Translate this page into:
Unusual causes of gastrointestinal bleeding in the intensive care unit through the radiology lens

*Corresponding author: Oleg Epelbaum, Department of Pulmonary, Critical Care, and Sleep Medicine, Westchester Medical Center, Valhalla, New York, United States. oleg.epelbaum@wmchealth.org
-
Received: ,
Accepted: ,
How to cite this article: Rahmatullah S, Saidman J, Pais S, Maddineni S, Somwaru AS, Epelbaum O. Unusual causes of gastrointestinal bleeding in the intensive care unit through the radiology lens. J Clin Imaging Sci. 2024;14:16. doi: 10.25259/JCIS_96_2023
Abstract
The great majority of patients admitted to the intensive care unit (ICU) for critical gastrointestinal bleeding (GIB) will have a predictable etiology. Once the site is localized to the upper versus the lower gastrointestinal tract, the number of typically encountered etiological possibilities is quite limited. On rare occasions, the cause of GIB requiring ICU care is not one of the standard considerations, potentially leading to diagnostic and therapeutic delays. Within a short time period, three patients were admitted to our institution’s medical ICU each with a different unexpected cause of GIB. All three cases generated a variety of instructive images, which are used in the present series to illustrate these conditions and the role of radiology in their evaluation and management.
Keywords
Gastrointestinal bleeding
Splenic artery
Pseudoaneurysm
Varices
Jejunum
Nonocclusive mesenteric ischemia
INTRODUCTION
Gastrointestinal bleeding (GIB) is a common reason for admission to the intensive care unit (ICU). Upper gastrointestinal (GI) tract hemorrhage is clinically more severe than lower GI tract hemorrhage and, thus, is more prevalent among patients requiring ICU for GIB.[1] In the vast majority of ICU cases, the source of bleeding – if identified – is one of a few predictable possibilities. For upper GIB, the source is almost always either gastroduodenal ulceration or esophageal pathology in the form of inflammation or varices.[1] For lower GIB, the source is likewise almost invariably either diverticulosis or “watershed” ischemia of the colon.[1] In ICU practice, very rarely does GIB arise from an unexpected source. Remarkably, this is exactly what happened in three separate cases encountered in the medical ICU of our institution over a short period of time. In each of these cases, radiology played a pivotal role, generating photogenic images with not only clinical but also educational value. Herein, we describe this three-patient series, relying heavily on the illustrative nature of the accompanying radiological images and highlighting the vital contribution of radiology to the eventual positive outcomes.
CASE SERIES
Case 1
A 57-year-old man with a history of alcohol abuse and prior acute pancreatitis was admitted to the ICU with hematemesis. Multiple esophagogastroduodenoscopies (EGD) demonstrated fresh blood and clots in the stomach without an obvious source. Due to ongoing bleeding, he underwent computed tomography (CT) angiography of the abdomen that revealed an actively bleeding pseudoaneurysm arising from the splenic artery with fistulization to the posterior gastric wall, leading to hemorrhage into the stomach [Figure 1]. Urgent catheter-directed coil embolization of the splenic artery pseudoaneurysm (SAP) was performed, with post-embolization angiography confirming occlusion of the pseudoaneurysm [Figure 2].
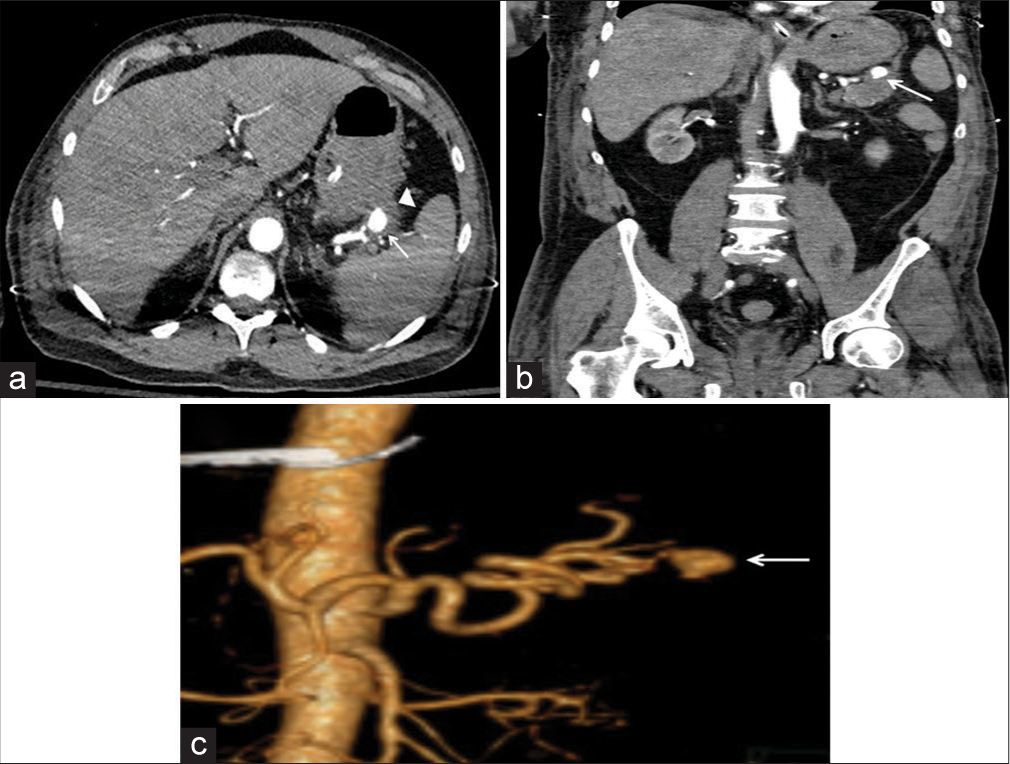
- A 57-year-old man with prior alcoholic pancreatitis presented with hematemesis. (a) Axial image from computed tomography angiography of the abdomen showing a splenic artery pseudoaneurysm (SAP) (white arrow) that fistulized to the posterior wall of the stomach (white arrowhead). (b) Coronal reconstruction from the angiography study in (a) again showing fistulization of the SAP (white arrow) to the stomach. (c) Three-dimensional volume-rendered image from the same angiography study shows to advantage the pseudoaneurysm sac (white arrow) and its relationship to the splenic artery.
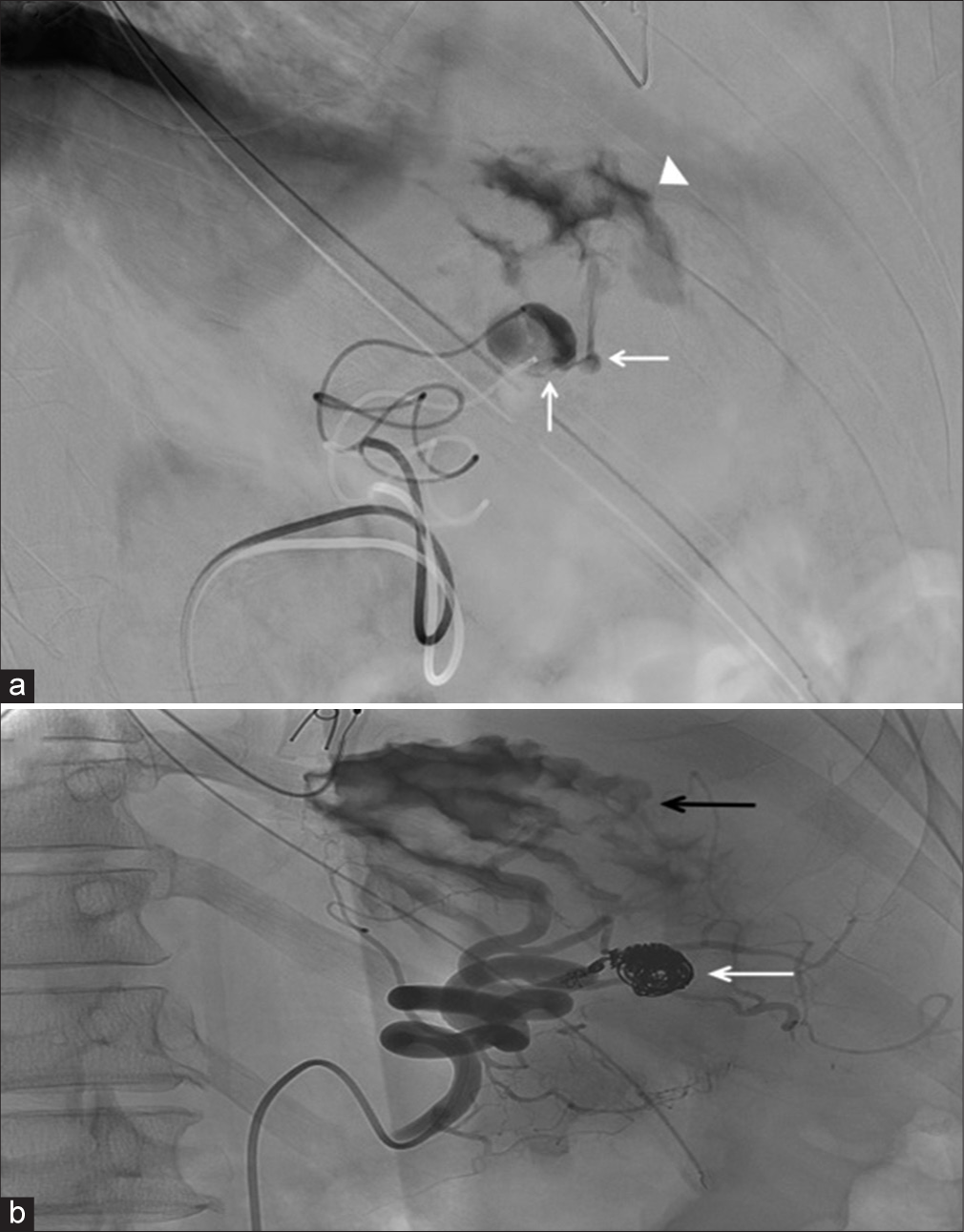
- A 57-year-old man with prior alcoholic pancreatitis presented with hematemesis. (a) Digital subtraction angiographic image from selective splenic arteriography showing a splenic artery pseudoaneurysm (SAP) that is actively bleeding (white arrow) into the stomach and opacifies the gastric rugal folds (white arrowhead). (b) Digital subtraction angiographic image from the SAP coil embolization procedure confirming pseudoaneurysm occlusion (white arrow) on selective splenic arteriography. Contrast from the prior pseudoaneurysm bleeding remains in the stomach and opacifies the gastric rugal folds (black arrow).
Case 2
An 80-year-old man with a history of pancreatic cancer status post-neoadjuvant radiation therapy followed by pancreaticoduodenectomy (Whipple procedure) was transferred to our intensive care unit (ICU) for further evaluation of obscure hematochezia. At the referring hospital, the patient’s evaluation had included EGD, push enteroscopy, colonoscopy, capsule endoscopy, and multiple CT angiograms. All of these failed to disclose the bleeding site. EGD performed at our hospital demonstrated a normal efferent jejunal limb, whereas the afferent limb was filled with blood, and the choledochojejunostomy (CDJ) site was covered by a large clot, which when dislodged revealed underlying varices as the source of bleeding [Figure 3]. The patient was taken to the interventional radiology suite, where catheter-directed super-selective portal venography showed severe stenosis of the superior mesenteric vein (SMV), resulting in pre-hepatic portal hypertension and giving rise to the culprit varices [Figure 4a]. The next procedural step was placement of a transjugular intrahepatic portosystemic shunt (TIPS) followed by coil embolization of the varices. Subsequent portal venography at the conclusion of the same procedure revealed blood flow through the TIPS with occlusion of the embolized varices [Figure 4b].
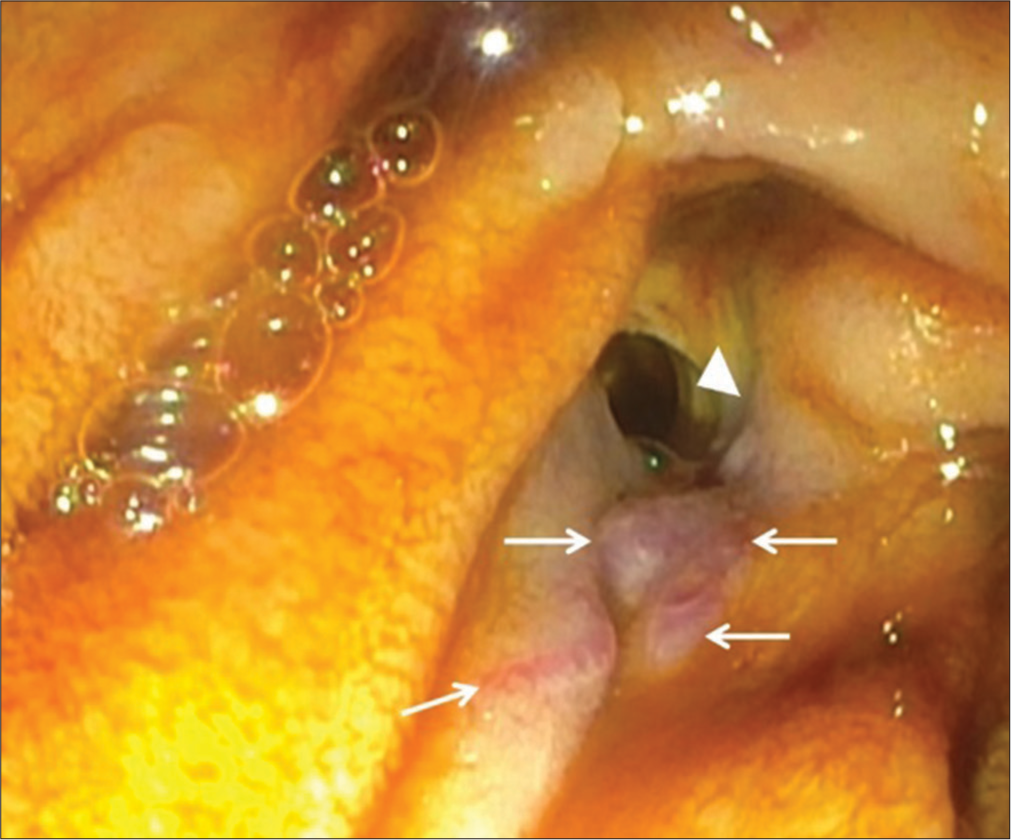
- An 80-year-old man status post Whipple procedure for pancreatic cancer presented with hematochezia. Esophagogastroduodenoscopy image of the afferent limb of the jejunum showing multiple varices (white arrows) at the choledochojejunostomy anastomosis (white arrowhead).
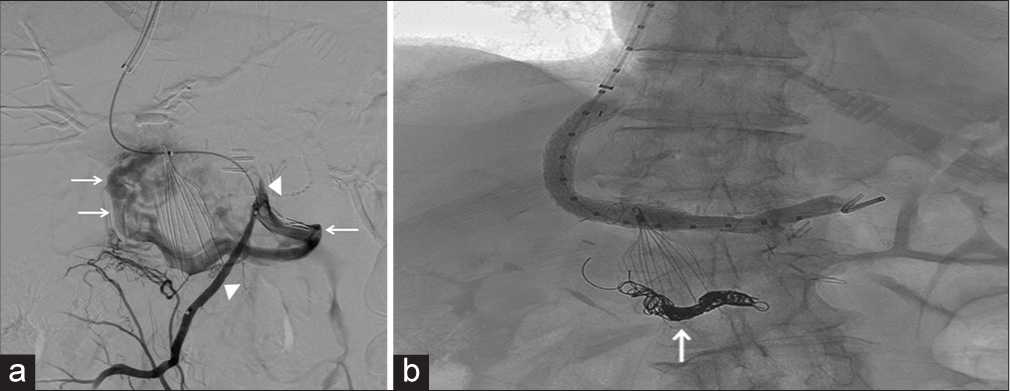
- An 80-year-old man status post Whipple procedure for pancreatic cancer presented with hematochezia. (a) Digital subtraction angiography image from super-selective portal venography showing a stenotic superior mesenteric vein (white arrowheads) that supplies a network of varices (arrows) in the territory of the afferent jejunal limb. (b) Digital subtraction angiography image from repeat portal venography after variceal coil embolization shows blood flow through a previously placed transjugular intrahepatic portosystemic shunt with occlusion of the embolized varices (white arrow).
Case 3
A 76-year-old woman with a history of heart failure with low ejection fraction was admitted to the ICU for acute large-volume hematochezia complicated by syncope that occurred during a long car ride. Her heart failure was being managed with goal-directed medical therapy, which maintained a baseline low systolic blood pressure (SBP) of approximately 80–90 mmHg. She was also taking aspirin 81 mg and ticagrelor due to recent cardiac stenting. She underwent CT angiography of the abdomen with intravenous contrast that showed active bleeding from the ileocolonic branch of the superior mesenteric artery (SMA) in the cecum [Figure 5a and b]. However, subsequent catheter-directed angiography of the SMA showed no active bleeding [Figure 5c]. While the option of provocative mesenteric angiography was available, it was not utilized. The patient then proceeded to colonoscopy that demonstrated a large ischemic ulcer with stigmata of recent, but not active, bleeding in the cecum [Figure 5d].
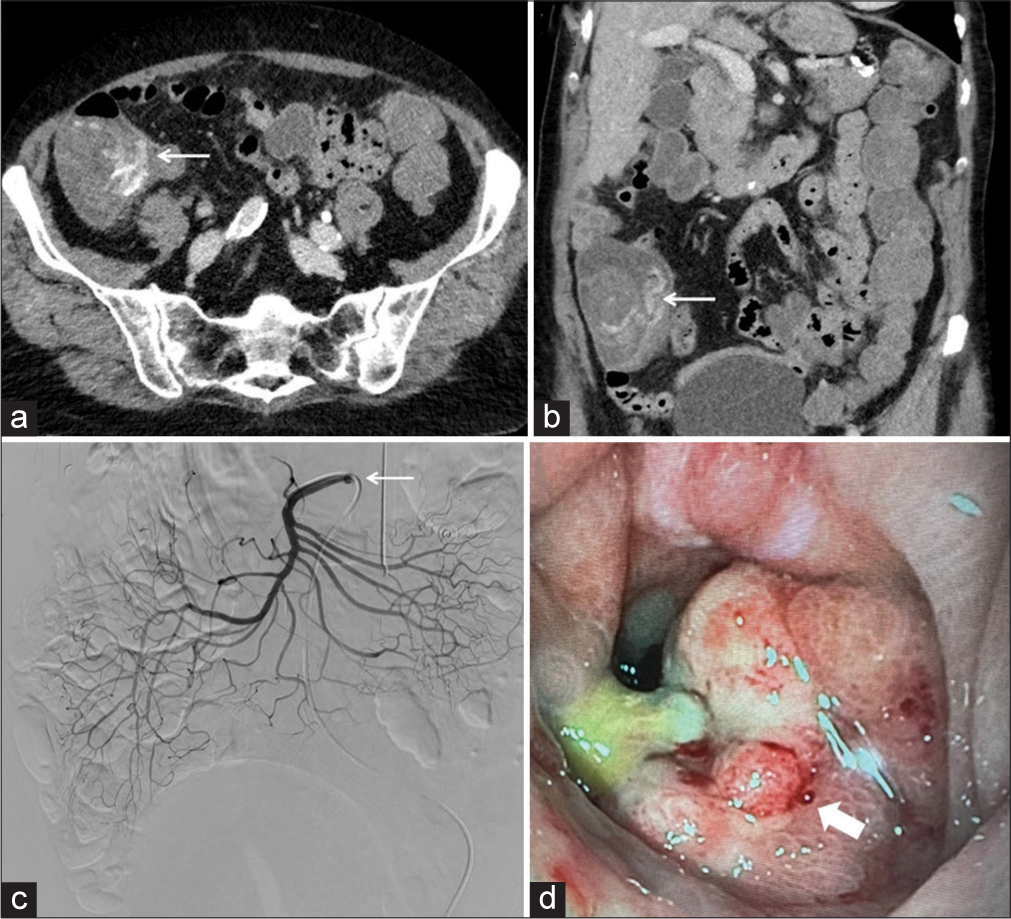
- A 76-year-old woman with congestive heart failure presented with hematochezia. (a) Axial image from computed tomography (CT) angiography shows active bleeding from the ileocolonic branch of the superior mesenteric artery (SMA) in the cecum (white arrow). (b) Coronal reconstruction from the same CT angiography as in (a) depicts the cecal bleeding in a different projection (white arrow). (c) Digital subtraction angiography image from selective arteriography of the SMA (white arrow) shows no active bleeding. (d) Photograph obtained at colonoscopy shows a large ischemic ulcer in the cecum at the site of prior bleeding (white arrow ).
DISCUSSION
Splenic artery pseudoaneurysms (SAPs) are encountered infrequently (10 patients in 18 years at the Mayo Clinic) and are associated with pancreatitis, whether chronic or acute.[2] Although hemorrhage is the most common clinical presentation of SAPs, their relative rarity makes them an unusual etiology of upper GIB. The traditional management strategy has been splenectomy, but coil embolization is a more contemporary and less invasive alternative.[3]
Jejunal varices (an example of so-called ectopic varices) are an uncommon cause of variceal GIB, and variceal bleeding at the site of the CDJ performed as part of the Whipple procedure is particularly noteworthy. In patients with resected pancreatic malignancy, post-operative and radiation-induced changes can lead to stenosis of the portal vein or its tributaries (e.g., SMV) with formation of portosystemic communications in the jejunum as opposed to the much more classical gastroesophageal location, thus evading detection.[4] Management options include sclerotherapy, transjugular intrahepatic portosystemic shunt (TIPS), and transcatheter coil embolization; the latter two interventions were employed in our case.[5]
Non-occlusive mesenteric ischemia (NOMI) occurs in the setting of critically reduced blood flow through patent branches of the mesenteric circulation. Such low splanchnic flow states can be produced by chronic heart failure, hypovolemia, and septic shock. Our patient had a history of heart failure treated to a low SBP and likely developed hypovolemia during her long trip. Hematochezia can complicate resultant bowel ulceration; this complication was promoted in our patient by receipt of dual antiplatelet therapy. If abnormal, catheter-directed angiography offers the option of local vasodilator injection, although that intervention is of uncertain benefit. Otherwise, management is supportive with surgery reserved for cases with necrosis or perforation.[6] In the face of a negative conventional catheter-directed mesenteric angiogram, the proceduralist may elect to pivot to so-called provocative angiography wherein a medication meant to promote bleeding such as heparin or thrombolytics is instilled under controlled conditions in an attempt to induce detectable hemorrhage from the culprit vessel. A recent meta-analysis reported an approximately 50% positivity rate of provocative mesenteric angiography following a negative conventional angiogram.[7] The mortality of NOMI has traditionally been very high, exceeding 70% in most studies.[8]
CONCLUSION
In the vast majority of cases, the cause of GIB in patients admitted to the ICU for this reason will not be a surprise, but there will be occasional memorable encounters with an unexpected source. The above series illustrates three such possible surprises: SAP, jejunal varices, and NOMI. Both diagnostic and interventional radiology have an established role in the evaluation and management, respectively, of these unusual etiologies of critical GIB. Of note, CT angiography was the one tool employed in all three cases of GIB and was diagnostic in two of them, highlighting its versatility and utility in the approach to localizing occult GIB.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- BLEED: A classification tool to predict outcomes in patients with acute upper and lower gastrointestinal hemorrhage. Crit Care Med. 1997;25:1125-32.
- [CrossRef] [PubMed] [Google Scholar]
- Iatrogenic hepatic artery pseudoaneurysms: An uncommon complication after hepatic, biliary, and pancreatic procedures. Ann Vasc Surg. 2003;17:663-9.
- [CrossRef] [PubMed] [Google Scholar]
- Transhepatic portal venous angioplasty with stenting for bleeding jejunal varices. Hepatogastroenterology. 2005;52:749-52.
- [Google Scholar]
- Ectopic variceal bleeding after hepatobiliary surgery: A case report. Medicine (Baltimore). 2021;100:e24975.
- [CrossRef] [PubMed] [Google Scholar]
- Nonocclusive mesenteric ischemia and interventional local vasodilatory therapy: A meta-analysis and systematic review of the literature. J Intensive Care Med. 2020;35:128-39.
- [CrossRef] [PubMed] [Google Scholar]
- Provocative mesenteric angiography for occult gastrointestinal bleeding: A systematic review. CVIR Endovasc. 2023;6:42.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review of survival after acute mesenteric ischaemia according to disease aetiology. Br J Surg. 2004;91:17-27.
- [CrossRef] [PubMed] [Google Scholar]







