Translate this page into:
Unusual Sclerosing Orbital Pseudotumor Infiltrating Orbits and Maxillofacial Regions
Address for correspondence: Dr. Huseyin Toprak, Department of Radiology, School of Medicine, Bezmialem Vakif University, Vatan Street, Aksaray, Istanbul, Turkey. E-mail: huseyin_toprak@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Idiopathic orbital pseudotumor (IOP) is a benign inflammatory condition of the orbit without identifiable local or systemic causes. Bilateral massive orbital involvement and extraorbital extension of the IOP is very rare. We present an unusual case of IOP with bilateral massive orbital infiltration extending into maxillofacial regions and discuss its distinctive magnetic resonance imaging (MRI) features that help to exclude other entities during differential diagnoses.
Keywords
Idiopathic
magnetic resonance imaging
orbital
pseudotumor
INTRODUCTION

Idiopathic orbital pseudotumor (IOP), also known as idiopathic orbital inflammatory syndrome (IOIS), is a nonmalignant orbital inflammation without a known local or systemic cause.[1] It is the most common cause of a painful orbital mass in adults after Graves’ disease.[2] Diagnosis is one of exclusion based on history of the case, clinical examination and clinical course, imaging findings, biopsy, and response to steroid therapy. IOP can affect people of virtually any age, with no sex and race predilection. IOP may present acutely, subacutely, or chronically. It usually presents unilaterally; bilateral presentation is more frequent in children. The disease may be confined to a single orbital structure, but frequently may involve a combination of different structures including the globe, extraocular muscles, retroocular fat tissue, and lachrymal glands. Optic nerves may also be involved. Extraorbital extension of the disease is rare. Clinical presentation may vary according to the specific location and degree of inflammation, fibrosis, and mass effect. Patients may present with proptosis, lid swelling, chemosis, limited motility with tenderness to palpation and pain on movement of the eyes, double vision, light sensitivity, and less commonly, vision loss. An unusual case of IOP with bilateral massive orbital infiltration extending into maxillofacial regions is presented in this report and its distinctive magnetic resonance imaging (MRI) features that help to exclude other differential diagnoses are discussed.
CASE REPORT
A 25-year-old woman presented to our ophthalmology clinic with a long history of progressive protrusion of bilateral eyes and periorbital swelling without vision changes. Her symptoms started when she was 9 years old, but she had no history of treatment or operation because of poor conditions of her country. She denied history of a blow or other injuries to the orbit. She had intermittent attacks of retrobulbar pain and headache. Clinical examination revealed protrusion of both eyes with bilateral conjunctival congestion, restrictive eye movements, and periorbital and facial swelling, more so on the right. Anterior chambers were clear and vision was normal. Routine laboratory and hematologic investigations including T3, T4, and thyroid stimulating hormone (TSH) were normal. Chest X-ray was unremarkable. Doppler ultrasound (USG) showed increased soft-tissue thickness in the periorbital region with arterial and venous flow inside. A vascular malformation was suspected and patient underwent routine and contrast-enhanced orbital MRI [Figure 1]. Exophthalmos and hypertelorism were present. Edematous contrast-enhancing soft-tissue thickening was noted in both orbits as well as in buccal and zygomatic regions. In the orbits, pre- and post-septal structures were extensively affected, sparing the optic nerve dural sheaths and bulbi oculi on both sides. Extraocular muscles were thickened and enhancing brightly. Infiltrative changes were more prominent on the right. Due to multispatial appearances, vascular malformation Graves’ disease was suspected. However, hypointensity seen on T2 image indicated infiltrative changes and ruled out Graves’ disease. Additional diffusion-weighted imaging (DWI) sequences were taken. Diffusion restriction was noted in the massively infiltrated areas. Extensions into paranasal sinuses, middle cranial fossa, and cavernous sinuses were not present. Massive orbital and maxillofacial infiltrating disease with T2 hypointensity, diffusion restriction, and multispatial appearance were suggestive of either lymphoproliferative diseases (orbital pseudotumor, eosinophilic tumor, histiocytic tumor, Langerhans cell tumor, periorbital xantogranulomatous diseases) or sarcoidosis. A biopsy was taken from the left upper eyelid for definitive diagnosis. Histopathologic examination showed a chronic lymphocytic infiltrate consistent with orbital pseudotumor. Patient was treated with oral corticosteroids in tapering dose for 3 months. At the end of treatment, periorbital swelling and redness, and proptosis of eyes resolved to a great extent.
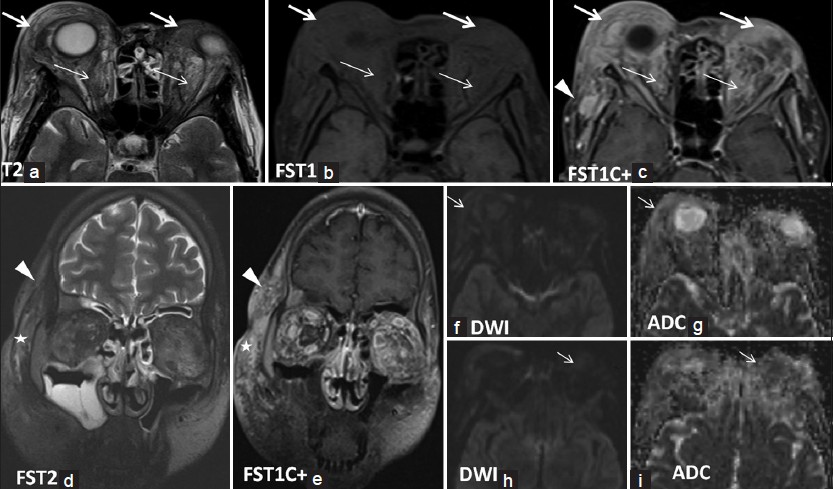
- 25-year-old woman with a long history of progressive bilateral protrusion of eyes, periorbital swelling without vision changes presented with intermittent attacks of retrobulbar pain and headache later diagnosed with idiopathic orbital pseudotumor. (a) Axial T2, (b) axial fat-saturated T1, (c) axial post-contrast fat-saturated T1, (d) coronal fat-saturated T2, and (e) coronal fat-saturated T1-weighted images with (f and g) diffusion-weighted images with corresponding (h and i) apparent diffusion coefficient (ADC) maps demonstrate multispatial massive infiltrative changes including pre-septal (long thick arrows) and post-septal orbital structures (thin arrows) and soft tissue of buccal (asterisks on d and e) and zygomatic regions (arrowheads on c-e). Infiltrated areas are enhancing, T2 hypointense in appearance with restricted diffusion (arrows on f and i), suggestive of either lymphoproliferative diseases or sarcoidosis.
DISCUSSION
IOP is a disease of unknown etiology and is characterized by non-granulomatous inflammation of the orbital soft tissue. It is a type of lymphoproliferative disease. The inflammatory process is generally unilateral and may involve the extraocular muscles, orbital fat, sclera, optic nerve, or lacrimal gland.[3] Extraorbital extension of IOP, though not very common, has been previously reported.[4] IOP can extend via the superior orbital fissure and optic canal into the middle cranial fossa and cavernous sinus, and via the inferior orbital fissure into the infratemporal and pterygopalatine fossa.[5] The most common imaging findings in decreasing order of frequency include infiltration of retroorbital fat, proptosis, extraocular muscle enlargement and enhancement, orbital apex inflammation, and optic nerve thickening.[6] MRI is more valuable in demonstrating soft-tissue changes of IOP because the fibrous and hypercellular nature of the inflammatory mass is reflected by its low signal intensity on T1-weighted (T1W) and T2-weighted (T2W) images.[7] Abnormal soft tissue usually shows intense enhancement on contrast-enhanced T1W images.[8]
Orbital and systemic diseases that mimic IOP include orbital cellulitis, Graves’ disease, sarcoidosis, lymphoma, vascular malformation, metastatic carcinoma, uveal melanoma, and ruptured dermoid cyst. These often can be distinguished based on radiographic characteristics on computed tomography (CT) and MRI, along with clinical examination. In case of extensive orbital infiltration, orbital cellulitis, lymphoproliferative diseases (IOP, eosinophilic tumor, histiocytic tumor, Langerhans cell tumor, periorbital xantogranulomatous diseases), Graves’ disease, and sarcoidosis, vascular malformation should be considered in differential diagnosis. Orbital cellulitis is an infective process associated with pain, fever, and sinusitis, and is usually unilateral. Multispatial appearance favors both vascular malformation and lymphoproliferative diseases, but T2 hyperintensity is typical for vascular malformation. T2 hypointensity and diffusion restriction is more suggestive of lymphoproliferative diseases. IOP can mimic thyroid opthalmopathy; but in IOP, the involvement is less regular and unilateral with involvement of the tendinous insertion of the extraocular muscles.[910] Infiltrative changes in the adjacent fat, periocular involvement, or a discrete mass with thickened muscles favors the diagnosis of IOP. In Graves’ disease, the affected extraocular muscles are T2 hyperintense in contrast to the findings in lymphoproliferative disease. In severe cases of Graves’ disease, retrobulbar and periorbital fatty tissue involvement may be seen. There are no diffusion properties of Graves’ involvement reported in literature. In sarcoidosis, ophthalmologic involvement is frequent, and anterior uveitis, retrobulbar masses, or infiltration of lacrimal gland, extraocular muscles and optic nerve, chiasma, and/or sheath, eyelid swelling, palpable lid masses, and bone destruction can be seen.[9] Infiltrations in sarcoidosis are similar to those of lymphoproliferative diseases with the lesion being isointense on T1W and hypointense on T2W images,[9] but no diffusion restriction is reported in literature.
Our case is unusual in that the clinical course was very long in duration, presentation was bilateral, and there was associated massive involvement of the subcutaneous tissues of the buccal and zygomatic regions on both sides. However, imaging features showing multispatial appearance, T2 hypointensity, and diffusion restriction greatly decreased the possible entities in differential diagnosis.
CONCLUSION
Diagnosis of IOP is one of exclusion because many other conditions may mimic this lesion; thus, it represents a diagnostic challenge for radiologists and clinicians. Complete and detailed medical history, relevant serologic tests, and imaging studies are important to exclude other conditions. IOP should be considered in patients with clinical evidence of persistent, progressive, or recurrent orbital disease and MRI features show multispatial involvement, T2 hypointensity, and diff usion restriction.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/30/133265
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Orbital pseudotumor after an upper respiratory infection: A comprehensive review. Optometry. 2010;81:638-46.
- [Google Scholar]
- Idiopathic orbital inflammatory pseudotumor: Case report and review of the literature. Rom J Morphol Embryol. 2011;52:927-30.
- [Google Scholar]
- Idiopathic orbital inflammation with extensive intra- and extracranial extension presenting as 6th nevre palsy-a case report and literature review. Orbit. 2008;27:458-61.
- [Google Scholar]
- Idiopathic orbital inflammation with extraorbital extension: Case series and review. Eye (Lond). 2006;20:107-13.
- [Google Scholar]
- Idiopathic orbital inflammatory pseudotumor: Case report and review of the literature. Rom J Morphol Embryol. 2011;52:927-30.
- [Google Scholar]
- Pseudotuor of the orbit: Clinical, pathologic, and radiologic evaluation. Radiol Clin North Am. 1999;37:151-68.
- [Google Scholar]
- Systemic Sarcoidosis with Bilateral Orbital Involvement: MR Findings. AJNR Am J Neuroradiol. 1998;19:336-7.
- [Google Scholar]
- MR Imaging of Orbital Inflammatory Pseudotumors with Extraorbital Extension. Korean J Radiol. 2005;6:82-8.
- [Google Scholar]






