Translate this page into:
Salivary Duct Cyst: Histo-pathologic Correlation
Address for correspondence: Dr. Divya Vinayachandran, Department of Oral Medicine and Radiology, Sri Ramaswamy Memorial Kattankulathur Dental College and Hospitals, Chennai, Tamil Nadu, India. E-mail: drdivyavc@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Non-neoplastic cysts of the salivary glands are uncommon and represent 2-5% of all salivary gland lesions. They are mainly mucoceles or salivary duct cysts. Unlike a mucocele, which is surrounded by granulation tissue, the salivary duct cyst is lined by epithelium. Salivary duct cysts are more common in the oral minor salivary glands and rarely occur in the major salivary glands, show a marked predilection for the superficial lobe of the parotid, and represent 10% of all salivary gland cysts. Neoplastic differentiation of the lining of the salivary duct cyst has been reported. We report a case of a salivary duct cyst of the left parotid gland, with a review of radiographic and histopathologic features.
Keywords
Cyst
histopathology
imaging
parotid gland
INTRODUCTION

Cystic lesions involving the salivary glands are mostly reported to be cystic neoplasms.[1] Few examples include pleomorphic adenoma, warthin's tumor, mucoepidermoid carcinoma, low grade papillary cystadenocarcinoma, and metastatic squamous cell carcinoma.[2] Non-neoplastic cysts are a rarity and comprise 2-5% of all salivary gland lesions. Benign cysts are classified as lymphoepithelial cyst, salivary duct cyst, and dysgenetic cyst.[1] Salivary duct cysts are true cysts that have a congenital or acquired origin. Although literature reveals that most of the cases reported are of acquired origin, duct obstruction often seems to be the cause of the lesion.[3]
CASE REPORT
A 63-year-old male patient, presented with a swelling in front of the left ear that had persisted for 4 months. The swelling initially small had gradually increased in size. No associated symptoms were present. On extra-oral examination [Figure 1], a single, well-defined, localized, oval shaped swelling was present in the left preauricular region, measuring approximately 3 × 4 cm in size. On palpation, it was non-tender, mobile, fluctuant, and soft in consistency anteriorly and firm posteriorly. It was compressible but not reducible. Skin over the swelling was pinchable. A posteroanterior mandibular radiographic image revealed no abnormal findings. Ultrasonography of the left preauricular region [Figure 2] revealed a well-defined anechoic area measuring 3.3 × 1.9 × 3 cm seen in the superficial part of the left parotid gland. Fine needle aspiration yielded a clear straw colored fluid, which had a protein content of 4.6 g/dl. Magnetic resonance imaging (MRI), following aspiration, revealed a well-defined cystic lesion seen in the superficial part of the left parotid gland on T1 and T2 weighted sequences measuring 3.5 × 2.0 × 3.2 cm. [Figure 3]. A hypointense lesion with a focus of hyperintensity within the lesion was seen in T1-weighted image [Figure 4]. A similar focus of hypointensity was seen within the lesion in gradient and T2-weighted images [Figure 3]. This indicated that there was hemorrhage within the lesion, which could have been caused by the aspiration. T2 weighted sequence with fat saturation and short tau inversion recovery (STIR) images revealed an area of high signal intensity within the left parotid gland. The cyst was enucleated under general anesthesia. Histopathological investigation revealed a cyst wall lined with oncocytes [Figure 5]. There were occasional lymphoid follicles and normal salivary gland tissue in the surrounding connective tissue. These features were consistent with the diagnosis of a salivary duct cyst. Patient was reviewed after 6 months and there was no evidence of recurrence [Figure 6].
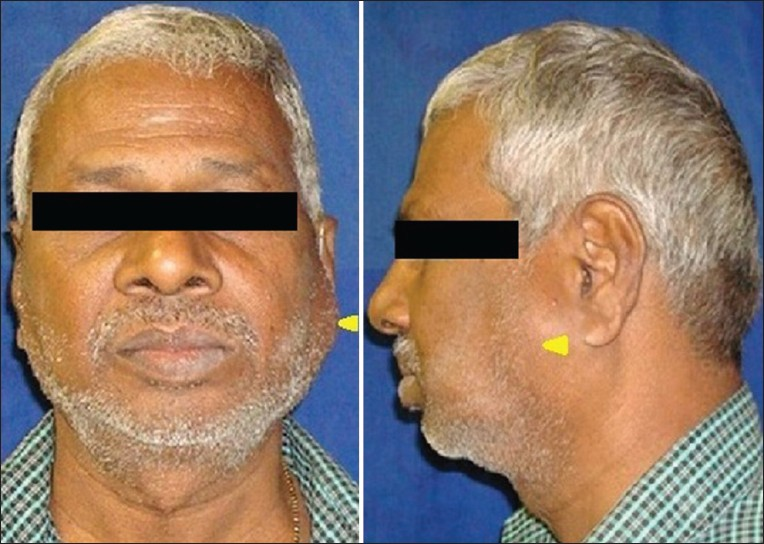
- Extra-oral frontal view of a 63-year-old male patient, shows facial asymmetry, with a single swelling present in the left parotid region (arrowhead). Extra-oral clinical view of the left side of the face, reveals a single, well-defined, oval shaped swelling, approximately 3 × 4 cm in size, present anterior to the ear (arrowhead).

- Ultrasonographic image longitudinal view of the left preauricular region shows a well-defined anechoic area measuring 3.3 × 1.9 × 3 cm seen in the superficial part of the left parotid gland.

- Magnetic resonance imaging: T1-weighted axial image shows a hypointense lesion within the left parotid gland (arrowhead), with a focus of hyperintensity within the lesion.

- Magnetic resonance imaging: T2-weighted axial image, shows a well-defined cystic lesion of high signal intensity, approximately measuring 3.5 × 2.0 × 3.2 cm, present within the left parotid gland (arrowhead). A focus of hypointensity is seen within the lesion.

- Hematoxylin and eosin stained specimen at ×20 view shows the cyst wall with oncocytic metaplasia (arrowhead).

- Postoperative extra-oral clinical view of the left side of the face shows absence of the swelling in the preauricular region (arrowhead).
DISCUSSION
Salivary duct cysts are true cysts and are also referred to as mucus retention cyst, mucus duct cyst, sialocyst, and simple cyst.[13] According to European and American literature, salivary duct cysts constitute 10% of all cysts of the salivary glands.[4] They may be of congenital or acquired origin. However, a vast majority of the cases are acquired and occur following obstruction in the duct.[1] Although the exact causative factor leading to obstruction is often unknown, some suggestions include calculi, mucus plugs, postoperative, or post-inflammatory strictures.[4] Salivary duct cysts most commonly involve the minor salivary glands and those in the floor of the mouth, buccal mucosa, and lip are usually involved.[45] They rarely involve the major salivary glands and when they do, they may be multiple and are often found in the superficial lobe of the parotid. Children to older adults are affected, mostly those over 30-40 years of age.[4] There is no gender predilection. Salivary duct cyst of the parotid gland mostly presents as an asymptomatic, unilateral swelling.[1] The facial nerve is uninvolved and fixation to overlying skin is absent. The cysts range from 0.8 cm to 10 cm in size but majority reach 1-3 cms in size.[4]
Imaging plays an important role in investigation of salivary duct cysts in delineating the borders, extent of involvement, and the content. Ultrasonography reveals a well-defined lesion with imperceptible walls, anechoic center, and posterior acoustic enhancement.[6] There is no internal blood flow on power Doppler or with color Doppler. On computed tomography, cystic lesions appear as well circumscribed, non-enhancing (following contrast administration), and low density areas.[7] They appear as well circumscribed, high signal areas on T2-weighted MRI. No enhancement is seen, following administration of gadolinium contrast, unlike benign mixed tumors. Sialography permits only indirect visualization of the cyst, evaluated by the displacement of the ducts around them.
Histological investigation paves way to the final diagnosis and should be carefully evaluated. These lesions are mostly unilocular, lined by ductal epithelium, which may be cuboidal or columnar, and completely or partly lined by squamous epithelium.[1] Sparse to moderate lymphocytic infiltrations may be observed in the cyst wall. Occasionally, oncocytic metaplasia (often seen in cases following ductal obstruction) is seen.[3] The lesions composed of oncocytic cells range from oncocytic metaplasia, and hyperplasia to benign and malignant neoplasms, including oncocytomas and oncocytic carcinomas.[8] Salivary duct cysts may present with multilocular or papillary appearances.[1]
Salivary gland cysts could be an early manifestation of a salivary gland tumor.[9] Presence of epithelial alterations, such as metaplasias and focal papillary proliferations observed, are comparable to similar changes seen in odontogenic cysts and may be early marker of tumor manifestation. There have been rare instances of development of benign and malignant neoplasms such as adenocarcinoma and mucoepidermoid carcinoma from the lining of a salivary duct cyst.[4] An association of latent Epstein-Barr virus infection with this neoplastic transformation has also been reported.[10]
Surgical excision is curative. Partial or total removal of the gland may be necessary.[3]
CONCLUSION
The inconspicuous clinical presentation and similarities between the epithelial linings of various lesions makes meticulous investigation mandatory. Imaging plays a significant role in diagnosing parotid gland duct cyst and ultrasound should be the first modality in its screening.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/2/3/111236
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- Tumors of the Salivary Glands. In: Rajendran R, ed. Shafer's Textbook of Oral Pathology (5th ed). Amsterdam: Elseiver; 2007. p. :309-56.
- [Google Scholar]
- Oral and Maxillofacial Pathology. (2nd ed). Philadelphia: Saunders; 2002. p. :389-436.
- [Google Scholar]
- Salivary duct cyst: Its frequency in a certain Japanese population group (Tohoku districts), with special reference to adenomatous proliferation of the epithelial lining. J Oral Sci. 2001;43:9-13.
- [Google Scholar]
- Contemporary oral and maxillofacial pathology. (2nd ed). Maryland Heights: Mosby, Elsevier; 2004. p. :335-7.
- [Google Scholar]
- US of the major salivary glands: Anatomy and spatial relationships, pathologic conditions, and pitfalls. Radiographics. 2006;26:745-63.
- [Google Scholar]
- Salivary gland radiology. In: White SC, Pharoah MJ, eds. Oral Radiology, Principles and Interpretation (6th ed). Maryland Heights: Mosby Elseiver; 2009. p. :578-96.
- [Google Scholar]
- Mucoepidermoid carcinoma in a salivary duct cyst of the parotid gland.Contribution to the development of tumours in salivary gland cysts. Pathol Res Pract. 1996;192:1211-7.
- [Google Scholar]






