Translate this page into:
Rationale of Using Dynamic Imaging for Characterization of Suspicious Lung Masses into Benign or Malignant on Contrast Enhanced Multi Detector Computed Tomography
Address for correspondence: Dr. Saurav Bhagat, Department of Radiodiagnosis, Era's Lucknow Medical College and Hospital, Sarfarazgunj, Hardoi Road, Lucknow - 226 003, Uttar Pradesh, India. E-mail: dr.sauravbhagat@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
To assess the utility of dynamic imaging namely, wash-in and wash-out characteristics through multidetector contrast-enhanced computed tomography in differentiating benign and malignant pulmonary masses.
Materials and Methods:
Seventy-three patients who were suspected to have malignant pulmonary mass on the basis of clinical symptoms and chest radiograph were included in the study. All the patients underwent multidetector computed tomography scanning, and three series of images were obtained for each patient-noncontrast, early enhanced, and 15 min delayed enhanced scans. Computed tomography (CT) findings were assessed in terms of washin, absolute, and relative percentage washout of contrast. Biopsy of the mass was done and sent for histopathological evaluation. Sensitivity, specificity, and area under curve for diagnosing malignancy in the lung masses were calculated by considering both the wash-in and wash-out characteristics at dynamic CT and plotting the receiver operating curve after the final diagnosis which was obtained by histopathological evaluation.
Results:
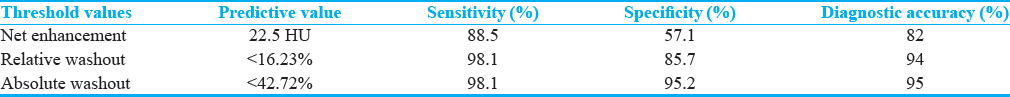
Threshold net enhancement (washin) value of >22.5 HU had sensitivity, specificity, and diagnostic accuracy of 88.5%, 57.1%, and 82%, respectively, in predicting malignancy. Threshold relative percentage washout of <16.235% had 98.1%, 85.7%, and 94% sensitivity, specificity, and diagnostic accuracy, respectively, and threshold absolute percentage washout of <42.72% had 98.1%, 95.2%, and 95% sensitivity, specificity, and diagnostic accuracy, respectively, in predicting malignancy.
Conclusion:
Threshold net enhancement (washin), absolute and relative washout percentages can be used to predict malignancy with very high diagnostic yield, and possibly obviate the need of invasive procedures for diagnosis of bronchogenic carcinoma.
Keywords
Contrast wash-in
contrast wash-out
histopathology
lung mass
multidetector computed tomography

INTRODUCTION
Lung cancer is the leading cause of cancer-related deaths in men and women worldwide. Imaging plays a crucial role in evaluating suspicious pulmonary masses. Computed tomography (CT) constitutes the backbone of imaging of lung cancer and helps in imaging characterization of doubtful lung masses. The diagnosis of benignity or malignancy of suspicious lung lesion has direct implications on drafting treatment. Conventional imaging methods, which primarily focused on the morphologic evaluation of lesions, were inadequate in differentiating benign and malignant lesions.[1]
With the advent of newer techniques such as helical dynamic CT, multidetector row CT using contrast material, more accurate and useful characterization of pulmonary masses can be done by utilizing their hemodynamic differences, as degree of enhancement of malignant lesions is significantly more than benign lesions.[2345]
Earlier studies using dynamic-enhanced multidetector row CT mainly considered the early enhancing phase of the lung lesion, which revealed high sensitivity in diagnosing malignant nodules albeit low specificity.[4]
Recent studies have been done for the imaging characterization of adrenal lesions by assessing the washout properties of the adrenal lesions at delayed contrast-enhanced CT (CECT).[678910] Washout of the contrast material is defined as a decrease in the attenuation of the lesion at delayed CECT after the intravenous administration of contrast.[11]
However, very few authors have studied combined wash-in and wash-out properties at delayed CECT in imaging characterization of malignant and benign pulmonary nodules.[111213] Although these studies evaluate the standard wash in–wash out characteristics, they are only in solitary lung nodules instead of lung masses that we are evaluating in this study. The purpose of the present study was to assess the sensitivity, specificity, and accuracy of a dedicated lung CT protocol using attenuation values at unenhanced CT and CECT in early and delayed phases to study wash-in and wash-out characteristics (by calculating both absolute and relative percentage washout) in the imaging of suspicious pulmonary masses and their correlation with histopathological examination.
MATERIALS AND METHODS
Patient inclusion criteria
Seventy-three patients who were suspected to have malignant pulmonary mass (diameter >3 cm) on the basis of clinical and chest radiographic evaluation were included in the study. Ethical committee clearance was taken for the study protocol and written informed consent was taken from all the patients.
Multidetector computed tomographic scanning
All the patients underwent multidetector CT (MDCT) scanning using 384-slice CT scanner (Siemens SOMATOM Force®). Scanning of the suspicious lesion was first done to obtain thin-section unenhanced CT scan images (2.5 mm collimation, 0.8 s gantry rotation time, 120 kVp, 90 mA), followed by dynamic and delayed enhanced scanning. With the help of a high-pressure injection apparatus (Medrad, Pittsburgh), at a flow rate of 1.8 ml/s, 60–90 ml of a nonionic contrast agent (Ultravist, 370 mg/ml) was injected through the cubital vein. The amount of the contrast agent was calculated based on the body weight (1.5 ml/kg). In each patient, three series of images were obtained – unenhanced noncontrast (from the lung apices through the adrenal glands), early enhanced postcontrast scanning of the entire lung at 15–20 s, and delayed scanning limited to the lung mass only, were done approximately 15 min after the administration of contrast material using similar scanning parameters. After scanning, images were reconstructed into slices 2 mm thick using standard algorithm. All images were then transferred to the workstation for further evaluation, and both mediastinal (window width, 400 HU; window level, 20 HU) and lung (window width, 1500 HU; window level, −700 HU) window images were then viewed.
A circular or ovoid region of interest (ROI) was placed over the lesion on each image of the nonenhanced CT scan and both dynamic and delayed scans. The section with the largest surface area of tissue was selected. Calcified and necrotic regions were not included in the assessment. Then, the mean attenuation value was calculated.
Using the mean Hounsfield unit value in each ROI of the suspicious pulmonary masses on the dynamic and delayed CT scans, following dynamic characteristics of tumor enhancement using wash-in and wash-out values of the contrast were calculated and assessed: peak enhancement, net enhancement (washin), and absolute and relative percentage loss (washout). Peak enhancement was defined as the attenuation value of the mass in the early enhancement phase. Net enhancement was calculated by subtracting the pre-enhancement attenuation value from the peak enhancement attenuation value. Absolute loss of enhancement at delayed imaging was calculated by subtracting the attenuation value at 15 min (HUdelayed) from the peak enhancement attenuation value (HUearly). Absolute percentage loss was calculated using the formulae:[11]
Absolute washout (absolute percentage loss of enhancement) = ([HUEarly − HUdelayed]/[HUEarly − HUnoncontrast]) × 100.
Relative washout (relative loss of enhancement) = ([HUearly – HUdelayed]/HUearly) × 100.
Pathologic evaluation
CT-guided biopsy was performed on MDCT scan (Siemens Somatom force® 384 slice).
Bronchoscopy (Biopsy) was performed by OLYMPUS flexible fiber-optic bronchoscope-TYPE TE2®.
Biopsy samples were kept in formalin and send to the pathology department for the histopathological analysis.
Statistical analysis
Statistical analysis was performed with SPSS Software (Version 15.0, Chicago, IL: SPSS Inc.). The values were compared between malignant and benign pulmonary masses after final diagnosis by histopathological evaluation by the use of Student's t-test. Receiver operating characteristic analysis was performed to determine a threshold for differentiating malignant from benign lesions.
Sensitivity and specificity were calculated by varying the level of enhancement that signified a positive finding (cut-off value).
Diagnostic characteristics – that is sensitivity, specificity, and area under curve – were calculated by considering both the wash-in (net enhancement) and washout (absolute and relative percentage loss of enhancement) characteristics at dynamic CT.
Student's t-test and receiver operating curve analysis were used to analyze statistically significant differences between attenuation values for unenhanced imaging, net enhancement, and absolute and relative loss of enhancement in malignant and benign masses. P < 0.05 was considered statistically significant difference.
RESULTS
Out of 73 patients suspected to have malignant lung mass, 51 were males and 22 were females. Out of 73 lung masses suspicious for malignancy, 52 were proven to be malignant and 21 turned out to be benign on histopathological examination [Table 1]. The mean age for patients with diagnosed malignancy was 56.43 ± 4.07 years and for benign mass was 26.53 ± 10.13 years.
Noncontrast computed tomography
The mean CT attenuation value for benign lesions on noncontrast CT scan was 39.00 ± 3.48 HU (range 33-45). The mean attenuation value in 52 malignant lesions on noncontrast CT scans was 38.98 ± 3.45HU (range 34-46). The mean attenuation value of benign and malignant lesions on nonenhanced CT scans was not significantly different from each other (Student's t-test, P = 0.983).
Early enhanced computed tomography and washin of contrast material
The mean attenuation of benign lesions on early CECT scans was 61.29 ± 6.94 HU (range 52–75) and net enhancement attenuation (washin) was 22.29 ± 7.60 HU (range 7–40). The mean attenuation of the malignant lesions on early enhanced CT scans was 69.94 ± 10.88 HU (range 58–84). Net enhancement attenuation (washin) for malignant lesion was 30.96 ± 5.95 HU (range 20–42). Significant differences were found between benign and malignant lesions with regard to the mean attenuation value (Student's t-test, P < 0.001). Significant differences were found between benign and malignant lesions with regard to the net enhancement attenuation (washin) on early CECT scans.
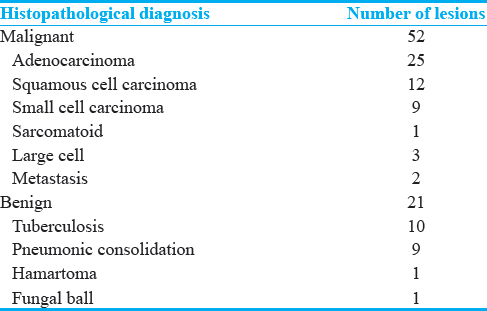
Results of the receiver operating curve analysis [Figure 1] showed that a threshold net enhancement value of 22.5 HU has a sensitivity of 88.5% and specificity of 57.1% to diagnose malignancy on early CECT scans.

- The graph depicting results of the receiver operator characteristic analysis to differentiate between benign and malignant lesions with regard to net enhancement attenuation (wash-in) on contrast-enhanced computed tomography in early phase. The area under curve is 0.827, P < 0.001.
Delayed contrast-enhanced computed tomography with absolute and relative percentage washout of contrast material
On delayed CECT scans, the mean absolute attenuation value for the benign lesions was 44.86 ± 7.51 HU (range 35–70). The mean absolute attenuation value for 52 malignant lesions on delayed CECT scans was 64.58 ± 5.93 HU (range 54–82). The absolute attenuation values of malignant lesions were significantly larger than values of benign lesions on delayed CECT scans (Student's t-test, P < 0.001).
Results of receiver operating curve analysis [Figure 2] showed that a threshold absolute attenuation value of >56.5 HU had 92.3% sensitivity and 90.5% specificity in diagnosing malignancy on delayed CECT scans.
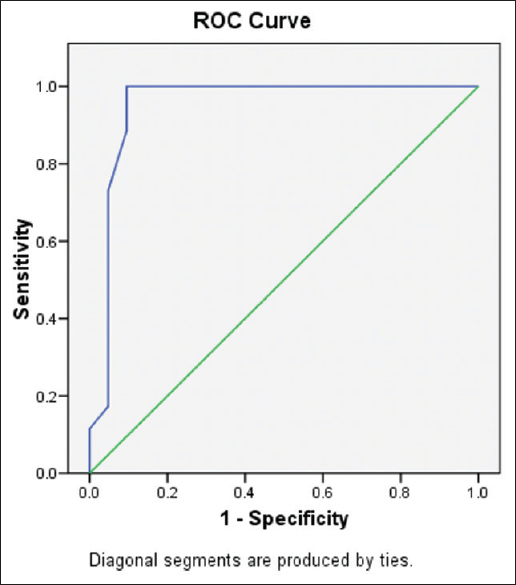
- The graph depicting results of the receiver operator characteristic analysis to differentiate between benign and malignant lesions with regard to absolute attenuation value on contrast-enhanced computed tomography in early phase. The area under curve is 0.950, P < 0.001.
On the MDCT scans, the mean absolute percentage washout value for benign lesions came out to be 75.76 ± 20.69 (range, 7.5–96.15).
The mean absolute percentage washout value for malignant lesions was 17.77 ± 10.51 (range, −4.76–35.45). The range is in negative as the Hounsfield unit of one lesion actually increased on delayed imaging than early enhanced CT.
The absolute percentage washout values of malignant lesions were significantly lower than the values of the benign lesions on delayed CECT scans (Student's t-test, P < 0.001).
The results of receiver operating curve analysis [Figure 3] showed that a threshold absolute percentage washout of <42.72% had 98.1% sensitivity and 95.2% specificity for identifying malignant lesions.
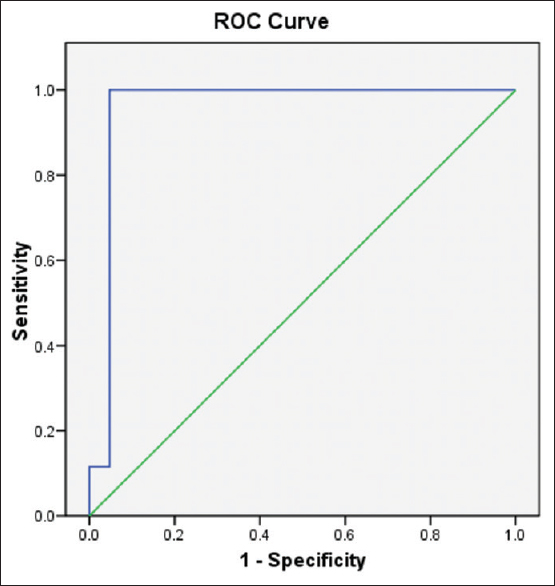
- The graph depicting the results of the receiver operator characteristic analysis for differentiating between malignant and benign pulmonary masses with regard to mean absolute washout at contrast-enhanced computed tomography. The area under curve is 0.958, P < 0.001.
On the MDCT scans, the mean relative percentage washout value for benign lesions came out to be 26.53 ± 10.13 (range, 4.11–44.59).
The mean relative percentage washout value for malignant lesions was 7.61 ± 4.07 (range − 1.67-18.99). The range is in negative as the attenuation value of one lesion actually increased on delayed imaging than early enhanced CT.
The relative percentage washout values of malignant lesions were significantly lower than the values of the benign lesions on delayed CECT scans (Student's t-test, P < 0.001).
The results of receiver operating curve [Figure 4] analysis showed that a threshold relative percentage washout of <16.235% had 98.1% sensitivity and 85.7% specificity for identifying malignant lesions.
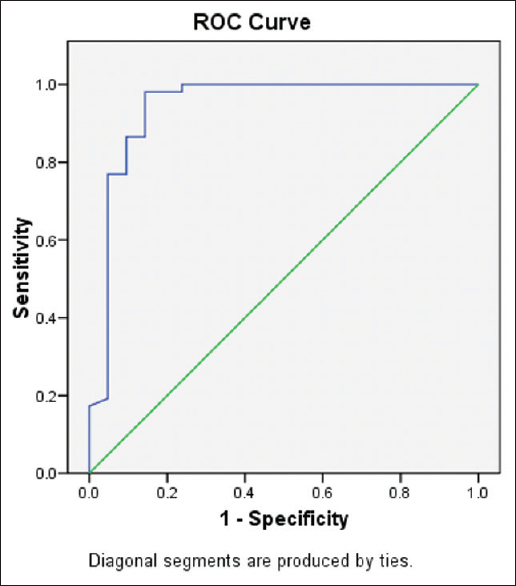
- The graph depicting the results of the receiver operator characteristic analysis for differentiating between malignant and benign pulmonary masses with regard to mean relative washout at contrast-enhanced computed tomography. The area under curve is 0.942, P < 0.001.
The results have been summarized in the following Tables 2 and 3. Two examples have been shown in Figures 5 and 6 which show the radiograph that served as inclusion criteria along with their MDCT and histopathological evaluation.

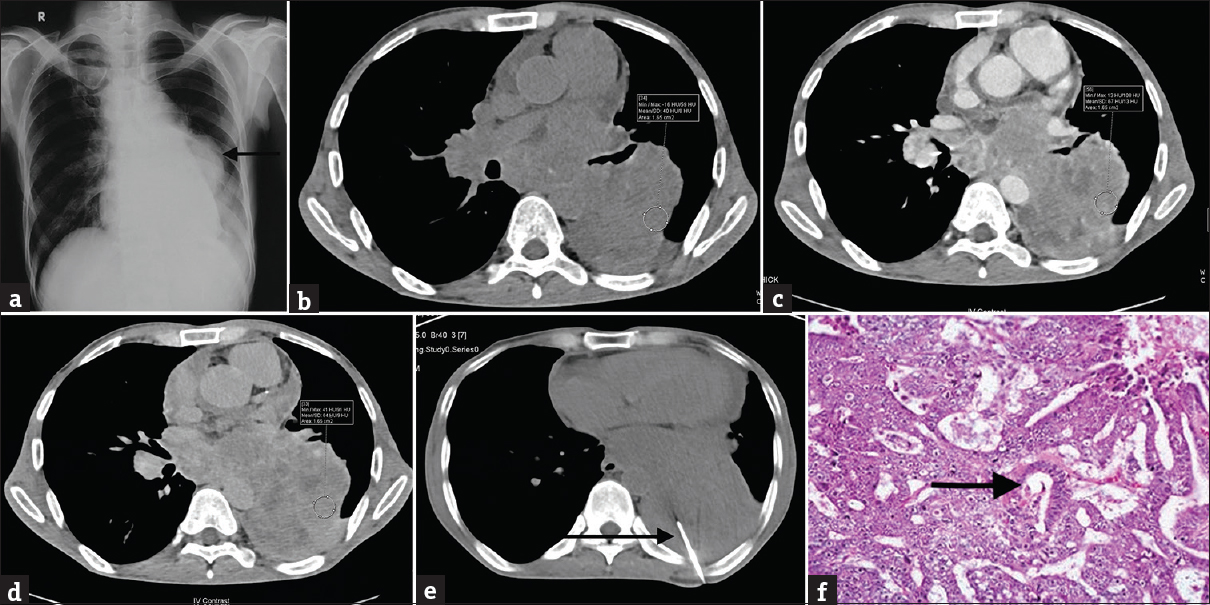
- (a) A 55-year-old male patient presented with complaints of cough and dyspnea for 2 months. Chest radiograph (posteroanterior view) of the same patient shows a well-defined radiopacity (marked by the black arrow) in the left lung middle zone. The lesion is seen merging with the left hilum; however, the cardiac silhouette is visualized separately. The patient was advised to undergo contrast-enhanced computed tomography thorax for the suspected lung mass. (b) Noncontrast multidetector computed tomography axial section (mediastinal window) of the same patient shows a well-defined soft tissue density lesion in the left lower lobe with an average attenuation of 40 HU in the region of interest (shown by the circle). (c) Contrast-enhanced multidetector computed tomography axial section (mediastinal window) in early phase of the same patient shows a heterogeneously enhancing lobulated mass lesion with an average attenuation of 67 HU in the region of interest (shown by the circle). The lesion is extending into the mediastinum with encasement of aorta and extrinsic compression along with luminal narrowing of the left main bronchus. (d) Contrast-enhanced multidetector computed tomography axial section (mediastinal window) in delayed phase (at 15 min) of the same patient shows an enhancing lesion with an average attenuation of 64 HU in the region of interest (shown by the circle). The absolute wash out comes out to be 11.11% and the relative washout comes out to be 4.47%. (e) The patient underwent computed tomography-guided biopsy of the lesion for histopathological correlation. The axial multidetector computed tomography scan (mediastinal window) shows biopsy needle (marked by the black arrow) within the lesion. (f) Computed tomography-guided biopsy specimen section stained with H and E (at low power) shows malignant cells with high N:C ratio and moderate amount of cytoplasm. The cells are in sheets and few of them are forming glands (marked by the black arrow) consistent with the diagnosis of adenocarcinoma.
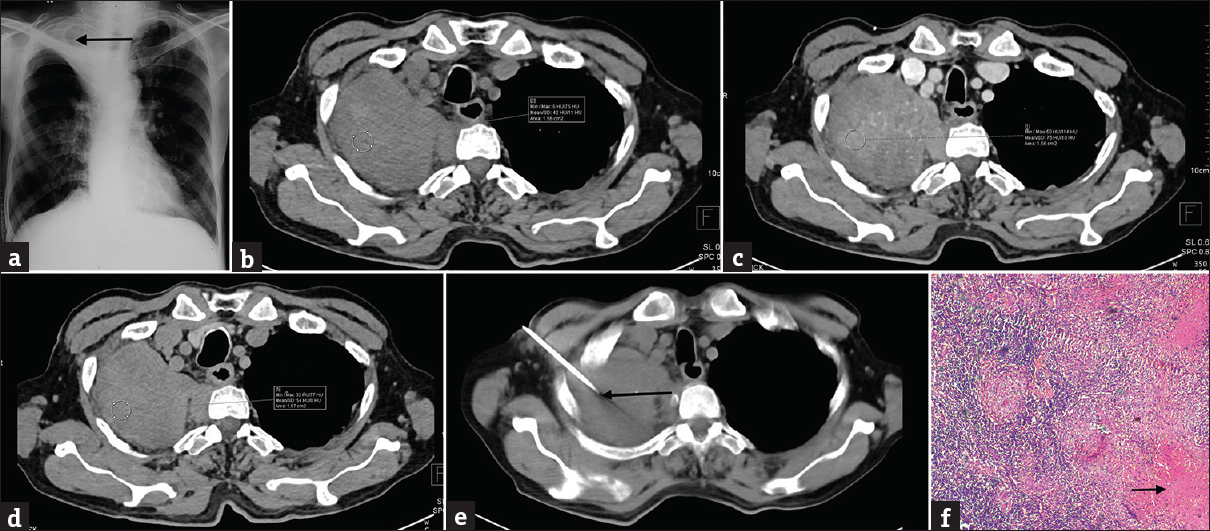
- (a) A 52-year-old male patient presented with complaints of cough, fever, and chest pain for 1 month. An ill-defined radiopacity (denoted by the arrow) is noted in apical region of the right lung. There is no evidence of bone destruction or cavitation. Fibrotic changes are noted in the right middle zone. The patient was advised to undergo contrast-enhanced computed tomography thorax for the suspected lung mass. (b) Noncontrast multidetector computed tomography axial section (mediastinal window) of the same patient shows a well-defined soft tissue density lesion in the apical segment of the right upper lobe with an average attenuation of 42 HU in the region of interest (shown by the circle). The lesion is abutting the pleura on anteroposterior and lateral aspects. (c) Contrast-enhanced multidetector computed tomography axial section (mediastinal window) in early phase of the same patient shows variegated enhancement in the lesion with an average attenuation of 75 HU in the region of interest (shown by the circle). No mediastinal extension or vascular encasement is seen. (d) Contrast-enhanced multidetector computed tomography axial section (mediastinal window) in delayed phase (at 15 min) of the same patient shows the lesion with an average attenuation of 54 HU in the region of interest (shown by the circle). The absolute washout comes out to be 63.63% and the relative washout comes out to be 28%. (e) The patient underwent computed tomography-guided biopsy for histopathological correlation. The axial multidetector computed tomography scan (mediastinal window) shows biopsy needle (marked by the black arrow) within the lesion. (f) Computed tomography-guided biopsy specimen section stained with H and E (at low power) shows large areas of caseous necrosis (marked by the black arrow). The section also shows epithelioid cells forming granulomas on a background of chronic inflammatory infiltrates with areas of necrosis consistent with the diagnosis of tuberculosis.
DISCUSSION
Enhancement of lung mass at CT is strongly predictive of malignancy and vascularity, as degree of enhancement of malignant lesions is significantly more than the benign lesions.[23451415] Yamashita et al.[16] reported that a maximum attenuation of 20–60 HU appears to be a good predictor of malignancy. In their study, Swensen et al.[2] reported that a threshold value of 15 HU produced a sensitivity of 98%, a specificity of 58%, and an accuracy of 77% for malignant nodules. Since then, the cutoff values for differentiating benign and malignant lesions have been set at 15 or 20 HU.
Cutoff values for differentiating benign and malignant lesions have increased since higher dynamic study peak enhancements were obtained with MDCT as compare to the earlier studies performed using conventional or single helical CT.[4] Therefore, by keeping 30 HU or more of net enhancement as a cutoff value in differentiation of malignant and benign lesions, sensitivity for malignant lesions was 99%, specificity was 54%, positive predictive value was 71%, negative predictive value was 97%, and accuracy was 78%. However, all of these previous dynamic CT studies[2345] mainly considered the early phase of dynamic CT scanning and showed low specificity ranging from 54% to 77% and showed false-positive results for active granulomas and thus did not help much to differentiate them from malignant lesions. In our study, a threshold net enhancement (washin) value of 22.5 HU (i.e., net enhancement more than 22.5 HU indicates malignancy) had a sensitivity of 88.5%, specificity of 57.1%, and accuracy of 82% in diagnosing malignancy on early CECT scans. The results in our study also showed that wash-in features have higher sensitivity but lower specificity in diagnosing malignant lesions. In the present study, wash-in enhancement of 22.5 HU or more was achieved by all malignant lesions.
Wash-out features at delayed CECT have been assessed in imaging characterization of adrenal lesions.[678910] However, very few studies have studied combined wash-in and wash-out properties at delayed CECT in imaging characterization of malignant and benign pulmonary nodules.[111213]
To the best of our knowledge, in the available literature, this is the first study to focus on wash-in, absolute, and relative percentage washout values at delayed CECT in imaging characterization of skeptical lung masses and then their correlation with histopathological examination.
In our study, the relative percentage washout values of malignant lesions were significantly lower than the values of the benign lesions on delayed CECT scans (P < 0.001). We also found that a threshold relative percentage washout of <16.235% calculated through receiver operating curve had 98.1% sensitivity, 85.7% specificity, and 94% accuracy in identifying malignant lesions. The absolute percentage washout values were also calculated and showed that malignant lesions have significantly lower absolute percentage washout values than the value of the benign lesions on delayed CECT scans (P < 0.001). We found out that a threshold absolute percentage washout of <42.72% had 98.1% sensitivity, 95.2% specificity, and 95% accuracy in predicting malignancy. Our study showed that by the assessment of washout characteristics, specificity in identifying malignant lesions was higher than that for wash-in features in the early phase of dynamic CT. In a study done by Ye et al.,[12] the relative percentage washout value was calculated for both malignant and benign lung nodules and showed a higher specificity in identifying malignant nodules than that for wash-in characterization in the early phase of dynamic CT scanning. However, Ye et al.,[12] did not calculate the absolute percentage washout.
The basis for the noted difference in the washout characterization of malignant and benign lesions has been attributed to the difference in their pathologic and pharmacokinetic properties. Both intravascular and interstitial spaces are notably involved in the delivery of contrast material through the lung parenchyma.[17] In general, malignant pulmonary lesions are primarily supplied by the bronchial arteries with varying degree of contribution from the pulmonary circulation.[18192021] Washout from the intravascular space takes place mainly through the pulmonary veins in the normal pulmonary tissue. However, in malignant lung lesions, outflow of contrast through the pulmonary veins is decreased, and the predominant venous outflow is through the bronchial veins into the right atrium.[18] Remarkably large interstitial space has been noticed in some human and experimental malignant tumors.[22] In the normal lung tissue, washout from the interstitial space takes place through the lymphatic vessels.[18] An extremely distinguishable feature of malignant lung lesions is the near complete absence or pronounced diminution of lymphatic outflow.[17] The impeded flow through pattern in the intravascular and the interstitial spaces leads to holding of contrast medium in the malignant lung lesions.
The intravascular space is decreased in actively infectious and inflammatory lesions.[18] In majority of the inflammatory lung processes, there is diffuse thrombosis at the level of arterioles in the pulmonary circulation. Thus, the lesion is predominantly supplied by the bronchial arteries which appear to increase in number and size.[23] Washout of the contrast from the intravascular space in the inflammatory lesions occurs through comparatively straight vessels with a normal configuration and thus not hindered. Washout from the interstitial space of the inflammatory lung nodules is escalated by the active lymphatic flow.[1724] Therefore, the retention of the contrast is improbable in majority of the inflammatory lung processes.
CONCLUSION
The assessment of suspicious pulmonary masses by calculating wash in and their absolute and relative percentage wash-out values through dynamic contrast-enhanced multidetector row computed tomography proved to be highly beneficial in the prediction of malignancy. The cutoff values obtained can be used for diagnosing malignancy with a very high diagnostic yield and can possibly obviate the need of biopsy or FNAC which require invasive procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/24/209065
REFERENCES
- Solitary pulmonary nodules: Part I. Morphologic evaluation for differentiation of benign and malignant lesions. Radiographics. 2000;20:43-58.
- [Google Scholar]
- Solitary pulmonary nodules: Dynamic enhanced multi-detector row CT study and comparison with vascular endothelial growth factor and microvessel density. Radiology. 2004;233:191-9.
- [Google Scholar]
- Pulmonary nodules: CT evaluation of enhancement with iodinated contrast material. Radiology. 1995;194:393-8.
- [Google Scholar]
- Delayed enhanced CT for differentiation of benign from malignant adrenal masses. Radiology. 1996;200:737-42.
- [Google Scholar]
- Adrenal masses: Characterization with delayed contrast-enhanced CT. Radiology. 1997;202:693-6.
- [Google Scholar]
- Adrenal adenomas and nonadenomas: Assessment of washout at delayed contrast-enhanced CT. Radiology. 1998;207:369-75.
- [Google Scholar]
- Characterization of indeterminate (lipid-poor) adrenal masses: Use of washout characteristics at contrast-enhanced CT. Radiology. 2000;217:798-802.
- [Google Scholar]
- Adrenal masses: Characterization with combined unenhanced and delayed enhanced CT. Radiology. 2002;222:629-33.
- [Google Scholar]
- Solitary pulmonary nodule: Characterization with combined wash-in and washout features at dynamic multi-detector row CT. Radiology. 2005;237:675-83.
- [Google Scholar]
- Characterization of solitary pulmonary nodules: Use of washout characteristics at contrast-enhanced computed tomography. Oncol Lett. 2012;3:672-6.
- [Google Scholar]
- Dynamic MRI, dynamic multidetector-row computed tomography (MDCT), and coregistered 2-[fluorine-18]-fluoro-2-deoxy-D-glucose-positron emission tomography (FDG-PET)/CT: Comparative study of capability for management of pulmonary nodules. J Magn Reson Imaging. 2008;27:1284-95.
- [Google Scholar]
- Solitary pulmonary nodule: CT evaluation of enhancement with iodinated contrast material – A preliminary report. Radiology. 1992;182:343-7.
- [Google Scholar]
- Solitary pulmonary nodules: Evaluation of blood flow patterns with dynamic CT. Radiology. 1997;205:471-8.
- [Google Scholar]
- Solitary pulmonary nodule: Preliminary study of evaluation with incremental dynamic CT. Radiology. 1995;194:399-405.
- [Google Scholar]
- Dynamic contrast-enhanced CT and MRI for pulmonary nodule assessment. AJR Am J Roentgenol. 2014;202:515-29.
- [Google Scholar]
- The blood supply of abnormal tissues in the lungs. J Pathol Bacteriol. 1938;47:489-99.
- [Google Scholar]
- Circulation of primary and metastatic pulmonary neoplasms. A postmortem microarteriographic study. Am J Roentgenol Radium Ther Nucl Med. 1967;100:603-19.
- [Google Scholar]
- Pulmonary metastases: Vascular supply and diagnosis. Int J Radiat Oncol Biol Phys. 1976;1:739-42.
- [Google Scholar]
- Vascular and extravascular spaces in tumors: Tumor vascular permeability. In: Peterson HI, ed. Tumor Blood Circulation: Angiogenesis, Vascular Morphology and Blood Flow of Experimental and Human Tumors. Boca Raton, Florida: CRC; 1979. p. :77-86.
- [Google Scholar]
- The bronchial circulation. Small, but a vital attribute of the lung. Am Rev Respir Dis. 1987;135:463-81.
- [Google Scholar]
- Diagnostic efficacy of PET-FDG imaging in solitary pulmonary nodules. Potential role in evaluation and management. Chest. 1993;104:997-1002.
- [Google Scholar]






