Translate this page into:
Traumatic Ectopic Dislocation of Testis
Address for correspondence: Dr. Eranga Perera, Department of Radiology, National Hospital of Sri Lanka, Colombo 10, Sri Lanka. E-mail: wp_eranga@yahoo.co.uk
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Traumatic ectopic dislocation of testis is a rare occurrence and usually occurs following a motorcycle collision, in what is referred to as “fuel tank injury”. Early identification and subsequent surgical management is of utmost importance to maintain normal spermatogenesis in the dislocated testis. In appropriate clinical setting, scrotal ultrasound examination with gray-scale and color flow Doppler imaging is the method of choice for diagnosis. Computed tomography of the abdomen is a useful adjunct procedure. We report a case of traumatic testicular dislocation with partial testicular torsion following a motorcycle collision, diagnosed with imaging, and subsequently confirmed on surgery.
Keywords
Ectopic testis
fuel tank injury
traumatic dislocation of testis
INTRODUCTION

Occurrence of traumatic dislocation of the testis is rare. It occurs as a result of direct external pressure to the perineum dislocating the testis to the surrounding soft tissue (typically the groin).[1] The commonest cause of dislocation is as a result of fuel tank injury following a motorcycle collision. The first case of testicular dislocation was reported secondary to a wagon wheel injury and was published in 1818.[1] Testicular dislocation usually occurs at the time of injury, but a few rare cases have been reported of a late onset of dislocation following injury.[2] Ultrasound examination and computed tomography (CT) may help in the early diagnosis of this condition. Early diagnosis and surgical management is extremely essential to preserve the testis.
CASE REPORT
A 30-year-old male presented to the Emergency Department following a motorcycle collision. Patient complained of a lump in the left inguinal region and on physical examination, the left testis was not palpable within the scrotal sac. A laceration was identified on the right side of the perineum. No pelvic fractures were identified. Ultrasound was performed for further evaluation of the scrotum and inguinal region [Figure 1]. The evaluation revealed that the left testis was located within the inguinal canal, it was normal in size with normal echotexture and no focal lesions. Right testis was in normal position within the scrotal sac, but showed a heterogeneous echotexture that was thought to be due to contusions arising from the trauma [Figure 2]. Spectral Doppler examination of the left testis demonstrated decreased amplitude of systolic upstroke and absence of diastolic flow, suggesting partial testicular torsion [Figure 3].[3] Follow-up CT scan to exclude any solid organ injury within the abdomen and pelvis demonstrated the left testis in the inguinal canal. The right testis was present within the scrotal sac [Figures 4 and 5]. Reconstructed volume rendered image confirms that the superficially palpable lump in the left inguinal region corresponds to the left dislocated testis [Figure 6]. Surgical exploration of the left inguinal canal confirmed the dislocation of the left testis along with a thickened spermatic cord that was looped on itself. Repositioning of the dislocated left testis into the scrotum and orchidopexy was performed.
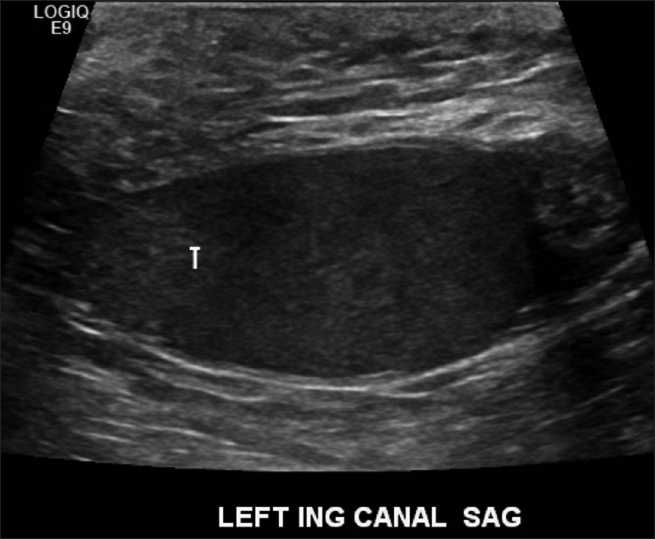
- Gray-scale ultrasound of left inguinal region demonstrates the superior and lateral dislocation of the left testis (T) secondary to scrotal trauma.
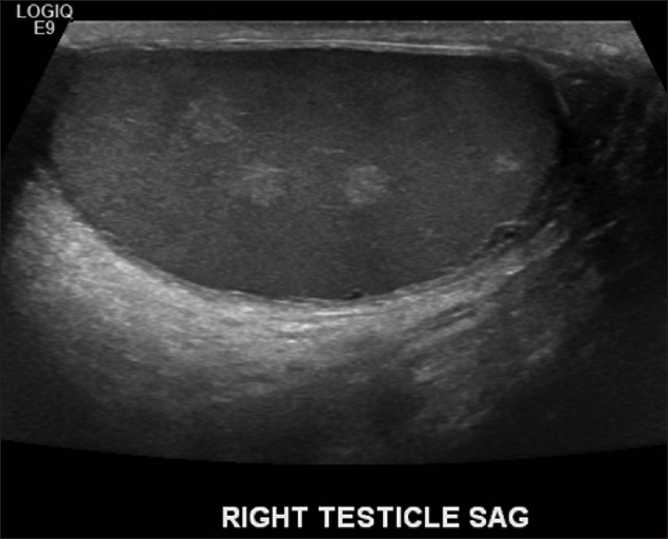
- Gray-scale ultrasound of the right testis. Multiple ill-defined hyperechoic lesions within the parenchyma, representing likely contusions. They resolved on follow-up examination.
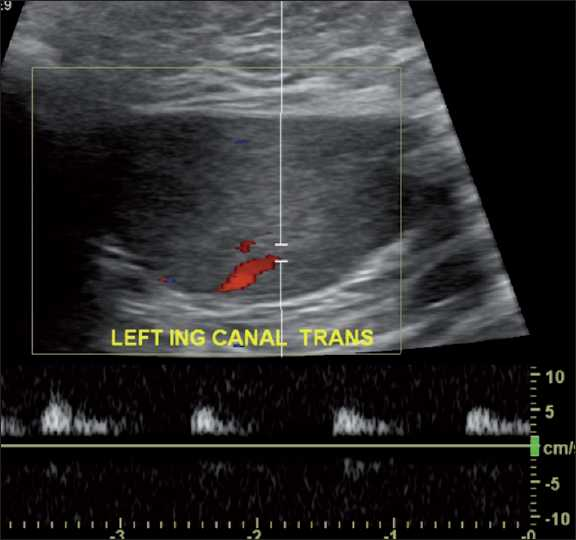
- Spectral Doppler evaluation of the left testis demonstrates a low amplitude waveform with absent diastolic flow suggestive of a partial testicular torsion.

- Contrast enhanced CT scan of pelvis. Axial section at the level of inguinal canal, demonstrates the dislocated left testis (arrow) and small amount of subcutaneous emphysema (arrow head).
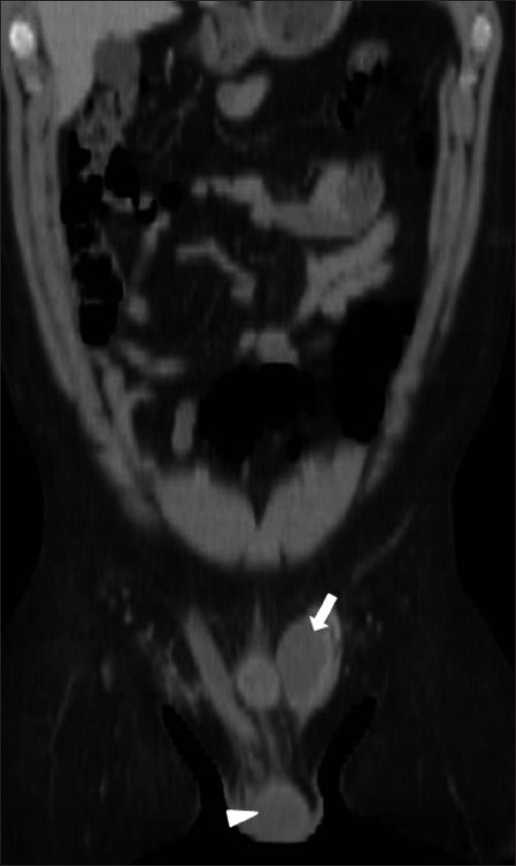
- Coronal reformatted CT image confirms the dislocated left testis (arrow) and the normal position of the right testis within the scrotal sac (arrow head).
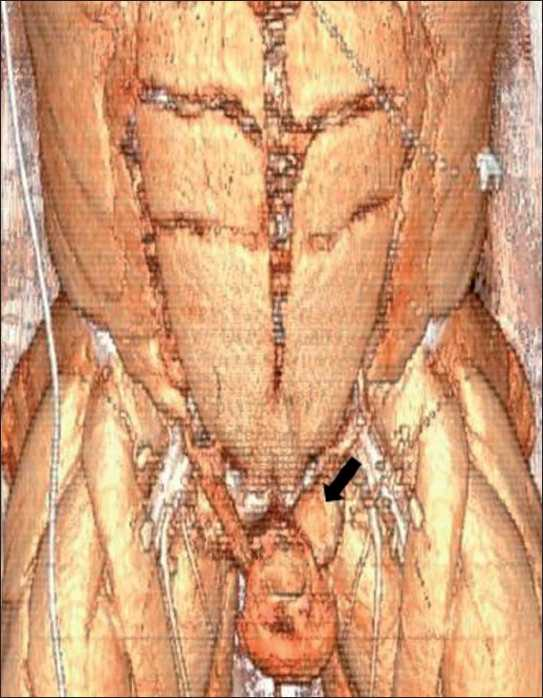
- Surface rendered 3-dimensional CT reformatted image further confirms the presence of dislocated left testis in the inguinal region (arrow).
DISCUSSION
Testicular dislocation is a rare complication of testicular trauma and is defined as displacement of one or both normally located testes out of the scrotum.[4] It was first described by Herbst and Polkey in 1936.[5]
Testicular dislocation commonly occurs following motorcycle collision due to the impact of the fuel tank on the perineum and the scrotum displacing the testis in a superior and lateral direction. These types of injuries are also referred to as “fuel tank injuries”.[56] Patients usually present with a painful palpable mass either in the inguinal region, prepubic area, or crural location.[5]
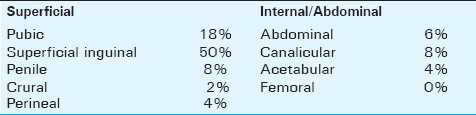
Superficial inguinal pouch is the commonest reported location for a dislocated testis and occurs in 40-50% of the cases.[1] Testicular dislocation can be categorized into two types.[16] In Type 1, the testis is displaced to the inguinal canal or the abdominal cavity through the external /internal inguinal ring. In Type 2, the dislocated testis is located superficially in the subcutaneous regions such as the inguinal, pubic, crural, penile, or acetabular regions.[5] A “Compound dislocation” of the testis is a special category in which traumatic extrusion of the testis occurs through the skin of the scrotum. It is an extremely rare occurrence and was first described by Alyea in 1929.[7] Possible locations of dislocated testis and their reported frequencies are listed in Table 1.[2]
Most dislocations occur immediately after trauma, although some may develop days or even weeks later. The dislocation of the testis is commonly unilateral but can be bilateral as seen in about 30% of the cases.[25] Factors that lead to the dislocation of testis are identified as a spasm of the cremasteric muscle, a wide external inguinal ring, presence of indirect inguinal hernia, and atrophic testis.[5] Dislocation of testis can also be associated with torsion of the spermatic cord and other severe injuries such as multiple bone fractures.[48]
Dislocation of testis has been reported to impair spermatogenesis in post-pubertal men. The histologic changes usually appear after four months of dislocation. They include hyalinization and atrophy of seminiferous tubules, absence of sperm or spermatid formation, presence of germ cells, and an increase in alternative germ cells.[4] However, Hayami et al., reported a case of improving spermatogenesis following orchiopexy performed in a patient four months after traumatic dislocation of the testis.[9] Sakamoto et al., reported a case of recovering spermatogenesis in a patient with bilateral testicular dislocation and azoospermia after 15 years.[4]
Ultrasonography is the first method of choice in evaluating a patient with testicular trauma.[5] In our patient, the dislocated testis is seen in the inguinal region and pubic region with an empty scrotal sac. The scrotal sac is well developed in traumatic dislocation of the testis when compared to cryptorchidism where it is underdeveloped (Broakman's sign).[6] Also, the dislocated testis is typically normal in size unlike the atrophy expected in a cryptorchid testis. Color Doppler imaging can help in assessing the viability of the testis. Scrotal hematoma and hematocele are some of the commonly associated injuries which are present with dislocation of testis.[5]
Multiplanar reformatted images of CT scans are helpful in diagnosing testicular dislocation and are better in demonstrating the relationship of testis, scrotum, and inguinal region. Early diagnosis and treatment are necessary to prevent complications. In rare cases, the dislocated testis can descend spontaneously. Manual reduction is reported to be successful in only 15% of the cases because of the small size defect in the spermatic cord layers and the edema following trauma. Surgical treatment includes groin exploration, open reduction, and orchidopexy to prevent any possible future torsion.[110]
CONCLUSION
Traumatic dislocation of the testis with partial testicular torsion is a rare occurrence, commonly seen after motor cycle injuries. Absence of the testis in the scrotal sac should raise a suspicion of a dislocated testis, and an attempt should be made to locate the dislocated testis by ultrasound examination. Commonest site of dislocation is the inguinal canal. Early surgical management with reduction and orchiopexy is essential to reposition the testis and preserve the spermatogenesis.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp? 2011/1/17/77124
REFERENCES
- Dislocation of the testis as a delayed presentation of scrotal trauma. Urology. 1994;43:743-5.
- [Google Scholar]
- Role of spectral Doppler sonography in the evaluation of partial testicular torsion. J Ultrasound Med. 2008;27:1629-38.
- [Google Scholar]
- Traumatic bilateral testicular dislocation: A recovery of spermatogenesis by orchiopexy 15 years after the onset. Fertil Steril. 2008;90:e9-11.
- [Google Scholar]
- False diagnosis of ruptured testes in a case of traumatic dislocation. JUM. 2009;28:549-53.
- [Google Scholar]
- A two- rider motorcycle accident involving injuries around groin area in both the driver and the passenger. Legal Med. 2007;9:274-7.
- [Google Scholar]
- Pelvic and scrotal trauma: CT and triage of patients. Abdom Imaging. 2009;34:541-4.
- [Google Scholar]
- Traumatic dislocation of the testis: A rare sequel of perineal injury. Emerg Med J. 2003;20:566-7.
- [Google Scholar]






