Translate this page into:
Temporal and Pontine Involvement in a Case of Herpes Simplex Encephalitis, Presenting as Kluver Bucy Syndrome - A Case Report
Address for correspondence: Dr. Suresh Thirunavukarasu, Department of Neurology, Indira Gandhi Government General Hospital and Post Graduate Institute, Puducherry, India. E-mail: sureshy2001@rediffmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Bilateral temporal and frontal lobe involvement is a common characteristic of herpes simplex encephalitis (HSE). Clinical sequelae of herpes simplex encephalitis may manifest sometimes as Kluver Bucy syndrome (KBS). In herpes simplex encephalitis, apart from frontal lobe, extra temporal involvement is rare and uncommon. We report a case of HSE manifesting clinically as KBS with a rare radiological finding of temporal and extratemporal involvement of pons.
Keywords
Extratemporal
herpes simplex encephalitis
kluver bucy syndrome
magnetic resonance
INTRODUCTION

Herpes simplex encephalitis (HSE) is the most common fatal non-endemic and sporadically occurring viral encephalitis. In the western population, the annual incidence is approximately 1-2 per million, and contributes to 20% of all encephalitis.[12] Exact rate of incidence in India is not known.[3] If not treated early it can be fatal and has significant morbidity. The most important clinical sequelae of herpes simplex encephalitis is Kluver Bucy syndrome (KBS) with symptoms of hyperphagia, hypersexuality, agnosia, hypermetamorphosis, and placidity. Typical magnetic resonance imaging (MRI) findings in HSE include T2 hyperintensive areas in the temporal and frontal lobes. Brain stem involvement is rare and uncommon. Here we report a case of HSE presenting with a clinical sequelae of KBS involving pons and both temporal lobes.
CASE REPORT
A 40-year-old female was brought to the hospital in an unconscious state. Prior to admission she had fever, decreasing sensorium, and seizure activity. On physical examination, she was found to have minimal response to sharp pain. Her eye movement was sluggish and fundus examination was unremarkable. Deep tendon reflexes were brisk and her plantar was extensor bilaterally. The body temperature was 39.6 degrees Centigrade. There were no signs of meningitis. The patient′s complete blood count, liver function, renal profile, human immunodeficiency virus (HIV) and venereal disease research laboratory (VDRL) status were within normal limits.
Electroencephalogram showed bilateral periodic epileptic discharges. Cerebrospinal fluid (CSF) analysis showed high cell count with preponderance of lymphocytes, raised protein level, and normal sugar level. Polymerase chain reaction herpes simplex virus (PCR HSV) type 1 test was positive. Computed tomography (CT) brain was normal. MRI showed bilateral symmetrical T2 hyperintensity in both the temporal lobes and pons, that was not suppressed on fluid attenuated inversion recovery (FLAIR) sequence and showed no diffusion restriction.
On day 2 after admission, her seizures stopped. By day 5, she started to respond. However, she started to display certain abnormal behavioural patterns. At times she remained placid, sometimes she cried, and at other times she became physically violent. Then she would hit and bite people. She would chew her nails and at times even chew the bed sheets. By day 10, she was ambulant but the abnormal behaviour continued. Based on imaging and patient′s clinical behaviour pattern a diagnosis of KBS secondary to herpes simplex encephalitis was made. She was treated with intravenous acyclovir 10 mg per kg and antiepileptic drugs. The patient is currently under follow up.
DISCUSSION
Involvement of pons in herpes simplex encephalitis is uncommon. Few cases have been reported till now in literature. Extra temporal involvement is more common in patients associated with HIV infection.[4] Extratemporal involvement can be seen in upto 20-30% of the cases.[4–6] The most affected extratemporal lesions are seen in the frontal and parietal cortices, the occipital lobe, basal ganglia, and brain stem. In our patient apart from temporal lobe, pons was also involved. Brainstem involvement especially of pons is very rare. Kluver Bucy syndrome is an uncommon clinical sequelae of herpes simplex encephalitis. 252 cases of this syndrome have been reported till now. The syndrome results in hypermetamorphosis, hyperphagia, hypersexuality, visual agnosia, and behavioural disturbances.[3] In our patient the entire spectrum of Kluver Bucy syndrome was present except for hypersexuality. The exact mechanism for KBS, however, is not known, but the postulation is that there is a disruption of the pathway connecting the dorsomedial thalamus with prefrontal cortex.[7] We are presenting this case to highlight this unique clinical and radiological association in a single immunocompetent patient of herpes simplex encephalitis.

- T2 axial MRI shows central pontine hyperintensity with sparing of the periphery.
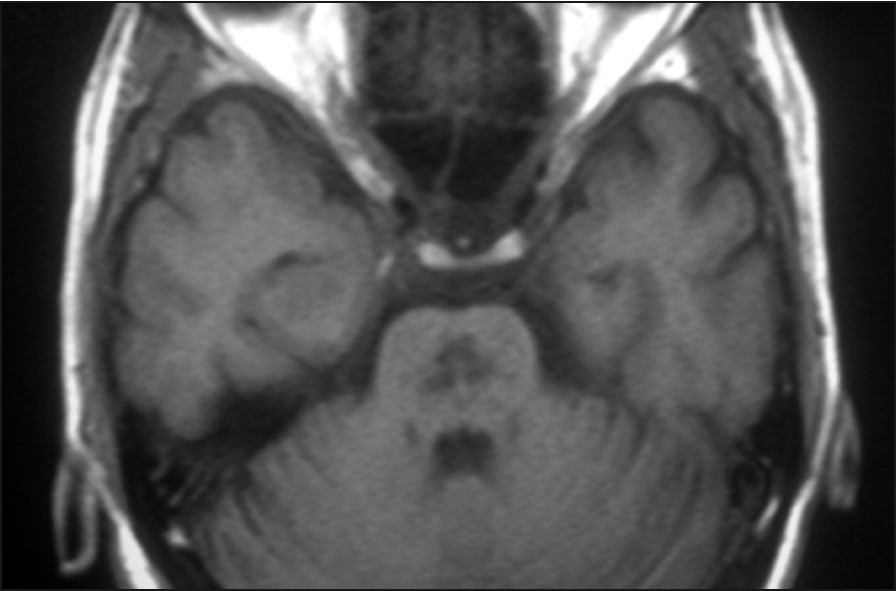
- T1 axial image shows hypointense lesions in the pontine region and at the periphery of the pons. Central pontine myelinolysis is a likely diagnosis, however, involvement of the temporal lobe and clinical features makes central pontine myelinolysis unlikely.
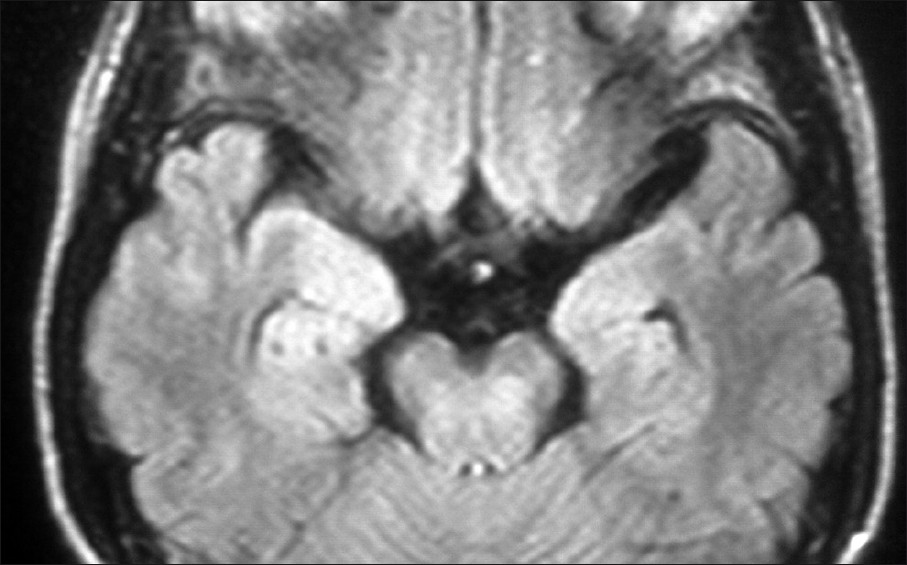
- FLAIR axial MRI image shows bilateral temporal lobe lesions and involvement of the pons. The lesions are hyperintense involving the central pons and anterior part of the temporal lobes. The temporal lobe lesions are symmetrical and bilateral. Bitemporal involvement is characteristic of herpes simplex encephalitis, while basal ganglia and thalamic involvement is characteristic of japanese encephalitis.
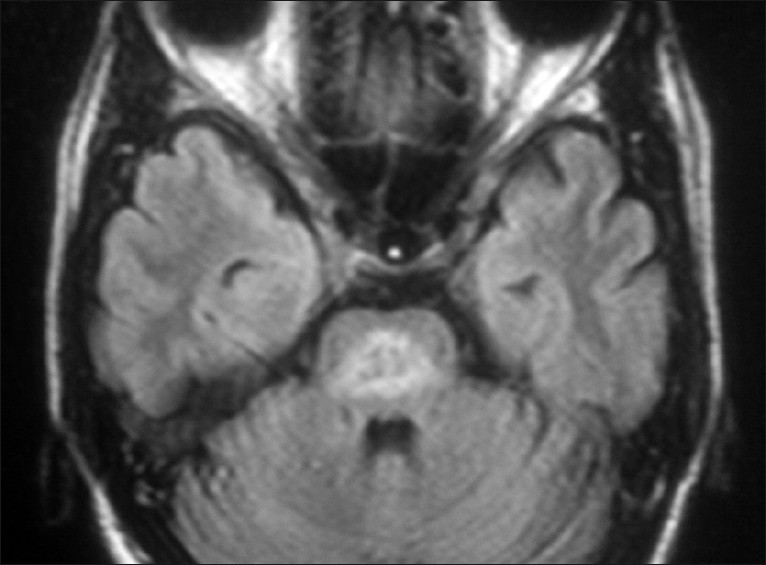
- FLAIR axial MRI image shows well delineated pontine lesions. Pontine lesions and extra temporal involvement in herpes simplex encephalitis is rare.
ACKNOWLEDGMENT
Dr. V. Govindaraju (MD), Medical Superintendent, IGGGH and PGI, Puducherry is gratefully acknowledged.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/43/84318
REFERENCES
- Herpes simplex: encephalitis children and adolescents. Semin Pediatr Infect Dis. 2005;16:17-23.
- [Google Scholar]
- Extra temporal involvement in herpes simplex encephalitis. Eur J Neurol. 2005;12:475-9.
- [Google Scholar]
- Herpes simplex virus infection limited to the brainstem. Wien Klin Wochenschr. 2005;117:495-9.
- [Google Scholar]
- Basal ganglia involvement in a child with herpes simplex encephalitis. Indian J Pediatr. 2009;76:749-50.
- [Google Scholar]
- Kluver-Bucy syndrome after bilateral selective damage of Amygdala and its cortical connections. J Neuropsychiatr Clin Neurosci. 1998;10:354-8.
- [Google Scholar]






