Translate this page into:
Viable Intrauterine Pregnancy and Coexisting Molar Pregnancy in a Bicornuate Uterus: A Rare Presentation
Address for correspondence: Dr. Kavitha Krishnamoorthy, 1611 NW 12th Avenue, Miami, FL 33136, USA. E-mail: kavitha.krishnamoort@jhsmiami.org
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A complete hydatidiform mole with a viable coexisting fetus (CMCF) is a rare occurrence. Similarly, Mullerian anomalies such as a bicornuate uterus are uncommon variants of normal anatomy. We report a case of a 40-year-old female with a known bicornuate uterus presenting at 13 weeks gestation with vaginal bleeding. Ultrasound findings showed a healthy viable pregnancy in the right horn with complete molar pregnancy in the left horn. After extensive counseling, the patient desired conservative management, however, was unable to continue due to profuse vaginal bleeding. The patient underwent suction dilation and curettage under general anesthesia and evacuation of the uterine horns. Postoperatively, the patient was followed until serum beta-human chorionic gonadotropin (β-hCG) level dropped to <5 mU. This is the first case of a CMCF reported in a bicornuate uterus, diagnosed with the use of ultrasound imaging.
Keywords
Bicornuate uterus
hydatidiform mole
twin pregnancy
ultrasound

INTRODUCTION
The presence of a complete hydatidiform mole with a viable coexisting fetus (CMCF) is reported to occur in one in 22,000–100,000 pregnancies.[1] Risk factors of a complete hydatidiform mole include extremes of maternal age and previous history of the gestational trophoblastic disease (GTD).[2] Molar pregnancies are associated with potentially life-threatening complications such as heavy vaginal bleeding, preeclampsia, preterm labor, and thyroid abnormalities, making management of these conditions more challenging. Uterine anomalies occur in approximately 0.5–10% of all women and are the result of incomplete Mullerian fusion. Depending on the type of malformation, uterine abnormalities may be associated with several pregnancy complications including recurrent pregnancy loss and preterm labor. We present a unique case of a CMCF in a bicornuate uterus, a rare and unreported occurrence thus far.
CASE REPORT
The patient is a 40-year-old female, gravida 3 para 1011, who presented at 13 weeks 2 days gestation to the emergency department with vaginal bleeding. The patient's past obstetrical history was significant for a prior cesarean section in 2013 and a first-trimester spontaneous loss in 2006. An ultrasound examination performed during the current pregnancy demonstrated a 13 week viable intrauterine pregnancy in the right horn of the bicornuate uterus, and abnormal appearing placental tissue with focal hydropic changes most consistent with a hydatidiform mole present in the left horn [Figure 1]. Laboratory examination demonstrated elevated beta-human chorionic gonadotropin (β-hCG) levels at 480,977 U/L; alpha-fetoprotein was 10.7 IU/ml; hemoglobin and hematocrit were 8.3 g/dL, and 26.2%; thyroid-stimulating hormone was 0.005 mIU/L; free T4 was 2.58 mIU/L; and chest X-ray was clear.
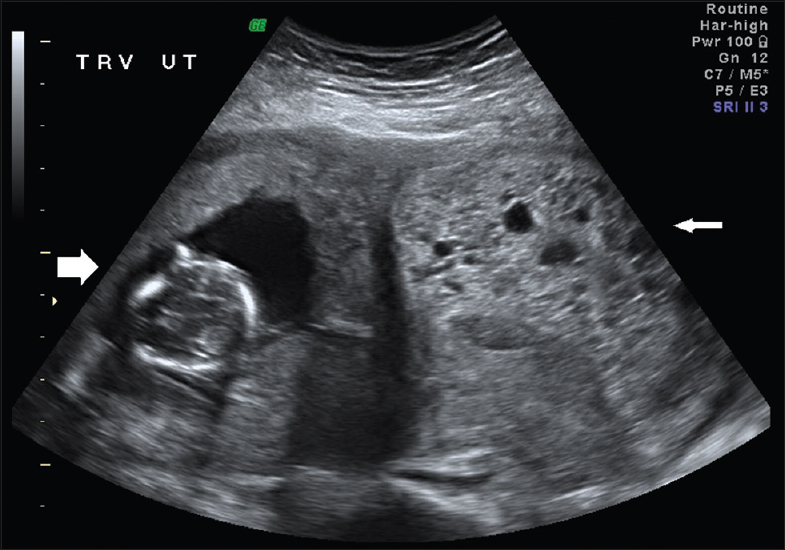
- A 40-year-old female with a known bicornuate uterus and twin pregnancy. Transvaginal ultrasonography demonstrates a transverse cross-sectional view of a bicornuate uterus with a viable intrauterine pregnancy in the right horn (thick arrow on the left of the image) and a molar gestation in the left horn (thin arrow on the right of the image).
The patient was counseled on all management options including expectant versus surgical management, and originally opted for expectant management. However, the patient subsequently had significant vaginal bleeding and thus had to undergo surgical treatment. Using ultrasound guidance, suction dilation and curettage were performed with general anesthesia until all products of conception were removed, and both horns of the uterine cavity were evacuated. The patient received 40 mU of intravenous oxytocin, 0.2 mg of methylergonovine, and 1 unit of packed red blood cells intraoperatively. Her postoperative course was uneventful. Final pathologic diagnosis confirmed a complete hydatidiform molar pregnancy obtained from the left uterine horn. The right horn contained fetal products of conception, and cytogenetic testing confirmed a normal karyotype, 46XX. Paternal karyotyping was unable to be obtained to confirm the paternal origin of the hydatidiform mole. The patient was followed weekly until β-hCG levels returned <5 IU without any cytotoxic therapy. There was no evidence of any persistent trophoblastic disease 1 year later.
DISCUSSION
Approximately, 200 cases of CMCF have been reviewed and cited in the literature.[3] Currently, in patients who desire to continue their pregnancy, the chance of a live birth ranges from 29% to 40%.[34] Sebire et al., noted a 40% live birth rate while studying 77 CMCF pregnancies.[4] Since the coexisting fetus is usually chromosomally normal and potentially viable. Twin pregnancy with a complete hydatidiform mole and a coexisting live fetus is also known as sad fetus syndrome.[5] CMCF pregnancies are complicated by an increased risk of fetal death, maternal vaginal bleeding, hyperemesis gravidarum, preeclampsia, thyrotoxicosis, theca lutein cysts, maternal respiratory distress due to trophoblastic embolization, and persistent GTD (19–30%).[467]
This is the first known case of a normal gestation and molar pregnancy in a bicornuate uterus. All cases reported in the literature of a normal and coexisting molar pregnancy are in single uterine cavities. Molar pregnancies are more likely to have complications including hemorrhage resulting in termination of pregnancy. In this case, it was presumed that since the pregnancies were present in different uterine horns, the outcome may have been better compared to previously reported cases. Unfortunately, this case did not follow through as presumed, and instead, required evacuation of the pregnancy due to the risk of maternal well-being.
Molar pregnancies can differ in presentation depending on the nature of the hydatidiform mole and time of gestation. Complete molar gestations show a central heterogeneous mass with anechoic spaces, described as “snowstorm appearance.” Additional findings of ovarian theca lutein cysts may be present as well. The use of pelvic ultrasonography can detect complete moles 70–90% of the time during the first trimester.[8] On the contrary, partial molar pregnancies can display fetal parts with amniotic fluid and abnormal cystic spaced placenta. The gestational sac may have an increased transverse diameter.[9] Ultrasound, in this case, illustrated the appearance of a typical complete hydatidiform mole [Figure 1].
Congenital uterine anomalies are associated with increased risk of pregnancy loss, malpresentation, premature delivery, and intrauterine growth restriction among others. The degree of poor prognosis depends on the severity of anomaly present. An increased risk of preterm birth is expected with all these patients, with the highest risk noted in females with a unicornuate uterus (50%), followed by those with a bicornuate uterus (39.1%), and then those with didelphys uterus (33.3%) as seen by a study with Fox et al.[10] On the contrary, females with minor uterine anomalies such as arcuate uteri have a low incidence of preterm birth. Diagnosis of Mullerian anomalies has improved with innovations in the gynecological world. The uterine anomaly, in this case, was clearly demonstrated with the use of advanced ultrasonography to display both pregnancies in different horns.
CONCLUSION
To the best of our knowledge, this is the first case of a CMCF reported in a bicornuate uterus. Both pregnancy continuation and elective termination have been documented in the literature, and practice guidelines have not yet been established in regards to the preferred plan of care. What remains crucial is the successful diagnosis of CMCF – more accurately and efficiently accomplished by the use of technological advances in ultrasound imaging. This provides critical information for confirmation of diagnosis and subsequent surgical planning for patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/26/184541
REFERENCES
- Twin pregnancy consisting of a complete hydatidiform mole and co-existent fetus: Report of two cases and review of literature. Gynecol Oncol. 2006;100:218-9.
- [Google Scholar]
- Gestational trophoblastic disease I: Epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol. 2010;203:531-9.
- [Google Scholar]
- Two cases of complete hydatidiform mole and coexistent live fetus. J Prenat Med. 2013;7:1-4.
- [Google Scholar]
- Outcome of twin pregnancies with complete hydatidiform mole and healthy co-twin. Lancet. 2002;359:2165-6.
- [Google Scholar]
- Twin pregnancy with a complete hydatidiform mole and a coexisting live fetus: Rare entity. Sultan Qaboos Univ Med J. 2015;15:e550-3.
- [Google Scholar]
- Management of molar pregnancy and gestational trophoblastic tumors. In: Knapp RC, Berkowitz RS, eds. Gynecologic Oncology (2nd ed). New York: McGraw-Hill; 1992. p. :328-38.
- [Google Scholar]
- Sonographic appearance of first trimester complete hydatidiform moles. Ultrasound Obstet Gynecol. 2000;16:188-91.
- [Google Scholar]
- Sonographic diagnosis of partial hydatidiform mole. Obstet Gynecol. 1989;73(3 Pt 1):414-8.
- [Google Scholar]
- Type of congenital uterine anomaly and adverse pregnancy outcomes. J Matern Fetal Neonatal Med. 2014;27:949-53.
- [Google Scholar]






