Translate this page into:
Thermographic Assessment of a Vascular Malformation of the Hand: A New Imaging Modality
Address for correspondence: Dr. Joseph T. Hardwicke, Birmingham Hand Centre, University Hospitals of Birmingham NHS Foundation Trust, Mindelsohn Way, Edgbaston, Birmingham B15 2WB, UK. E-mail: j.hardwicke@bham.ac.uk
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Vascular malformations of the hand are rare. Angiography is the current Gold Standard imaging modality. Thermal imaging is an emerging noninvasive, noncontact technology that does not require intravenous contrast agents. We present the case of a patient with an arteriovenous malformation affecting the hand in which thermal imaging has been used as an adjunct to capture baseline images to allow monitoring of progression. We suggest that thermal imaging provides an adjunct that can be used in addition to clinical examination and/or angiography for the diagnosis and routine follow-up of conservatively managed arteriovenous malformations, to monitor progression or vascular steal, and also for recording recurrence after surgical excision for which there is known to be a significant incidence. With the benefit of being a noninvasive imaging modality that does not require intravenous contrast, or ionizing radiation exposure, office-based thermal imaging may become commonplace.
Keywords
Diagnosis
imaging
monitoring
thermal imaging
thermography
vascular anomaly
vascular malformation
INTRODUCTION

Vascular malformations (VMs) of the hand are rare and can have a variable clinical progression.[1] Such lesions may expand with the growth of the patient or progressive ectasia, but they do not proliferate. Similarly, they do not undergo spontaneous resolution.[2] They can be classified as simple (capillary, lymphatic, venous, or arteriovenous), combined (defined as two or more VMs found in one lesion), or in association with other anomalies.[3] Arteriovenous malformations (AVMs), including arteriovenous fistulas (AVFs), can present as congenital vascular lesions arising from errors in embryonic vasculogenesis[4] or acquired in life secondary to trauma.[5] AVMs are characterized by high-velocity turbulent blood flow from an artery to a vein, bypassing a normal capillary bed and can be clinically staged according to Shobinger.[6] High-flow AVMs of the upper limb can be classified as Type A: Anomalies with either single or multiple AVFs, aneurysms, or ectasias of the arterial side of the circulation; Type B: Anomalies with micro- or macro-fistulas that were localized to a single axial artery of the limb, hand, or digit; Type C: Diffuse arteriovenous anomalies with macro- and micro-fistulous connections involving all tissues of the limb.[1]
Angiography is the current Gold Standard imaging modality and in majority of AVMs displays a central core, or nidus, of abnormal connections from enlarged feeding arteries to draining veins. Angiography is also important for planning of treatment interventions. Conservative treatment, primarily compression, is suggested for asymptomatic AVMs. Surgical or endovascular treatment can be complex with risk of uncontrollable bleeding, incomplete resection, and recurrence including rapid collateralization of adjacent arteries. This may be complicated by skin necrosis leading to amputation and associated loss of function.
Thermal imaging is a non-invasive, non-contact technology that does not require intravenous contrast agents. It has been used experimentally in various areas of plastic surgery including free-flap monitoring, perforator and perforasome mapping,[7] and burn depth assessment.[8] The infrared radiation that is emitted is a surrogate measure of blood flow and can be objectively quantified. The majority of thermal imaging cameras measure infrared radiation in the 1–15 μm range, with most clinical applications focusing on the long-wave infrared from 7 to 14 μm. Recent smartphone-based systems have brought low-cost thermal imaging to the clinic as high-resolution industrial systems may be cost-prohibitive.[9]
We present the case of a patient with an AVM affecting the hand in which thermal imaging has been used as an adjunct to capture baseline images to allow monitoring of progression.
CASE REPORT
A 39-year-old female was referred to our regional Peripheral Vascular Anomalies Clinic with a 24-year history of a lesion affecting the left nondominant hand which started as a pea size mass, progressing to involve the palm, digits, and forearm. She underwent a surgical debulking procedure at the age of 17, but the lesion continued to expand. Schooling and work were unaffected till the age of 21; however, due to pain, weakness, and coordination difficulties, she was not able to return to employment.
On examination, an extensive vascular anomaly was noted to involve the palm, index and middle fingers, and distal forearm and wrist [Figure 1a], with bruit and a palpable thrill. The tips of the thumb and ring and little fingers were cool. An ultrasound Doppler scan and magnetic resonance angiography confirmed the diagnosis of a high-flow AVM, and digital subtraction angiography was used to define the anatomy of the malformation and shows features of a Type-A AVM [Figure 1b]. Nerve conduction studies showed no evidence of compression neuropathy but some axonal loss, presumably due to mild ischemic changes secondary to the AVM.
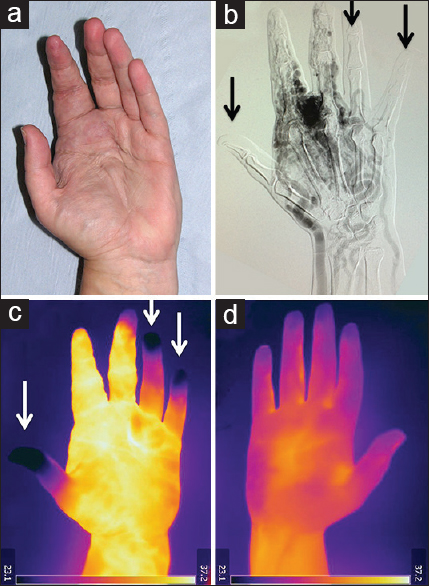
- 39-year-old female with a 24-year history of a lesion affecting the left nondominant hand diagnosed as a congenital arteriovenous malformation of the left hand and wrist. (a) Photograph of the hand shows the arteriovenous malformation visibly involves the radial aspect of the palm and index finger and (b) digital subtraction angiography confirms a Type-A arteriovenous malformation of the radial artery, palmar arch, and digital arteries of the index and middle fingers. There is minimal contrast agent seen in the thumb, ring or little finger digital arteries (black arrow). (c) Thermal image of the arteriovenous malformation shows distal vascular “steal” affecting the thumb, ring and little fingers (white arrows), and (d) thermal image of the unaffected right hand for comparison.
To monitor the “steal” phenomenon affecting the thumb and ulnar-sided digits, a thermal image was recorded in the clinic using an FLIR SC660 thermal imaging camera (FLIR Systems Inc., Wilsonville, Oregon, USA). Images were recorded at 22°C and 50% relative humidity at a distance of 70 cm after exposure of the hand for 3 min to allow surface cooling of the skin. Baseline images of the affected [Figure 1c] and unaffected hand [Figure 1d] were recorded for future monitoring of the AVM with regards to progression of the lesion or of the steal phenomenon. To date, the patient has declined any radiological or surgical intervention to date and is managed with a compression garment and simple analgesia for pain relief.
DISCUSSION
AVMs of the hand are more likely to cause functional impairment than those at other sites, and surgical and/or embolization may have catastrophic consequences to the digits. A comprehensive review by Upton et al., noted that only 12% of the upper limb VMs were AVMs (4 Type A, 15 Type B, and 14 Type C).[1] Although AVMs are rare, they exhibit more aggressive and unpredictable clinical behavior than other forms of VMs. The fast turbulent flow created between the directly connected arterial and venous systems is responsible for a destructive hemodynamic effect that determines clinical symptoms and potentially high recurrence rates. Complete surgical excision in conjunction with embolization sometimes may be impossible without threatening the viability of the digits, and limited debulking may lead to recurrence.
AVMs can be located in various anatomic areas and sometimes occur simultaneously in several regions. In a study by Vaišnyte et al., extracranial AVMs were analyzed, of which 80.4% were located in the extremities and the gluteal region,[10] allowing easy access for thermal imaging. At present, progression of AVMs is monitored clinically with impairment of function or pain determining the management. There is no non-invasive objective test that can determine the evolution or expansion of the lesion, or associated distal vascular steal that may occur in the extremities. Although Upton et al., included distal vascular steal in the Type-C AVM classification,[1] we have shown that this may still occur in Type A lesions and could lead to symptoms requiring surgical intervention. Although no skin or trophic changes have been noted in the reported case, a combination of angiography and thermal imaging has indicated the presence of markedly reduced distal perfusion, which may be subclinical at present. The natural history of AVMs of the hand can be variable, and thermal imaging provides an objective measure of progression that can determine the optimum time for surgery and/or embolization, balancing the risk of iatrogenic digital ischemia versus inherent vascular steal.
CONCLUSIONs
We suggest that thermal imaging is an adjunct that can be used in addition to clinical examination and/or angiography for the diagnosis and follow-up of arteriovenous malformations, to monitor progression or vascular steal, and also for recording recurrence after surgical excision. With the advantage of being a non-invasive imaging modality that does not require intravenous contrast, or ionizing radiation exposure, office-based thermal imaging may become commonplace.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/9/179414
REFERENCES
- Vascular malformations of the upper limb: A review of 270 patients. J Hand Surg Am. 1999;24:1019-35.
- [Google Scholar]
- Vascular anomalies classification: Recommendations from the international society for the study of vascular anomalies. Pediatrics. 2015;136:e203-14.
- [Google Scholar]
- Current knowledge and management of vascular anomalies, II: Malformations. Arch Facial Plast Surg. 2011;13:425-33.
- [Google Scholar]
- Iatrogenic arteriovenous fistula in the hand: A case report. J Plast Reconstr Aesthet Surg. 2012;65:e351-3.
- [Google Scholar]
- Proceedings of International Society for the Study of Vascular Anomalies Congress, Rome, Italy; 23-26 June 1996
- Detection of perforators using thermal imaging. Plast Reconstr Surg. 2013;132:1603-10.
- [Google Scholar]
- A pilot evaluation study of high resolution digital thermal imaging in the assessment of burn depth. Burns. 2013;39:76-81.
- [Google Scholar]
- Detection of perforators using smartphone thermal imaging. Plast Reconstr Surg. 2016;137:39-41.
- [Google Scholar]
- Diagnostic methods, treatment modalities, and follow-up of extracranial arteriovenous malformations. Medicina (Kaunas). 2012;48:388-98.
- [Google Scholar]






