Translate this page into:
Endobronchial Ultrasound: A Useful Tool in the Diagnosis of Bronchogenic Cyst
Address for correspondence: Dr. Stamatis Katsenos, Department of Pneumonology, Army General Hospital of Athens, 158 Mesogion and Katehaki Avenue, 115 25 Athens, Greece. E-mail: skatsenos@yahoo.gr
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Diagnosis of bronchogenic cysts is possible with computed tomography, where the cysts are seen usually as well-circumscribed lesions of water density. However, many of the cysts have a soft-tissue density thus rendering them indistinguishable from neoplasms. In this article, we describe a case of bronchogenic cyst presenting as soft-tissue mass that was evaluated and diagnosed by endobronchial ultrasound (EBUS). We discuss the ultrasound image characteristics of the cyst and its histopathology findings. EBUS seems to be a valuable tool in the diagnosis of bronchogenic cysts and also enables their complete aspiration.
Keywords
Bronchoscopy
bronchogenic cyst
endobronchial ultrasound
INTRODUCTION

Bronchogenic cysts are congenital lesions thought to result from abnormal budding of the ventral foregut that occurs between the 26th and 40th days of gestation.[1] This abnormal bud subsequently differentiates into a fluid-filled, blind-ending pouch. The clinical features are variable. They may be asymptomatic, especially in older children and adults. Otherwise, chest pain, cough, dyspnea, fever, and expectoration if the cysts are infected comprise their symptomatology.[2]
Diagnosis of bronchogenic cysts is possible with computed tomography (CT) that usually shows well-circumscribed lesions of water density. However, half of the cysts have attenuation values of soft-tissue because of viscid mucoid content, making them indistinguishable from neoplasms. In this article, we describe the imaging characteristics and pathological findings in a case of bronchogenic cyst presenting as soft-tissue mass, which was evaluated and diagnosed by endobronchial ultrasound (EBUS). An 18-year-old male presented with 2-months history of progressive dyspnea on exertion and persistent non-productive cough. Physical examination was unremarkable.
RADIOLOGICAL FEATURES
Chest X-ray showed a left perihilar mass and the CT scan revealed a well-circumscribed, round homogeneous low-density (50 Hounsfield Units) mass in the middle mediastinum adjacent to the left main bronchus measuring 5.1 cm × 5.8 cm at its maximum, causing over 80% luminal narrowing of both left pulmonary veins [Figure 1]. Rigid bronchoscopy was performed under general anesthesia followed by the insertion of the fiber-optic bronchoscope, which demonstrated a moderate extrinsic compression of the left main stem bronchus. Radial probe of 20 MHz frequency EBUS with a balloon (Olympus, UM-BS20-26R) was then placed through the working channel of the fiber-optic bronchoscope and this showed a hypoechoic homogeneous lesion compressing the left main stem bronchus suspicious of a cystic mass. Fine internal echoes within the lesion suggested it was mainly a viscous fluid-filled cyst. All bronchial wall layers were intact [Figure 2].
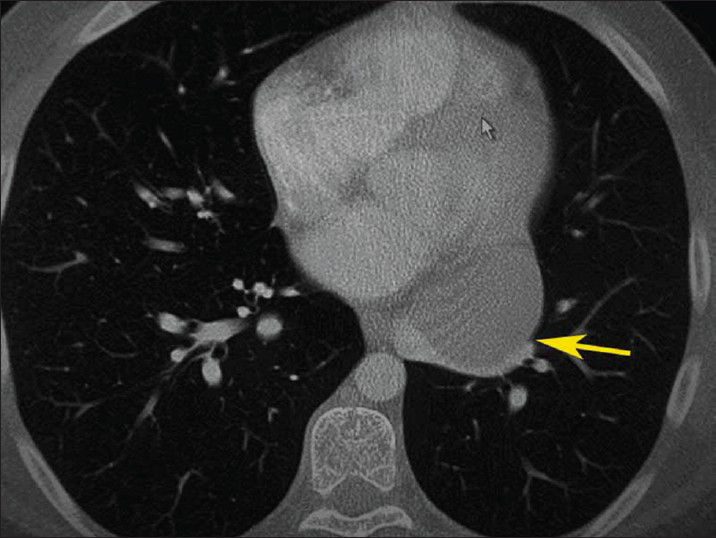
- 18-year-old male with progressive dyspnea on exertion and dry cough diagnosed with bronchogenic cyst. Contrast-enhanced computed tomography of the chest (lung window) shows a well-defined round homogeneous low-density mass in the mediastinum adjacent to the left main bronchus measuring 5.1 cm × 5.8 cm at its maximum, causing over 80% luminal narrowing of both left pulmonary veins (yellow arrow).
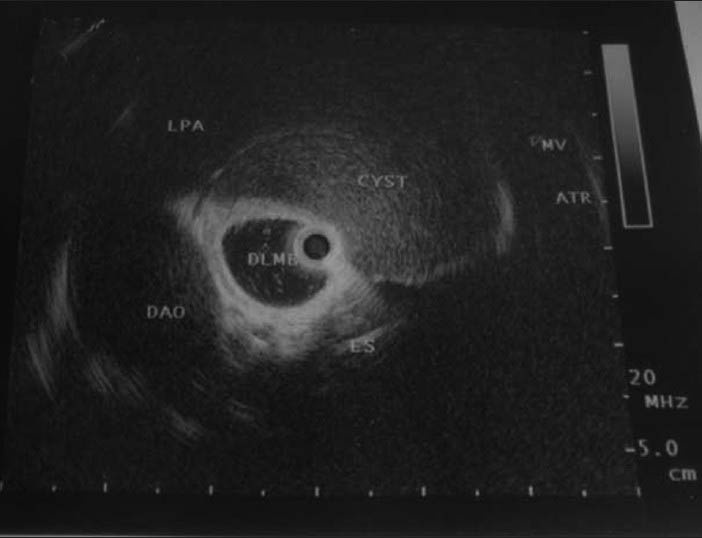
- 18-year-old male with progressive dyspnea on exertion and dry cough diagnosed with bronchogenic cyst. Endobronchial ultrasound demonstrates a hypoechoic homogeneous lesion compressing the left main stem bronchus suspicious of a cystic mass with surrounding anatomical structures. DLMB: Distal left main bronchus, DAO: Descending aorta, LPA: left pulmonary artery, ATR: Atrium, MV: Mitral valve.
PATHOLOGICAL FEATURES
Patient underwent complete surgical excision of the mediastinal cyst through a left posterolateral thoracotomy and exhibited an uneventful recovery. Grossly, the cyst was smooth, thin-walled, and unilocular measuring a maximum of 4.5 cm × 3.5 cm × 2.5 cm and containing mostly mucous brownish fluid [Figure 3]. Aspiration of the cyst contents was initially performed to make the cyst technically easier to remove. Then, the cyst was carefully dissected free of its mediastinal and pleural attachments, taking care not to leave any residual cyst wall behind. Histopathologically, the cyst was lined by respiratory epithelium with areas of sub-epithelial fibrosis [Figure 4]. A slight chronic inflammation of the epithelial lining was also noted. Microbiologic and cytologic examinations of cyst fluid were negative for any pathogen development or malignancy, respectively. The afore-mentioned findings were consistent with the presence of a bronchogenic cyst. At last follow-up, 2 months post-operatively, the patient had completely recuperated without complaints of any symptoms.
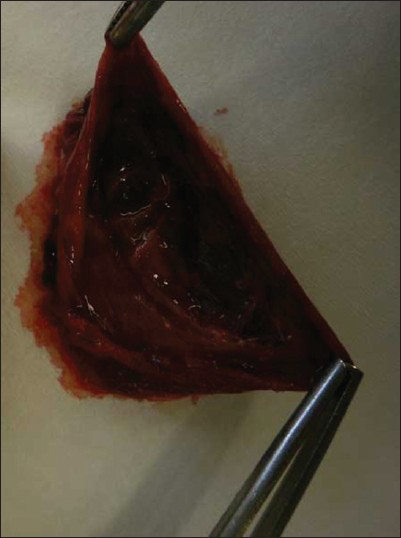
- 18-year-old male with progressive dyspnea on exertion and dry cough diagnosed with bronchogenic cyst. Photography the surgically removed mass shows the resected thin-walled and unilocular cyst measuring a maximum of 4.5 cm × 3.5 cm × 2.5 cm and containing mostly mucous brownish fluid.
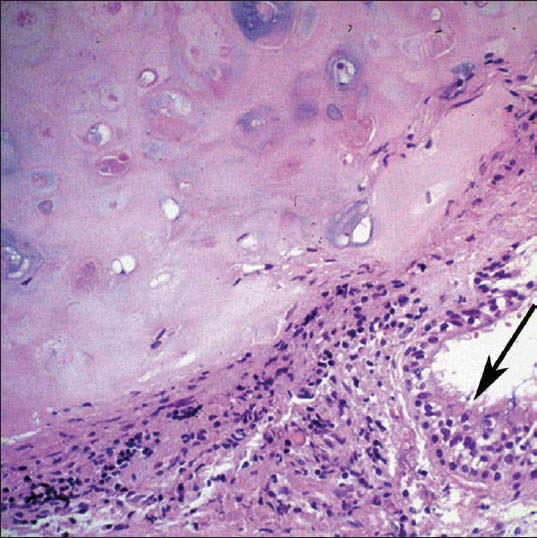
- 18-year-old male with progressive dyspnea on exertion and dry cough diagnosed with bronchogenic cyst. Microscopic examination of the mass (Hematoxylin and Eosin, ×50) shows a portion of the cyst wall with respiratory epithelium (black arrow) that overlies fibrous tissue and cartilage.
DISCUSSION
Bronchogenic cysts are congenital bronchopulmonary lesions derived from an abnormal budding of the tracheobronchial tree during embryonic development. Their incidence is estimated between 1:42,000 and 1:68,000. However, it is difficult to appreciate the incidence of the cysts exactly since some aged patients have lesions that remain forever silent. Bronchogenic cysts are the predominant sub-group of mediastinal cysts accounting for approximately 40% according to one series followed by pericardial cysts (35%), enteric cysts (10%), and non-specific cysts (14%).[1]
They are typically located near the large airways just posterior to the carina and lined with cartilage and pseudostratified columnar epithelium. Less commonly, they arise within the lung parenchyma.[2] Most bronchogenic cysts are seen in childhood, but can be diagnosed in adults. Presentation beyond 50 years of age is distinctly unusual. Bronchogenic cysts predominantly occur in males. Though usually found as an incidental finding on a chest radiograph performed for other unrelated conditions, they may cause compression symptoms such as chronic cough, chest pain, and dyspnea or may become infected. The symptoms occur frequently in children since their smaller thoracic volume and malleable airways predispose them to compressive symptoms earlier when the cyst enlarges.[3]
As for imaging modalities, mediastinal bronchogenic cyst appears on plain chest radiograph as smooth rounded opacity in the mediastinum. Some cysts that lie beneath the carina cannot be visualized by chest X-ray. Moreover, CT scan and magnetic resonance imaging (MRI) may both provide accurate diagnosis of bronchogenic cysts using typical characteristics of a round, well-circumscribed, unilocular mass with density of water. More specifically, uniform low T1 and high T2 intensities, indicative of water density, are demonstrated on MRI. Roughly, half of the cysts have attenuation values of soft-tissue because of viscous mucoid contents making them indistinguishable from neoplasms.[4] Although magnetic resonance may help to further differentiate these lesions, they can still be confounded with malignancies presenting with central necrosis.
Nevertheless, EBUS is a new promising modality, which has broadened the diagnostic possibilities for airway and mediastinal pathology. Both ultrasound probes (radial with a balloon-20 MHz and the convex one-7.5 MHz) allow better visualization of the tracheobronchial wall and mediastinal structures.[5] In the present case, EBUS detected easily the cystic lesion determining further its extent and relation to the airway wall and key anatomic structures and characterizing the intrinsic composition of its content. More specifically, ultrasound image showed a hypoechoic lesion with fine internal echoes within it thus suggesting mainly a viscous fluid-filled cyst.
Echogenicity of cystic lesions is related to their cellular content and echogenicity is by convention described with reference to soft-tissue such as lymph nodes or tumors. These structures are gray in color and are termed isoechoic. Darker (hypoechoic) or black (anechoic) images denote either cysts with serous fluid or blood vessels. Echogenic images within cysts identify complicated fluid collections that may contain either frank pus or blood clots. The presence of septations, thickened walls or floating debris within the cyst may give further radiological clues to an infected cyst. Therefore, EBUS can be used to diagnose bronchogenic cysts that present as soft-tissue densities on CT imaging. If there is any doubt in the diagnosis, then EBUS transbronchial aspiration can be considered and aspirate sent for bacterial cultures and cytological analysis.
Despite extensive investigations, the nature of a cystic lesion in the thorax cannot be ascertained in a significant percentage of individuals preoperatively. Differential diagnosis of bronchogenic cyst includes many other entities such as, congenital cysts and malformations (pericardial cysts, cystic hygroma/lymphangioma, neurenteric cyst, esophageal duplication cyst, thyroid colloid cyst, thymic cyst), hydatid cysts, lymphoma, lung abscess, fungal disease, tuberculosis, infected bullas, vascular malformations, mediastinal tumors, hematoma, sarcoidosis, pancreatic pseudocyst (for retroperitoneal bronchogenic cysts or for pancreatic pseudocysts that extend intrathoracically through the aortic hiatus or esophageal hiatus) and pulmonary masses (congenital cystic adenomatoid malformation, pulmonary sequestration, lung cancer, metastases).
Surgical resection remains the mainstay and the only curative treatment for bronchogenic cysts, even though they are asymptomatic and vary in their clinical behavior. The crucial point for avoiding cyst recurrences is the complete excision of the mucosal lining. Prognosis is generally good after complete resection.[2] In addition, convex-probe EBUS has an important implication in the management of the bronchogenic cyst as shown by recently published case studies, where it was successfully used to puncture and aspirate the cyst contents in patients who were unfit for surgery.[6789] Furthermore, real-time ultrasound allows complete aspiration of the cyst that is not always possible when “blind” techniques are employed. This results in cyst collapse and adhesion of the mucosal lining thus diminishing recurrence rates. Trans-thoracic aspiration can be done under ultrasound or CT guidance.[10] This is more likely a temporary procedure when emergency decompression of the cyst is needed to relieve a significant airway narrowing or in patients not fit for thoracotomy or other invasive procedure. Sometimes sclerosants like alcohol and bleomycin can be injected to prevent cyst recurrence. The disadvantage of the option is the possible increase in the cyst size later and the minimal risk of malignant transformation.
CONCLUSION
EBUS has a potential role in diagnosis, when a confident diagnosis of bronchogenic cyst cannot be made by CT. In particular, it can easily identify the cystic lesion and clearly clarify its nature as well as provide imaging guidance for therapeutic procedures.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/57/124078
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Pulmonary and mediastinal bronchogenic cysts: A clinicopathologic study of 33 cases. Lung. 2008;186:55-61.
- [Google Scholar]
- Bronchogenic cyst: Imaging features with clinical and histopathologic correlation. Radiology. 2000;217:441-6.
- [Google Scholar]
- EBUS: A new dimension in bronchoscopy. Of sounds and images – A paradigm of innovation. Respiration. 2006;73:583-6.
- [Google Scholar]
- Mediastinal bronchogenic cyst's recurrence treated with EBUS-FNA with a long-term follow-up. Eur J Cardiothorac Surg. 2006;29:627-9.
- [Google Scholar]
- Endobronchial ultrasound-guided transbronchial needle aspiration for the treatment of central airway stenosis caused by a mediastinal cyst. Eur J Cardiothorac Surg. 2007;32:538-40.
- [Google Scholar]
- Bronchogenic cyst treated by endobronchial ultrasound drainage. Thorax. 2008;63:386.
- [Google Scholar]
- Role of endobronchial ultrasound in the diagnosis of bronchogenic cysts. Diagn Ther Endosc 2011 2011 468237
- [Google Scholar]
- CT-guided percutaneous large-needle aspiration and bleomycin sclerotherapy for bronchogenic cyst: Report of four cases. J Vasc Interv Radiol. 2010;21:1045-9.
- [Google Scholar]






