Translate this page into:
Horizontal Long Axis Imaging Plane for Evaluation of Right Ventricular Function on Cardiac Magnetic Resonance Imaging
Address for correspondence: Dr. Abhishek Chaturvedi, Department of Radiology, University of Washington School of Medicine, 1959 Pacific Street, Seattle, WA, USA. Department of Imaging Sciences, University of Rochester, 601 Elmwood Avenue, Rochester, NY, USA. E-mail: toabhic@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Purpose:
The purpose of this study was to evaluate a horizontal long axis (HLA) magnetic resonance imaging (MRI) plane aligned to the long axis of the right ventricular (RV) cavity for functional analysis by comparing the measurement variability and time required for the analysis with that using a short-axis (SAX) image orientation.
Materials and Methods:
Thirty-four cardiac MRI exams with cine balanced steady-state free precession image stacks in both the SAX and the HLA of the RV (RHLA) were evaluated. Two reviewers independently traced RV endocardial borders on each image of the cine stacks. The time required to complete each set of traces was recorded, and the RV end-diastolic volume, end-systolic volume, and ejection fraction were calculated. Analysis times and RV measurements were compared between the two orientations.
Results:
Analysis time for each reviewer was significantly shorter for the RHLA stack (reviewer 1 = 6.4 ± 1.8 min, reviewer 2 = 6.0 ± 3.3 min) than for the SAX stack (7.5 ± 2.1 and 6.9 ± 3.6 min, respectively; P < 0.002). Bland–Altman analysis revealed lower mean differences, limits of agreement, and coefficients of variation for RV measurements obtained with the RHLA stack.
Conclusions:
RV functional analysis using a RHLA stack resulted in shorter analysis times and lower measurement variability than for a SAX stack orientation.
Keywords
Analysis time
magnetic resonance imaging
observer variability
right ventricle
ventricular function

INTRODUCTION
Cardiac magnetic resonance (CMR) imaging is currently considered the reference imaging modality for quantitative evaluation of right ventricular (RV) size and function.[1] With clinical CMR exams, ventricular function is typically derived using the modified Simpson's rule[2] applied to contour tracings of the endocardial surface of the ventricle of interest. These endocardial contours are traced on the end-diastolic and end-systolic frames of each cine image of a sequential stack of CMR cine images covering the complete extent of the ventricle.[3] With manual endocardial tracing, functional analysis requires dedicated operator or physician time at a workstation, and can vary depending on ventricular size, ventricular shape, and visibility of the endocardial margins.[4]
There is a growing interest in evaluating the RV by magnetic resonance (MR).[5] The RV's position behind the sternum and its complex geometric shape makes it difficult to accurately obtain RV function by echocardiography.[2] While no standard imaging plane has been defined for the functional assessment of the RV,[6] the majority of reports that present MR reference values for RV function have utilized the short-axis (SAX) cine stack, which is prescribed orthogonal to the long axis of the left ventricle (LV).[78910] Evaluation of the right heart function on a SAX cine stack, however, can be challenging due to difficulties delineating the tricuspid valve plane on the basilar images of a SAX cine stack combined with marked through-plane motion of the RV during systole [Figure 1].[13]
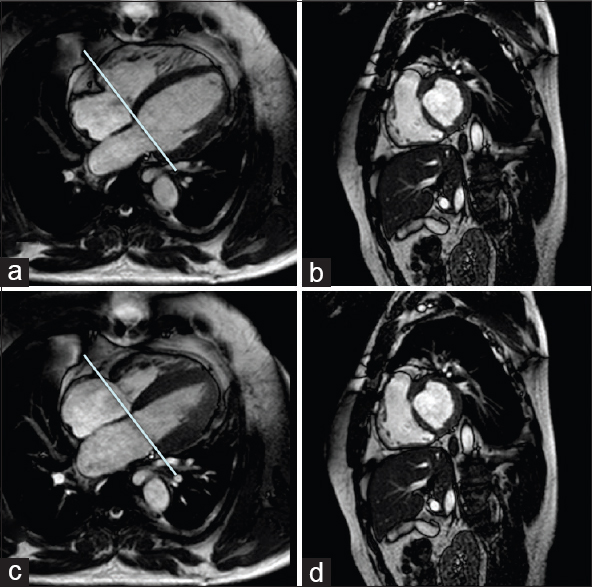
- Limitations of the short-axis orientation for right ventricular functional analysis. Short axis (b and d) and horizontal long axis (a and c) balanced steady-state free precession cardiac magnetic resonance images of the heart: diastole (a and b) and systole (c and d). The straight line on the horizontal long axis images (a and c) depicts the location of the corresponding basilar short-axis image in diastole (c) and at the same location with the ventricle in systole (d). Example illustrates the apical displacement of the tricuspid valve plane with systole (d) and the thin wall of the right ventricle that can be difficult to distinguish from the right atrium on the short-axis orientation (b and d).
In comparison to a SAX stack, an alternative imaging orientation aligned with the horizontal long axis of the RV (RHLA) could, in theory, improve visualization of the tricuspid valve throughout the cardiac cycle, better define RV contraction to identify end-systole, and require fewer slices to image the craniocaudal extent of the RV.[3111213] These potential advantages could lead to improved measurement variability of RV function and shorter analysis times. The purpose of this study was to evaluate the use of a horizontal long axis imaging plane aligned with the right ventricle (right horizontal long axis; RHLA) for RV functional analyses by comparing the measurement variability and time required for analyses performed with RHLA cine stack with analyses done using a the conventional SAX stack orientation.
MATERIALS AND METHODS
Patients
With the Institutional Review Board approval, the clinical CMR exam log over a 2-year period was reviewed to identify 39 sequential clinical cardiac MR imaging (MRI) exams that contained both a RHLA and SAX cine steady-state free precession (SSFP) stack to image the right heart. All patients were adults. Five of these exams were excluded because either the RHLA or SAX cine stack of SSFP images did not cover the entire RV. Indications for the 34 included CMR study exams were RV function for congenital heart disease (CHD) (n = 19), cardiomyopathy (n = 11), pulmonary hypertension or stenosis (n = 3), and right-sided cardiac mass (n = 1). The adult congenital heart abnormalities imaged were repaired tetralogy of Fallot (n = 14), transposition of the great vessels (n = 2), and Ebstein's anomaly, double-inlet LV, and repaired truncus arteriosus (one each).
Cardiac magnetic resonance imaging
All exams were performed on a 1.5T clinical MR scanner using a dedicated 5-channel cardiac coil (Philips Medical System ViewForum, Best, The Netherlands). Typical parameters for the cine balanced SSFP (bSSFP) sequence utilized for RV functional assessment were echo time 1.7 ms, repetition time 3.4 ms, flip angle 55°, cardiac phases 25, retrospective triggering, slice thickness/gap of 6/4 or 8/2 mm (24 exams with 6/4 mm prescription, 15 with 8/2 mm), field of view 360 mm, matrix 160 × 160, acquired voxel size 2.25 × 2.28 × 6–8 mm.
The conventional SAX cine stack was prescribed from LV vertical long axis (VLA) and horizontal long axis (HLA) single slice cine images. The plane of the SAX cine stack was oriented perpendicular to the interventricular septum, and the number of slices within the stack was adjusted to cover both ventricles from the apex through the atrioventricular valve plane.[14] The RHLA cine stack, in comparison, was prescribed to align with the HLA of the RV. To prescribe the RHLA cine stack, two single slice cine bSSFP long axis images were first obtained to better define the craniocaudal extent and angulation of the long axis of the RV.[15] The first of these two planning images was defined somewhat analogous to the VLA of the LV from an axial image by prescribing a single oblique coronal cine bSSFP slice positioned to pass through the middle of the tricuspid valve and the middle of the pulmonic valve, directed toward the RV apex (RVLA) [Figure 2a]. The second RV planning image is the standard oblique sagittal plane running through the RV outflow tract (RVOT) centered within and parallel to the main pulmonary artery [Figure 2b]. Using these two planning images (RVLA and RVOT), the RHLA stack is prescribed parallel to the RHLA, with the most superior slice placed above the pulmonic valve and the image stack extending below the inferior border of the RV [Figure 3].
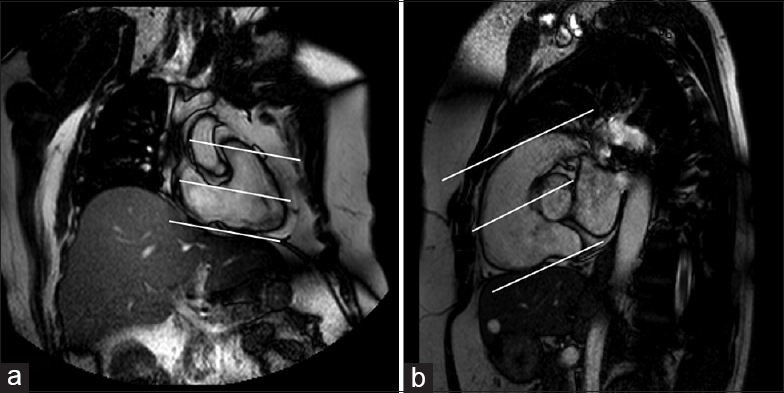
- Acquiring the right horizontal long axis cine stack. A stack of parallel cine balanced steady-state free precession images (straight lines) is aligned parallel to the horizontal long axis of the right ventricle on the right ventricle long axis (a) and sagittal right ventricle outflow tract (b) images, which allow determination of the level of the pulmonic valve and the obliquity of the inferior wall of the right ventricle.
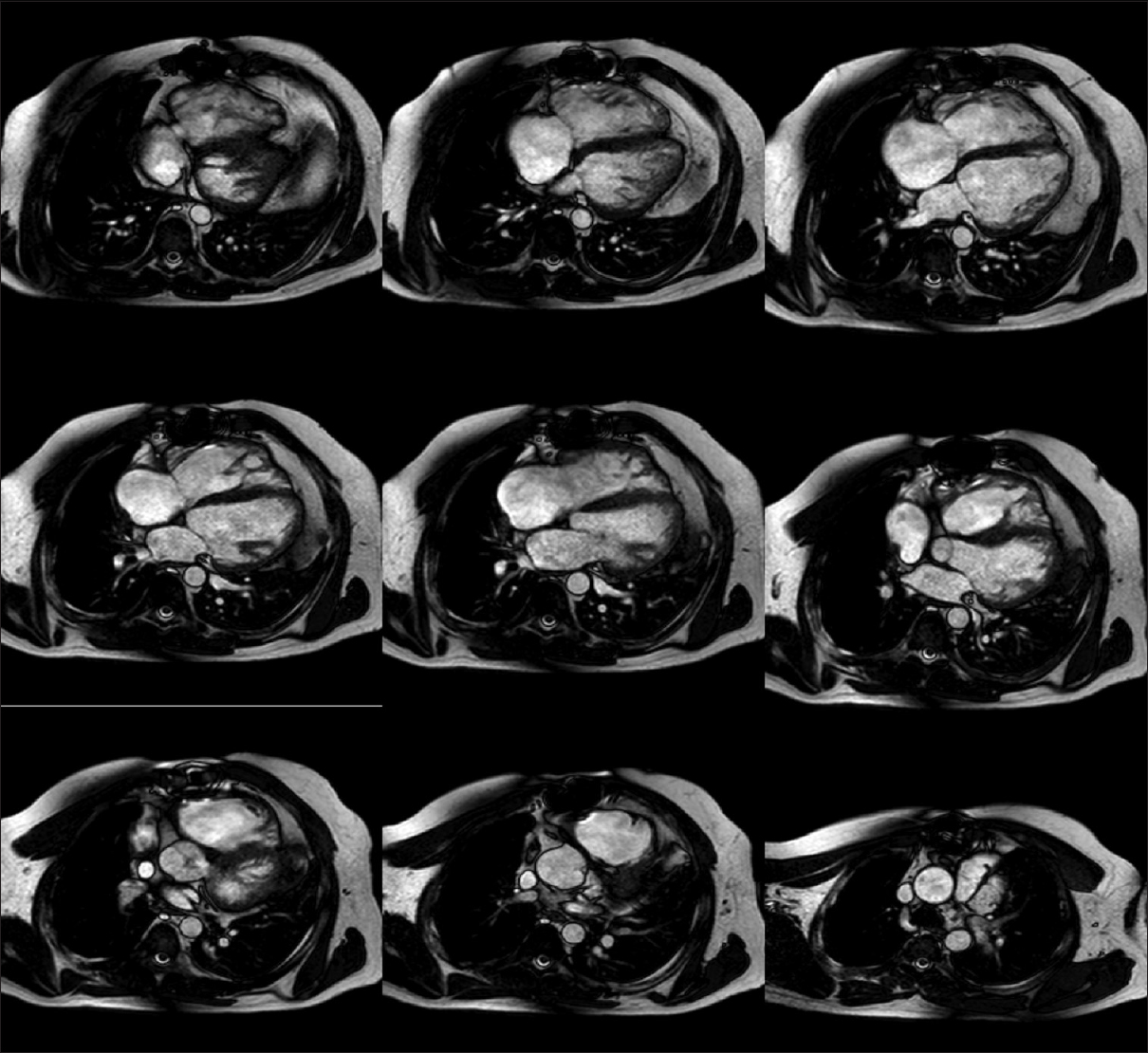
- Right horizontal long-axis cine stack obtained from the right ventricle long axis and right ventricle outflow tract. It extends from above the pulmonic valve to below the inferior border of the right ventricle.
Image analysis
Two radiologists (JW, LM) with 1 and 4 years of experience in CMR imaging separately performed the image analysis using commercially available software on an independent workstation (Philips Medical System ViewForum, Best, The Netherlands). The SAX and RHLA cine stacks from the clinical CMR exams included in the study were de-identified and then randomly and independently evaluated by the two reviewers.
Each reviewer subjectively assessed the image quality of each cine stack of RV images (RHLA and SAX) using a four-point scale: (0) unevaluable - poor visualization of RV endocardial margins, unable to perform quantitative analysis; (1) marginal - majority of the RV margins were blurred, analysis will likely be inaccurate; (2) satisfactory - only a few margins or images blurred; and (3) excellent - good exam quality with minimal to no RV margins being blurred.
The reviewers then independently performed RV functional analysis on both the cine stacks (SAX and RHLA) by first selecting the end-diastolic and end-systolic images, then manually tracing the RV endocardial contours. Trabeculations and papillary muscles were included within the RV blood pool.[16] The uppermost slice was the last image containing RV outflow tract blood pool signal below the pulmonic valve.[3] On basal SAX slices, blood volume was included with the RV cavity when it was surrounded by 50% or more by ventricular myocardium,[3] with attempts made not to include right atrium on the SAX stack (paging through the phases of each cine image and between sequential image locations within a cine stack was allowed to facilitate discrimination between the right atrium and RV). In the most inferior slice of the RHLA stack, in cases where there was significant partial voluming of RV muscle, the border was typically drawn halfway between the bright blood and outer ventricular borders. RV functional measures were then computed using clinically available software (Philips Medical System ViewForum, Best, The Netherlands). The following computed values were recorded for each cine stack: end-diastolic volume (EDV), end systolic volume (ESV), and ejection fraction (EF).
Each reviewer also tracked the total time required for RV functional analysis with each cine stack. The start of the analysis was specified as the time point when the exam had been set up for viewing on the workstation (series selected, images centered within the viewing panel, and appropriate magnification specified), but before selection of the end-systolic and end-diastolic phases. The end of the analysis was defined as the time point at completion of the last RV endocardial contour trace.[17] At the end of each cine stack analysis, the reviewer screensaved the RV endocardial traces. A third reviewer (AC), who was not involved with the functional analysis, then viewed the saved endocardial traces and recorded the number of slices that contained a drawn endocardial contour. The number of contour containing slices was used to compare the slices needed to cover the entire RV for each of the two stack orientations (SAX and RHLA).
Statistical analysis
Paired t-tests were used to make inferences for the differences in means comparing RVHLA and SAX in the following measures: EDV, ESV, EF, number of slices, analysis time. Wilcoxon matched-pairs signed-rank tests were used to compare exam quality. The agreement between methods and the agreement between reviewers were evaluated using Pearson's correlation coefficient with a Fisher's Z-test transformation to obtain 95% confidence intervals and Bland–Altman analysis.[18] Coefficients of variation (CoV) were calculated by dividing the standard deviation of the measurement differences by the mean of the measurements. Agreement in the selection of the end-systolic phase between the two cine stack orientations (RHLA or SAX) was determined by a weighted Cohen's kappa statistics.
RESULTS
There was no significant difference in the mean exam image quality scores between the two imaging sets for each reviewer [Table 1]. Reviewer 1 rated one SAX exam marginal (score = 1). Reviewer 2 scored one RHLA stack and three SAX stacks as marginal. No exams were scored as unevaluable.
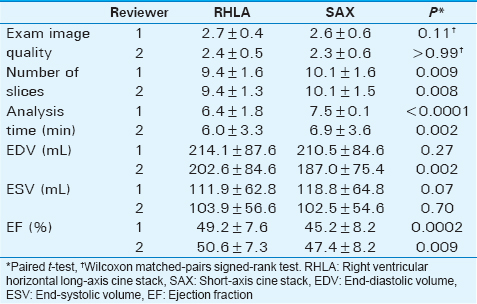
The RV functional measures, number of slices traced, and analysis times for the RHLA and SAX cine stacks are summarized for each reviewer in Table 1. Average number of slices needed to perform the functional analysis with the RHLA cine stacks was 9.4 slices for both reviewers, which was significantly lower than the number of slices required for analyses performed on the SAX cine stacks (10.1; P < 0.01). For both reviewers, the time required for RV analysis was significantly shorter with the RHLA than for the SAX cine stacks (P < 0.002).
Agreement between methods (right horizontal long axis vs. short axis)
Analysing each reviewer independently [Table 1] revealed no significant difference in the EDV derived with the RHLA cine stack versus the volume obtained with the SAX stack for reviewer 1 (P = 0.27) although the EDV for reviewer 2 was found to be significantly lower with the SAX data than the RHLA imaging plane (P = 0.002). No significant difference was found for the ESV obtained from the two cine stacks each reviewer (reviewer 1, P = 0.07; reviewer 2, P = 0.7) or as a combined set (P = 0.3). Combining both reviewers, the EF was lower by an average value of 3.6 ± 6.1% when obtained from the SAX cine stack than that from the RHLA cine stack (P < 0.0001). There was moderate agreement between the SAX and RHLA cine stack orientations for the selection of the end-systolic phase (weighted Kappa 0.56, P < 0.001).
The correlation between the RV functional measures obtained from the SAX and RHLA cine stacks for each reviewer is summarized in Table 2. Bland–Altman analysis between methods [Table 2 and Figure 4] for the two reviewers revealed a general positive bias for the RHLA results with the largest bias found being 15.6 ml (EDV by reviewer 2).
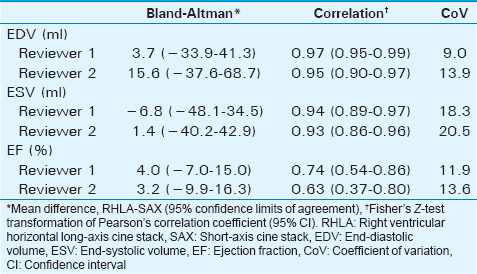
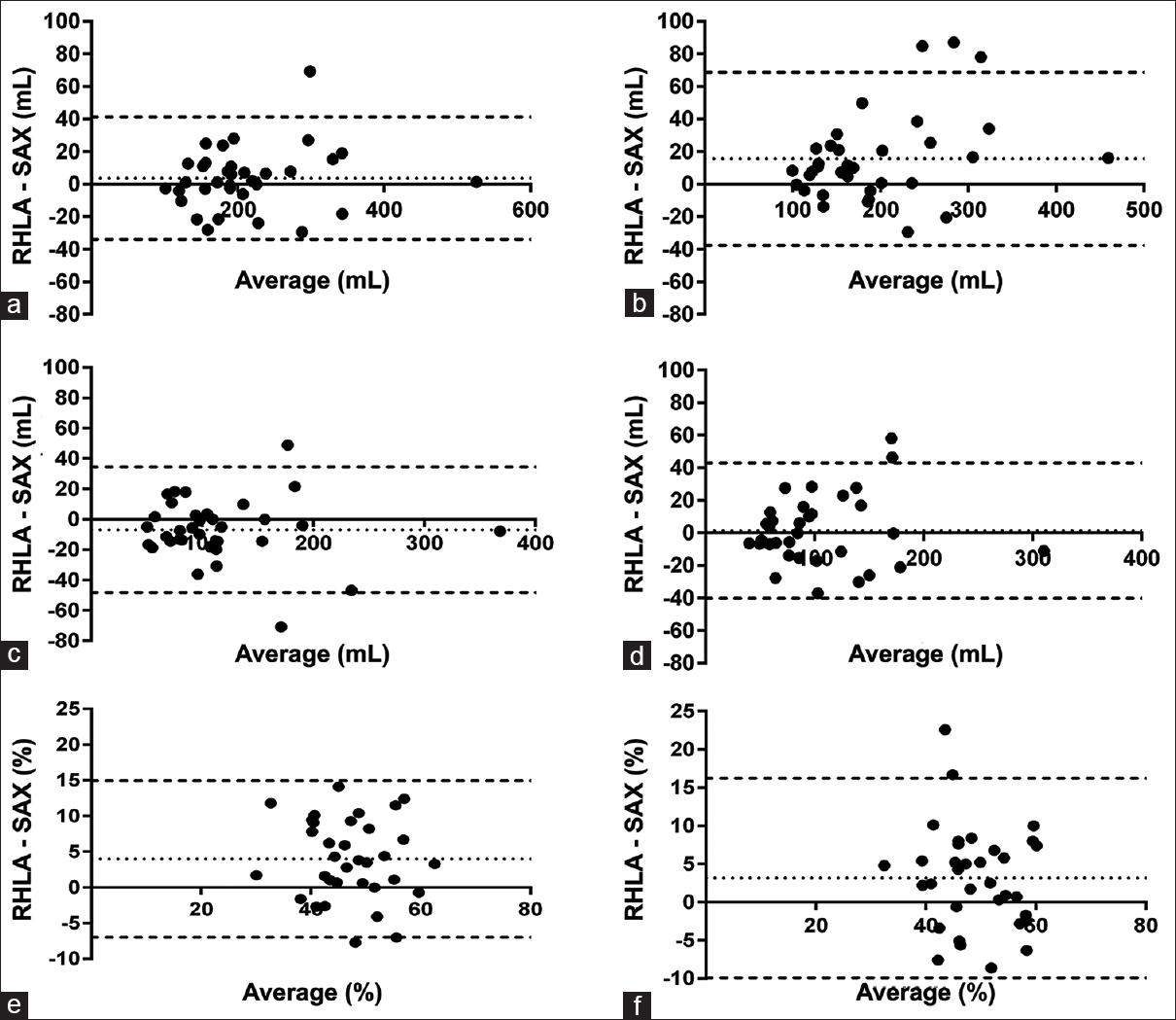
- Bland–Altman plots of the mean difference between methods for (a) end-diastolic volume, reviewer 1, (b) end-diastolic volume, reviewer 2, (c) end-systolic volume, reviewer 1, (d) end-systolic volume, reviewer 2, (e) ejection fraction, reviewer 1, and (f) ejection fraction, reviewer 2. Dotted lines represent the mean difference for each right ventricle functional measurement, and dashed lines depict the upper and lower limits of agreement.
Agreement between reviewers (reviewer 1 vs. reviewer 2)
The correlation of the RV functional metrics (EDV, ESV, EF) between reviewers was greater when obtained from the RHLA cine stacks than when obtained from the SAX cine stacks [Table 3] although the difference in the degree of correlation did not reach significance. Bland–Altman analysis performed between reviewers (reviewer 1 and reviewer 2) for each RV functional measure revealed no systematic error with respect to RV volumes or EF [Table 3 and Figure 5]. The functional measures obtained from the RHLA cine stacks had lower mean differences, narrower range of agreement, higher correlation, and lower CoV than the metrics obtained with the SAX cine stacks [Table 3].
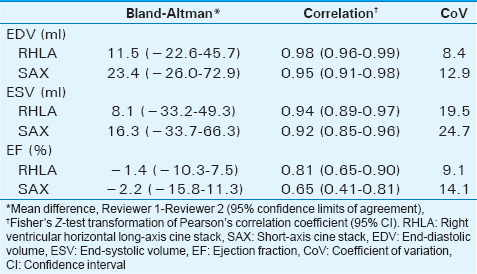
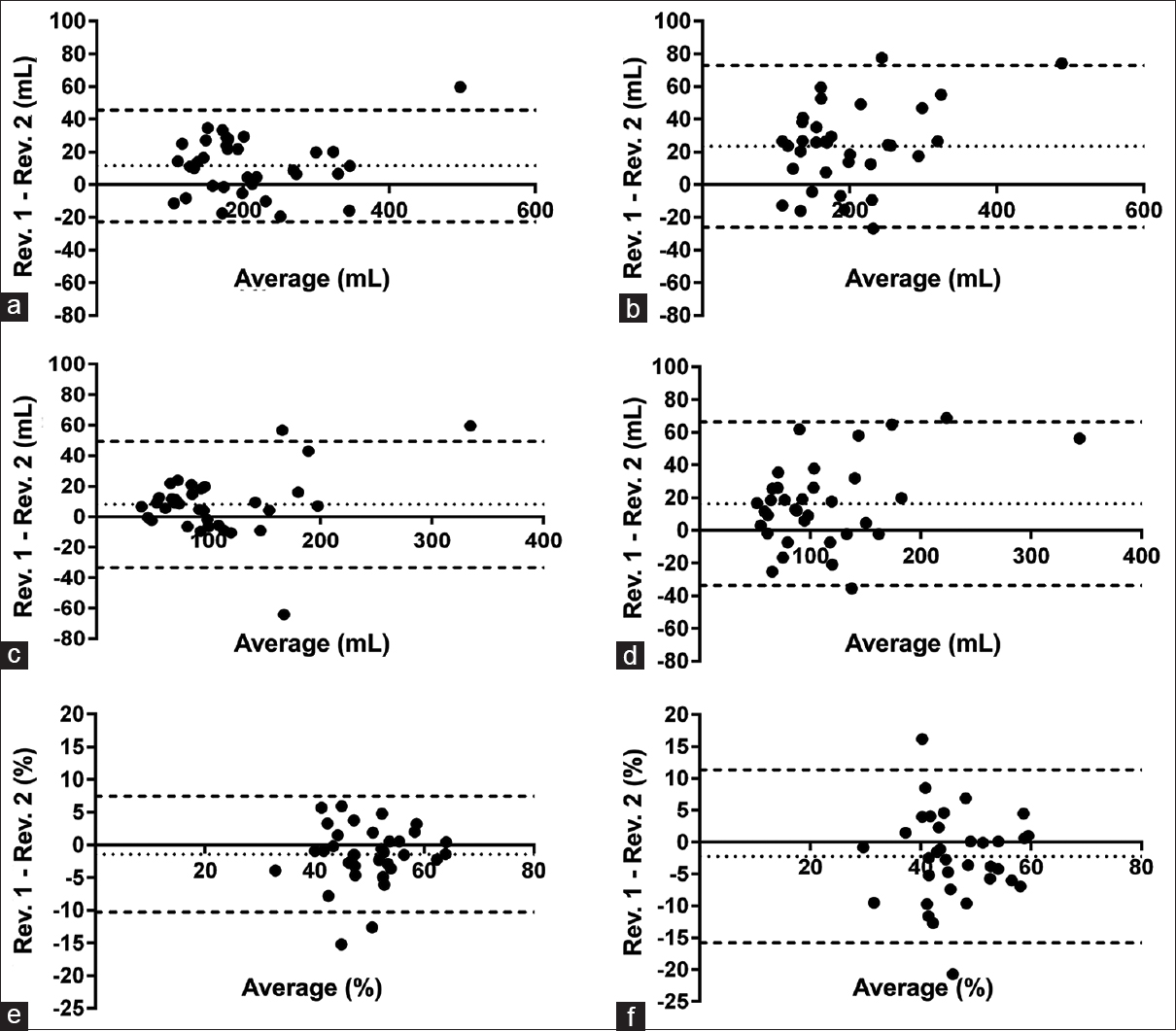
- Bland–Altman plots of the mean difference between reviewers (a) end-diastolic volume, right horizontal long axis, (b) end-diastolic volume, short axis, (c) end-systolic volume, right horizontal long axis, (d) end-systolic volume, short axis, (e) ejection fraction, right horizontal long axis, and (f) ejection fraction, short axis. Dotted lines represent the mean difference for each right ventricle functional measurement, and dashed lines depict the upper and lower limits of agreement.
DISCUSSION
While standardized imaging planes have been defined for noninvasive evaluation of LV function, there is currently no consensus as to the optimal imaging plane for the MR assessment of the RV.[6] As a result, different imaging planes are used in practice, including plane orientations that are not aligned with the RV. The RV shape is complex, with predominant contraction occurring in the longitudinal plane, with additional radial contraction and traction secondary to LV contraction.[1920] We examined the use of a cine stack aligned with the RHLA for evaluating RV function, based on the premise that accuracy and interobserver variability are important issues as CMR is increasingly used for serial evaluation of CHD, and changes in RV measurements help drive clinical decisions on the timing of therapeutic interventions.
The SAX plane is routinely obtained as a part of most CMR studies due to its wide application for LV analysis[3] and because it can be used for RV functional analysis, obviating the need to acquire a separate RV analysis imaging plane. The more complex shape and orientation of the RV, however, can make evaluation of RV function on SAX images less reliable than that of the LV. The dominant direction of RV shortening is along the long axis of the ventricle,[3] with the largest longitudinal displacement occurring at the RV base.[21] As such, the tricuspid valve plane and RV outflow tract often move into and out of the basal SAX images during the cardiac cycle[22] [Figure 1], making it difficult to be certain which side of the tricuspid valve a particular slice is positioned. As a further complication, the septal insertion of the tricuspid valve is more apically positioned than the mitral valve, and as a result, the SAX orientation often traverses the tricuspid valve obliquely,[11] creating a basal RV image that can contain portions of both the right atrium and RV [Figure 1]. Finally, differentiation between the right atrium and ventricle is difficult because of the typically thin RV wall (although not necessarily true in CHD, >50% of the cases in this study). Since the basal RV images represent relatively large ventricular volumes, any inaccuracy in defining the endocardial contour and extent of the basilar RV can result in appreciable measurement error. Thus, improving the delineation of the right atrioventricular valve plane on CMR exams could potentially reduce measurement variability and shorten analysis times by lessening the time required for endocardial trace modifications.[323]
In this study, RV functional assessment using a RHLA stack demonstrated lower interobserver variability, shorter analysis times, and a fewer number of slices to completely image the RV as compared to assessment performed with a SAX stack. Geometrical alignment of the RHLA cine stack with the long axis of the RV explains the fewer necessary slices to image the entire RV. While a lower number of images requiring endocardial traces will shorten analysis times, the time efficiency related to improved visualization of the RV base is difficult to define.
Comparing the functional metrics between the RHLA and SAX cine stacks obtained in this study, there was no significant difference in RV volumes (EDV, ESV). This supports the interchangeable use of normative RV volume ranges derived from SAX cine stacks with those from the alternative long axis cine stack (RHLA) orientation presented here. In contrast to the volumetric measurements, however, a significant difference in RVEF (3.6 ± 6.1%) was found between the two methods. This could not be entirely explained by the selection of the end-systolic frame on the different cine stacks, and likely relates to the fact that the EF is calculated from two independent measurements (EDV, ESV), and any error in ventricular volumes is propagated and amplified by the EF calculation.[1] While statistically significant, this small numerical difference in EF is likely not clinically significant and is less than the measurement variability reported elsewhere (5.5–6.4 EF%;[17] 8.3 EF%[1]).
The interobserver variability of RV functional measurements obtained using RHLA cine stacks as expressed by the CoV (RVEDV 8.4%, RVESV 19.5%, and RVEF 9.1%) were similar to other CMR reproducibility studies that reported CoV values and included patients with heart disease, and better than those same measurements for SAX (RVEDV 12.9%, RVESV 24.7%, RVEF 14.1%). Mooij et al. studied sixty patients (twenty normals, twenty with atrial septal defect, and twenty with repaired tetralogy of Fallot), in which RV function was assessed on SSFP-SAX cine stacks by two reviewers and reported interobserver CoVs of RVEDV 6.4%, RVESV 13.0%, and RVEF 8.0%.[17] Grothues et al.[1] evaluated RV function with a FLASH-SAX cine stack of sixty subjects (twenty healthy volunteers, twenty with LV hypertrophy, and twenty with stable congestive heart failure) performed by a single experienced reviewer and reported interstudy CoVs of RVEDV 6.2%, RVESV 14.1%, RVEF 8.3%.
Comparing time efficiency between various CMR imaging planes is convoluted by differing methodologies, analysis software, and reviewer experience in the few studies that include the analysis times. Average analysis times for biventricular evaluation on SSFP SAX image stacks in one combined group of volunteers and patients ranged from 31 to 54 min.[17] In another study, 29 patients with a systemic RV, mean RV analysis time for functional assessment on bSSFP SAX image stacks (9–15 slices) was 20 ± 3 min although the observer experience level was not stated.[16] A third study of 52 volunteers and 325 cardiac patients reported biventricular analysis time between 15 and 20 min on SAX 2D FLASH images by a single skilled observer.[8] A fourth study of 10 volunteers reported an analysis time for RV analysis with 2D-cine SSFP cine data of 15.9 ± 2.9 min.[24] The mean RV analysis time for the cases included in this study ranged from 6.0 to 7.5 min, which is on the lower end for those reported (making the best case assumption that each ventricle requires half the time reported for a biventricular analysis).
Other alternative imaging planes for RV functional analysis that have been compared to SAX include a true axial (transverse to the chest)[3] and a modified RV SAX (aligned perpendicular to the RV outflow tract).[11] The axial plane reduced the number of required slices, resulting in more reproducible RV functional measures than with SAX.[3] Due to individual variation in the craniocaudal obliquity of the right heart relative to the chest, however, use of the axial plane can alter the perceived shape of the RV,[12] thereby potentially necessitating more slices to cover the right heart than a true RHLA. In their evaluation of 50 patients using a modified RV SAX imaging plane, Strugnell et al.[11] calculated the RV stroke volume and compared the results to the RV and LV stroke volumes obtained from SAX image stacks. Based on better agreement between RV and LV stroke volumes, the authors concluded that the modified RV SAX orientation improved RV volume analysis over the SAX orientation but did not include data on EDV, ESV, EF, or analysis time in their report to allow comparison with the results of our and other studies.
There are several disadvantages to the RHLA-based RV functional analysis proposed in this report. First, since the RHLA stack images the inferior RV wall tangentially, it may be difficult to accurately detect the blood pool due to partial voluming artifact. We handled this by choosing a contour approximately halfway between the blood pool and epicardial border (easily standardizable). Based on the decreased CoV for the RHLA versus SAX measurement, this does not appear to be a significant limitation to our reproducibility. Whether there is greater measurement error than the SAX cannot be determined as no true standard for RV EDV or ESV is available. Furthermore, the RHLA plane limits the ability to quantify RV mass,[25] and this may have to be measured on the SAX series. Second, acquisition of an additional cine imaging stack does lengthen the exam time. While the RHLA acquisition time was not measured in this study, one report described a second alternative cine image stack required <5 min,[3] and we believe that to be a good estimate for our RHLA acquisition. Since RHLA analysis time was only approximately 1 minute faster on average than for SAX [Table 1], there is undoubtedly a net increase in total exam plus processing time. Thus, to gauge whether this constitutes a good use of resources, three questions must be considered: (a) is decreasing interobserver variability clinically important, (b) does the cost-benefit of additional MR table time outweigh the smaller time savings on the processing end (which may in turn depend on who performs the processing – perhaps changing depending on whether this is a physician vs. technologist), and (c) is there added value having an additional RHLA series available for morphologic or functional evaluation? These are likely site and personal preference questions. At our institution, the interpreting physician performs the postprocessing, and we have several different providers reading CMR and following CHD patients in whom serial changes in RV functional metrics, particularly RVEDV, are deemed important. Commenting on the potential added value of the RHLA cine imaging itself, particularly in CHD patients, is beyond the scope of this work although we have anecdotally found it helpful on numerous occasions as these views provide additional and better visualization of the tricuspid and pulmonic valves-often abnormal in conditions involving the right heart. While we are not advocating that the current CMR practice standard should be altered to add an additional RHLA stack for RV function analysis, we are merely illustrating the potential merits of the approach.
This study has several potential limitations. The first is the small sample size although the heterogeneous patient population may make these results more generalizable as compared to analyses done with a more limited spectrum of cardiac disease. Although this study included a generous proportion of patients with RV disease, specific groups of patients may have different RV analysis errors related to the size and morphology of the RV.[17] Further recruitment and larger number of cases with a specific RV disease category will be needed to define the measurement error for each category of disease. Second, during the period of this study, patient's height and weight were not recorded and RV functional analysis results could not be normalized to body surface area. Finally, since the analysis time and measurement variability decrease with observer experience, some of the results may reflect the different experience levels of the two reviewers.[26]
CONCLUSION
In this broad spectrum of clinical cases, RV functional analysis using a cine image plane aligned with the RHLA demonstrated lower interobserver variability than the same analyses using a conventional SAX scan orientation. This may be useful when designing scan protocols for the quantitative CMR surveillance of patients with right heart disease. Finally, RHLA analysis itself was more time efficient than that of SAX although the extra-time required to acquire the RHLA cine stack makes the total CMR exam plus analysis time invested greater.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/52/197076
REFERENCES
- Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J. 2004;147:218-23.
- [Google Scholar]
- Comparison of right ventricular volume measurements between axial and short axis orientation using steady-state free precession magnetic resonance imaging. J Magn Reson Imaging. 2003;18:25-32.
- [Google Scholar]
- Reproducibility of MRI-derived measurements of right ventricular volumes and myocardial mass. Magn Reson Imaging. 1995;13:53-63.
- [Google Scholar]
- Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539-42.
- [Google Scholar]
- Normal human left and right ventricular dimensions for MRI as assessed by turbo gradient echo and steady-state free precession imaging sequences. J Magn Reson Imaging. 2003;17:323-9.
- [Google Scholar]
- Right ventricular volumes and ejection fraction with fast cine MR imaging in breath-hold technique: Applicability, normal values from 52 volunteers, and evaluation of 325 adult cardiac patients. J Magn Reson Imaging. 1999;10:908-18.
- [Google Scholar]
- Reference right ventricular systolic and diastolic function normalized to age, gender and body surface area from steady-state free precession cardiovascular magnetic resonance. Eur Heart J. 2006;27:2879-88.
- [Google Scholar]
- Normal human left and right ventricular and left atrial dimensions using steady state free precession magnetic resonance imaging. J Cardiovasc Magn Reson. 2005;7:775-82.
- [Google Scholar]
- Modified RV short axis series – A new method for cardiac MRI measurement of right ventricular volumes. J Cardiovasc Magn Reson. 2005;7:769-74.
- [Google Scholar]
- Right ventricle shape and contraction patterns and relation to magnetic resonance imaging findings. J Comput Assist Tomogr. 2005;29:725-33.
- [Google Scholar]
- Comparison of accuracy of axial slices versus short-axis slices for measuring ventricular volumes by cardiac magnetic resonance in patients with corrected tetralogy of fallot. Am J Cardiol. 2009;103:1764-9.
- [Google Scholar]
- Cardiovascular function in multi-ethnic study of atherosclerosis: Normal values by age, sex, and ethnicity. AJR Am J Roentgenol. 2006;186(6 Suppl 2):S357-65.
- [Google Scholar]
- Standardized cardiovascular magnetic resonance imaging (CMR) protocols, society for cardiovascular magnetic resonance: Board of trustees task force on standardized protocols. J Cardiovasc Magn Reson. 2008;10:35.
- [Google Scholar]
- Evaluating the systemic right ventricle by CMR: The importance of consistent and reproducible delineation of the cavity. J Cardiovasc Magn Reson. 2008;10:40.
- [Google Scholar]
- Reproducibility of MRI measurements of right ventricular size and function in patients with normal and dilated ventricles. J Magn Reson Imaging. 2008;28:67-73.
- [Google Scholar]
- Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307-10.
- [Google Scholar]
- Right ventricular function in cardiovascular disease, part I: Anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117:1436-48.
- [Google Scholar]
- Assessment of myocardial function: A review of quantification methods and results using tagged MRI. J Cardiovasc Magn Reson. 2005;7:501-16.
- [Google Scholar]
- Three-dimensional systolic kinematics of the right ventricle. Am J Physiol Heart Circ Physiol. 2005;289:H1826-33.
- [Google Scholar]
- Right ventricular function late after total repair of tetralogy of Fallot. Eur Radiol. 2005;15:702-7.
- [Google Scholar]
- Does right ventricular function predict survival in patients with chronic obstructive lung disease? Thorax. 1988;43:621-6.
- [Google Scholar]
- Quantitative assessment of ventricular function using three-dimensional SSFP magnetic resonance angiography. J Magn Reson Imaging. 2007;26:288-95.
- [Google Scholar]
- Evaluation of methods for MR imaging of human right ventricular heart volumes and mass. Acta Radiol. 2002;43:587-92.
- [Google Scholar]
- Operator induced variability in left ventricular measurements with cardiovascular magnetic resonance is improved after training. J Cardiovasc Magn Reson. 2007;9:777-83.
- [Google Scholar]






