic thrombectomy. Catheter Cardiovasc Interv. 2002;56:66-8.
- [Google Scholar]






