Translate this page into:
Plexiform Neurofibroma in the Axilla with Intraosseous Neurofibroma in the Humerus in Neurofibromatosis 5
Address for correspondence: Dr. Sanjay Mhalasakant Khaladkar, Department of Radiodiagnosis, Dr. D. Y. Patil Medical College and Research Center, Dr. D.Y. Patil Vidyapeeth, Pimpri, Pune, Maharashtra, India. E-mail: drsanjaymkhaladkar@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Segmental neurofibromatosis type 5 (NF5) is a rare form of NF, in which the cutaneous and/or neural changes are confined to one region of the body. It is often underdiagnosed or undetected due to the absence of symptoms. Inheritance of NF is different from other types of NF. Intraosseous neurofibromas are rare tumors which develop from nerves supplying the periosteum or nerves following the intraosseous course. Plexiform neurofibroma with associated intraosseous neurofibroma is extremely rare. We report a case of plexiform neurofibroma in the left axilla of a 17-year-old female with associated intraosseous neurofibroma in adjoining left humerus.
Keywords
Intraosseous
neurofibromatosis
plexiform
segmental

INTRODUCTION
Neurofibromatosis (NF) is a common neurocutaneous disorder affecting approximately 1 in 3000 persons.[1]
Segmental NF type 5 (NF5) is a rare form of NF, in which the cutaneous and/or neural changes are confined to one region of the body. It is important to become familiar with this unusual disorder as the natural history and genetic of segmental types are different from other common forms of NF [Table 1]. Crowe et al. in 1956 first introduced the concept of segmental NF.[2] The diagnostic criteria of NF5 are unilateral neurofibromas limited to one or adjacent nerve roots, café au lait spots either absent or limited to the involved region and somatic mutation with resultant absence or marked reduction in genetic transmission.[2]

In contrast, NF 1 and NF 2 are autosomal dominant with 50% risk of acquiring disease in offspring of affected individuals. However, few cases of patients of NF 5 with their offspring having NF have been reported. The natural history, clinical manifestation, and inheritance of NF 5 are different from other types of NF and should be known so that this rare entity can be diagnosed in early stages.[2] There is the absence of family history of NF and absence of Lisch nodules. The natural history of NF5 is variable and depends on the severity of involvement and growth of the tumor. It usually presents with pain. Neurological deficit is less common. About 3%–13% of patients with NF 5 develop malignant peripheral nerve sheath tumors after latent period of 10–20 years. However, development of malignant nerve sheath tumors has not been reported yet in literature. These patients often present with pruritis caused due to large number of mast cells in neurofibromas which usually respond to antihistamines. As segmental NF is due to somatic mutation, it is usually not transmitted to offspring.[2]
Our case is unique, as there was no family history of NF, there was no systemic involvement, there were no café au lait spots in affected area, it was segmental in affection with no crossing of midline, and there were pressure erosions on humerus due to plexiform neurofibroma along with eccentric intramedullary lesions in humerus with thin sclerotic rim suggestive of associated intraosseous neurofibroma.
CASE REPORT
A 17-year-old female patient presented with pain in the left shoulder with restriction of overhead movements for 1 year. No clinically visible swelling in the left shoulder region. There were no skin changes in affected areas such as café au lait spots and axillary freckles.
Radiograph of the left glenohumeral joint anteroposterior (AP) and axial view showed multiple well-defined osteolytic lesions in the neck and proximal shaft of the humerus within the sclerotic margins with thin medullary cavity. Osteolytic lesions were also noted in the medial cortex of upper humeral shaft [Figure 1].
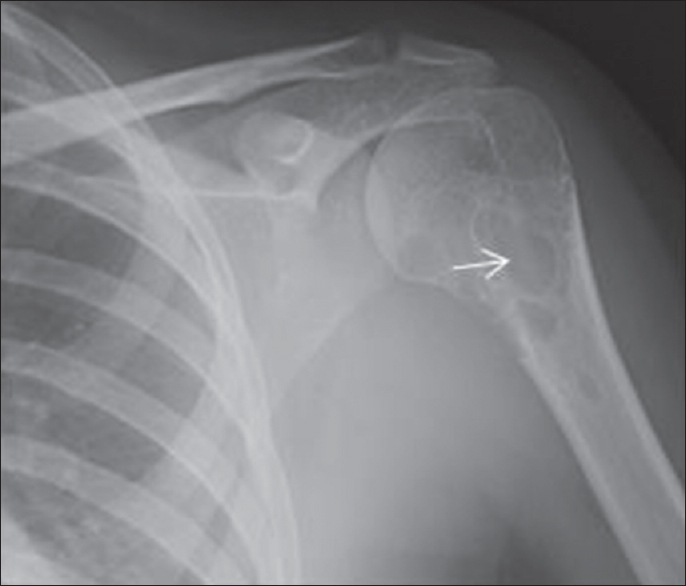
- A 17-year-old girl with neurofibromatosis who presented with pain in the left shoulder. Plain radiograph of the left shoulder anteroposterior view showing multilocular osteolytic lesion (arrow) in the left humerus involving metaphysis and upper shaft with sclerotic margins.
Local ultrasound of left shoulder with linear 7–12 MHz probe showed a well-defined hypoechoic solid mass with lobulated outlines measuring approximately 47 (L) × 19 (AP) × 50 (T) mm in relation to posteromedial aspect of humeral shaft without any cystic areas or calcification and significant vascularity. There was discontinuity in the cortex on posteromedial and posterolateral aspect of upper humeral shaft with an intraosseous well-defined hypoechoic soft-tissue lesion measuring approximately 32 mm × 25 mm [Figure 2a and b].

- A 17-year-old girl with neurofibromatosis who presented with pain in the left shoulder. (a) Ultrasound showing well-defined hypoechoic solid mass with lobulated outlines (arrow) in the left axilla suggestive of plexiform neurofibroma. (b) Ultrasound image showing discontinuity in adjoining cortex of upper humerus (red arrow).
Plain CT scan of left shoulder showed a well-defined soft-tissue density lesion (15–35 HU), slightly hypodense with respect to muscle with lobulated outlines measuring approximately 58 mm × 55 mm in the left axilla with extension along anterior, medial, and posterior aspect of upper humeral shaft. Multiple well-defined osteolytic lesions of variable sizes with sclerotic margins were noted in inferior portion of humeral head, upper metaphysis, and upper shaft [Figures 3 and 4].
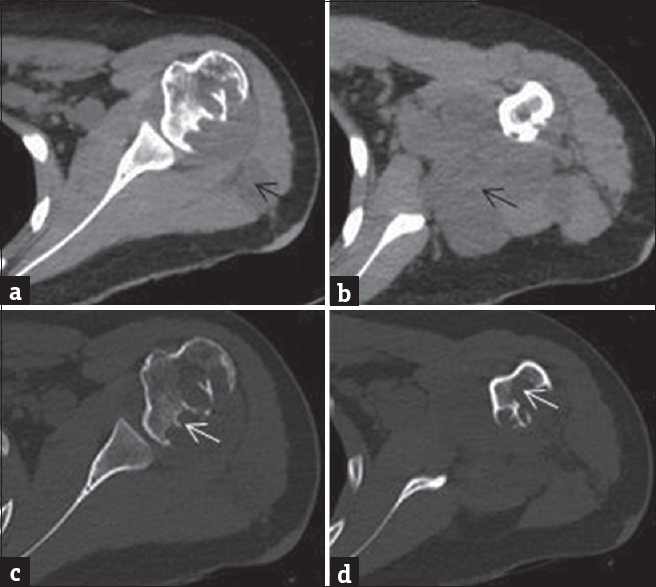
- A 17-year-old girl with neurofibromatosis who presented with pain in the left shoulder. (a and b) Plain computed tomography image of the left shoulder in soft-tissue window shows hypodense soft-tissue density mass with lobulated outlines (black arrow) in the left axilla extending in intermuscular fat planes suggestive of plexiform neurofibroma. (c and d) computed tomography image with bony window shows multilocular osteolytic lesions with sclerotic margins (white arrow) in adjoining humeral head and upper shaft suggestive of intraosseous neurofibroma.

- A 17-year-old girl with neurofibromatosis who presented with pain in the left shoulder. (a) Coronal and sagittal (b) plain computed tomography scan of left humerus at bony window showing multilocular osteolytic lesions (arrow) with sclerotic margins in adjoining humeral head and upper shaft suggestive of intraosseous neurofibroma.
Magnetic resonance imaging (MRI) of the left shoulder showed a large solid mass with lobulated outlines measuring approximately 69 mm × 56 mm × 50 mm in the left axilla extending both anterior and posterior to subscapularis, beneath infraspinatus and deltoid with extension in intermuscular fat planes, and involving infraspinatus and posterior fibers of deltoid. It was slightly hyperintense with respect to muscle on T1-weighted (T1WI), hyperintense on T2WI, and Proton density fat suppressed sequence. It was extending along anterior, medial, posterior aspect of inferior portion of humeral head, and upper shaft and showed multiple hypointense septations. Large intraosseous lesion measuring approximately 35 mm × 28 mm × 21 mm was noted involving posterior and medial cortex of upper humeral shaft, upper metaphysis, and posterior portion of lower humeral head with extension into medullary cavity. Diagnosis of plexiform neurofibroma in the left axilla was made with intraosseous neurofibroma [Figures 5 and 6].
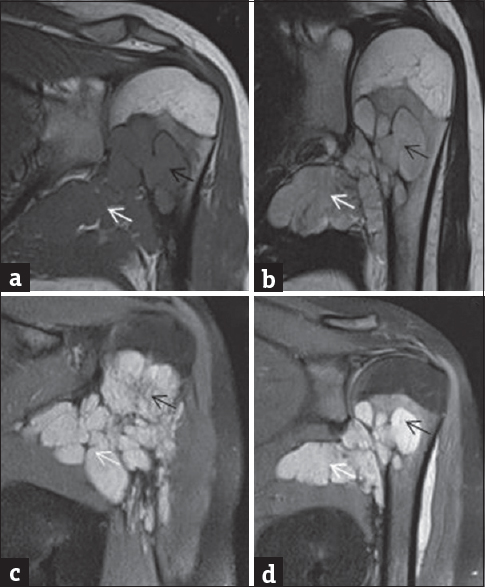
- A 17-year-old girl with neurofibromatosis who presented with pain in the left shoulder. (a) Magnetic resonance imaging left shoulder coronal T1 weighted showing plexiform neurofibroma in the left axilla (white arrow) and intraosseous neurofibroma (black arrow) in adjoining humerus appearing hypointense on T1 weighted. (b) Magnetic resonance imaging left shoulder coronal T2 weighted showing plexiform neurofibroma (white arrow) in the left axilla and intraosseous neurofibroma in adjoining humerus (black arrow) appearing hyperintense on T2 weighted. (c and d) Magnetic resonance imaging left shoulder coronal proton density fat suppressed sequence (PDFS) showing plexiform neurofibroma (white arrow) in the left axilla and intraosseous neurofibroma in adjoining humerus (black arrow) hyperintense on PDFS.

- A 17-year-old girl with neurofibromatosis who presented with pain in the left shoulder. (a and b) Magnetic resonance imaging left shoulder axial PDFS showing plexiform neurofibroma in the left axilla and adjacent to left humerus (white arrow), intraosseous neurofibroma (black arrow) in adjoining humerus appearing hyperintense on PDFS. (c and d) Magnetic resonance imaging left shoulder sagittal PDFS showing plexiform neurofibroma in left axilla and adjacent to left humerus (white arrow), intraosseous neurofibroma (black arrow) in adjoining humerus appearing hyperintense on PDFS.
It can be questioned whether the lesion (plexiform neurofibroma) originating from soft tissues has entered the humerus after causing pressure erosions. The plexiform neurofibroma arising in soft tissues is definitely causing pressure erosions on underlying humerus as destroyed cortex is curved inward due to compression by mass. However, the intraosseous lesions in underlying humerus are in the medullary cavity with thin sclerotic rim as seen on radiograph and computed tomography (CT) study. Intraosseous neurofibroma can arise in the periosteum, cortex, and medullary space. Eccentric location in medullary space is suggestive of neurofibroma arising from nerves supplying the periosteum or nerves following the intraosseous course.
Biopsy of soft-tissue lesion and intraosseous lesion was consistent with neurofibroma. On histopathology, the section showed a tumor showing stellate fibroblast with marked myxomatous changes with a delicate blood vessel lined by single layer of endothelial cells. Nuclear arrangement showed palisading at places with focal mononuclear infiltration. On immunohistochemistry, S100 was positive in tumor cells. Histopathological examination was suggestive of neurofibroma. The tumor cells were negative for CD34, desmin, DMA and CK, and expressed EMA and S100 protein. These are seen in neurofibroma. Plexiform neurofibromas show myxoid material along with benign stellate to spindle cells in cytology. Nerve sheath myxomas are S100 positive and EMA negative. The patient was advised surgical management; however, she left against medical advice.
DISCUSSION
Segmental NF was also called sectoral NF. Miller and Sparkes in 1977, renamed it as segmental NF.[3] Riccardi reclassified segmental NF as NF5 [Table 2].[4]
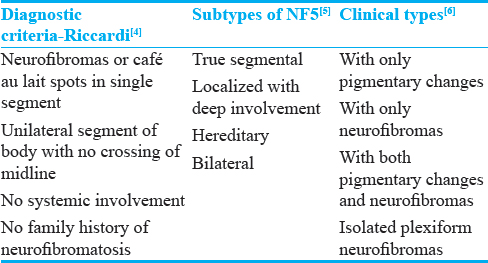
Segmental NF, sectoral NF, and NF5 are same. Segmental NF is divided into four subtypes by Roth et al.[5] [Table 2] Clinically, it is divided into 4 groups [Table 2].[6] Segmental NF is a rare disorder with prevalence between 0.0014% and 0.002%.[7] It is a form of mosaicism, in which localized disease occurs due to postzygotic NF1 gene mutation located in proximal long arm of chromosome 17. Gene mutation can occur in both somatic and gonadal cell lines. Gonadal mosaicism is responsible for reports of patients with segmental NF having children with generalized NF Type I.[7] It is often underdiagnosed or undetected due to the absence of symptoms.
Segmental NF has been described in 82 patients worldwide with median age of onset of 28 years. They have a low risk of passing the disease to offspring.[8]
The neurofibromas are typically asymptomatic. They extend in estimate from 0.1 cm to a few cms in distance across. They emerge in dermatomal dispersion, normally cervical, trailed by thoracic, lumbar, and sacral locale. Café au lait macules and axillary freckles are the pigmentary changes of which former are more typical.[6]
Abnormalities noted in musculoskeletal system in NF are anterolateral bowing of tibia/fibula; pseudoarthrosis; atrophic/thinned/absent fibula, radius and ulna; subperiosteal hemorrhage due to easy detachment of periosteum from the bone with endosteal sclerosis; intramedullary longitudinal streaks of increased density; single or multiple bone cysts or deossification/nonossification; multiple nonossifying fibromas; intraosseous neurofibromas; bone erosions from adjacent neurofibromas; focal gigantism of digit or entire limb; disorders of growth/hypertrophy/atrophy; scoliosis; and congenital abnormalities.[910]
Intraosseous neurofibromas are rare tumors which develop from nerves supplying the periosteum or nerves following the intraosseous course. On imaging, it reveals as osteolytic lesion with well-defined margins bordered by a layer of sclerotic bone. In long bones, it is often eccentric. Persistence of bony ridges gives a multilocular appearance. Subperiosteal hemorrhage cause pseudocystic lesions. The long bones affected in NF are the femur, humerus, tibia, jaw bones, less frequently pelvic bones, fibula, radius, and ulna.[11]
Ultrasound is useful in detecting plexiform neurofibroma which shows lobulated outlines and pressure erosions in adjoining bone. CT is useful in better detection of pressure erosions in underlying bony cortex and eccentric osteolytic lesions in adjoining medullary cavity with thin sclerotic margins. MRI can detect plexiform neurofibroma with its extent, pressure erosions in adjoining cortex and intraosseous bony lesions.
Bony lesions associated with NFM-5 are pressure erosions, intraosseous cysts, nonossifying fibromas, and intraosseous neurofibromas. Isolated NF5 can go undetected. Nonossifying fibromas are multiloculated, located eccentrically in the metaphysis adjacent to the growth plate with thin sclerotic rim. No periosteal reaction or cortical breach or associated soft-tissue component noted. Nonossifying fibromas and intraosseous neurofibromas can appear similar on MRI. Differentiation between nonossifying fibroma and intraosseous neurofibromas can be done on histopathology and immunohistochemistry.
CONCLUSION
Segmental NF5 is a rare form of neurofibromatosis. Isolated segmental NF5 and intraosseous neurofibroma are rare. Plexiform neurofibroma with associated intraosseous neurofibroma is extremely rare. Multilocular osteolytic lesion with well-defined sclerotic margins with associated soft-tissue component should raise suspicion of segmental NF.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/3/224246
REFERENCES
- Clinical, Pathological, and Genetic Study of Multiple Neurofibromatosis. Springfield (IL): Charles C Thomas; 1956. p. :153-4.
- Segmental neurofibromatosis: A report of 3 cases. Indian J Dermatol. 2010;55:105-8.
- [Google Scholar]
- Solitary intraosseous neurofibroma of the mandible. Zahedan J Res Med Sci. 2014;16:42-4.
- [Google Scholar]
- Solitary intraosseous neurofibroma of the tibia. Skeletal Radiol. 2005;34:303-6. 2005;11:20
- [Google Scholar]






