Translate this page into:
Rare Case of Reversible Acute Symmetrical Lesions of the Bilateral Basal Ganglia Associated with Diabetic Nephropathy and Chronic Renal Failure
Address for correspondence: Dr. Parag Suresh Mahajan, Department of Radiology, Hamad Medical Corporation, PO Box 3050, Doha, Qatar. E-mail: mdfrcr@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Reversible acute symmetrical basal ganglial lesion on magnetic resonance imaging and/or computed tomography in cases of diabetic nephropathy and chronic renal failure exhibiting acute onset of movement abnormalities like chorea is a very rare entity. It has characteristic clinical and imaging features. Only 29 cases are described in the literature, including the current one. These cases are predominantly Asian patients from the Far East and only one Asian Indian patient has been described. We report the second Asian Indian case of this condition and describe its various clinical and imaging features. Our aim is to educate the clinicians and radiologists about this condition, so that more such cases can be detected.
Keywords
Acute chorea
acute movement disorder
diabetic nephropathy
diabetic uremia
hemodialysis
INTRODUCTION

Development of altered mental status in patients with diabetes-induced end-stage renal disease (ESRD) is a well-known condition. On the contrary, acute hyperkinetic or hypokinetic extrapyramidal disorder associated with acute bilateral basal ganglia pathology, in cases with diabetic ESRD, is a very rare syndrome.[12] Wang et al., first described it in 1998 in three patients.[12] Since then, 26 additional cases have been reported (including this case) in the literature.[12345678910] Twenty-four of these patients are Asians, four are Caucasians, and only one is Hispanic.[6]
CASE REPORT
A 52-year-old Asian Indian man was brought by family members to the nephrology department of our hospital with complaints of sudden onset of generalized involuntary limb movements associated with mildly altered mental status, gait imbalance, and slurred speech that began 2 days earlier. Patient's relatives noticed in him recent onset of confusion, frequent amnesia, loss of alertness, disorientation, defects in judgment, poor regulation of emotions, and alterations in his perception ability, psychomotor skills, and behavior. Patient complained of recent onset of inability to walk straight. He was a known case of ESRD secondary to Type 2 diabetes mellitus for many years. He was being treated with regular hemodialysis thrice a week for 4 years. There was no recent history indicating episodes of hypoglycemia or hypotension. There was no previous history of movement disorders. Family history was unremarkable.
Clinical examination revealed him to be normotensive with a blood pressure of 120/80 mm Hg. He was conscious, but mildly confused. Generalized chorea was noted mainly involving the limbs and the face. No signs of myoclonus, asterixis, or Parkinsonism were noted. Laboratory investigations indicated raised blood urea and serum creatinine levels and slight metabolic acidosis. Blood urea nitrogen level was 30.7 (normal 1.7-8.3) mmol/L and serum creatinine level was 1073 (normal 62-124) μmol/L. The other findings were as follows: serum bicarbonate level 16 (normal 21–28) mmol/L, hemoglobin level 10.1 (normal 13-17) g/dL, random blood glucose level 10.7 (normal 3.3-5.5) mmol/L, corrected serum calcium 1.98 (normal 2.1–2.6) mmol/L, serum phosphorus 1.39 (normal 0.87-1.45) mmol/L, serum potassium 4.1 (normal 3.6-5.1) mmol/L, and serum sodium 135 (normal 135-145) mmol/L. Serum parathormone, blood iron and blood lactate levels, and total iron binding capacity were normal.
Magnetic resonance imaging (MRI) of the brain was performed on the day of the visit. The diffusion-weighted (DW) images revealed hyperintense/bright signal in the basal ganglia bilaterally. Reduced apparent diffusion coefficient (ADC) values were demonstrated in the central parts of the bilateral basal ganglia and increased ADC values were demonstrated in the periphery [Figure 1a and b].
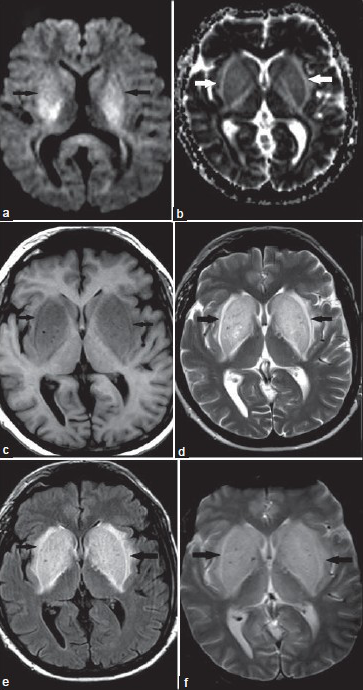
- 52-year-old man with sudden-onset chorea, altered mental status, behavioral alterations, and slurred speech for 2 days, diagnosed with reversible symmetrical basal ganglial lesions bilaterally, related to diabetic nephropathy and chronic renal failure. (a) Axial unenhanced diffusion-weighted image demonstrates symmetrical hyperintense/bright areas involving the basal ganglia bilaterally. (b) Axial unenhanced apparent diffusion coefficient (ADC) image demonstrates reduced ADC values in the central parts and elevated ADC values in the periphery. (c) Axial unenhanced T1-weighted image demonstrates symmetrical hypointense areas involving the basal ganglia bilaterally. No significant mass effect is noted. (d-f) Axial unenhanced T2-weighted, fluid attenuation inversion recovery (FLAIR), and T2*-weighted images show symmetrical hyperintense areas involving the basal ganglia bilaterally.
Symmetrical hypointense areas were noted on T1-weighted images involving the basal ganglia bilaterally [Figure 1c]. T2-weighted, fluid attenuation inversion recovery (FLAIR), and T2*-weighted images showed symmetrical hyperintense areas involving the basal ganglia bilaterally [Figure 1d–f].
Diagnosis of reversible and symmetrical lesions of the basal ganglia bilaterally related to diabetic nephropathy and chronic renal failure was made and frequency of hemodialysis was increased from three to five sessions per week. The increased frequency of hemodialysis was continued for 2 weeks. The altered mental status, behavioral changes, and slurred speech resolved within 3 days. The generalized chorea resolved completely within 6 days. After a week, the blood urea level regressed to 8 mmol/L and the serum creatinine level reduced to 308 μmol/L. He was not prescribed any particular medicine including steroids or clonazepam. Follow-up MRI of brain was performed 4 weeks after the first one, which showed complete resolution of the basal ganglial lesions bilaterally [Figure 2]. No evidence of any residual lesions was seen. Regular thrice-weekly hemodialysis was continued. He remained free of chorea and slurred speech and maintained normal mental status during a 4-month follow-up.
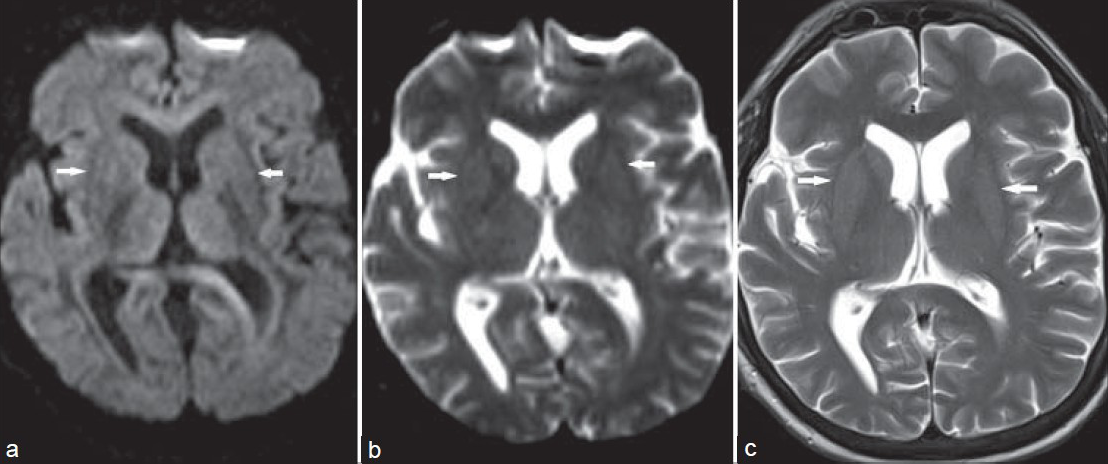
- 52-year-old man with sudden-onset chorea, altered mental status, behavioral alterations, and slurred speech since 2 days, diagnosed with reversible symmetrical basal ganglial lesions bilaterally, related to diabetic nephropathy and chronic renal failure. Follow-up (a) axial unenhanced diffusion-weighted images, (b) axial unenhanced apparent diffusion coefficient (ADC) images, and (c) axial unenhanced T2-weighted images demonstrate complete resolution of the altered signal intensities in the basal ganglia bilaterally, without any residual abnormalities.
DISCUSSION
Review of literature suggests the commonest adult movement abnormalities related to diabetic ESRD to be either chorea or Parkinsonism.[12] Both the movement abnormalities were reported in a single patient in only one of the 29 reported cases.[12] Other neurological features that are less common include mildly altered mental status, gait abnormalities, difficulty in speaking, and difficulty in swallowing. Our patient had mildly altered mental status and chorea, which suggests possibility of slight dysfunction of the cerebral cortex/gray matter.[12] Neuroimaging features are characteristic of this condition. Computed tomography (CT) and MRI, in most cases, demonstrate selective involvement of the basal ganglia bilaterally and sometimes the adjacent white matter. In our case, the patient was evaluated in detail by MRI. We performed DW, FLAIR, and T2*-weighted images over and above the routinely acquired T1- and T2-weighted images. DW images revealed cytotoxic edema in the central parts (reduced ADC values) and vasogenic edema in the periphery (increased ADC values). These features were also observed by Kim and colleagues and Lee and colleagues in patients with syndrome of bilateral acute basal ganglia lesions associated with diabetic nephropathy and chronic renal failure.[134] Permanent areas of cystic gliosis in the bilateral basal ganglia medially were reported by Kim et al.[13] In most of these reported cases, there was complete resolution of the bilateral basal ganglial lesions, similar to our case, on MRI scan performed within 3-8 weeks.[15]
The definite cause of this syndrome is unknown and various explanations have been provided by different researchers. Few of the factors that are suspected to lead to it include uremic toxins, metabolic acidosis, and diabetic microangiopathy.[7] In 2006, Lee et al., elucidated the vasogenic nature of bilateral basal ganglial edema and attributed it to focal hyperemia secondary to abnormal dilatation of small vessels.[8] In 2010, Juryńczyk et al., suggested hypoglycemia as one of the candidate trigger factors causing this syndrome and stressed on the significance of strict glucose control in uremic patients.[7] The recent article by Tajima et al., suggests the basal ganglial lesions to be due to demyelination.[9] They suggested a new demyelinating brain disease associated with diabetes mellitus and chronic renal failure.[9] In 2010, Dicuonzo et al., described the spectroscopic findings in this syndrome.[10] Significantly reduced metabolism of glucose in the bilateral basal ganglia, mainly in the putamen, was demonstrated in two cases by Wang et al., on 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) examination.[1] Reduced metabolism in the cortex of frontal and occipital lobes was also demonstrated. They hypothesized that these cases have already reduced function of the cells due to chronic diabetic microangiopathy or failure of utilization of energy. Due to this chronic metabolic and toxic insult, significant alterations occur in the metabolism of cells and there is collapse of the vasogenic auto-regulation, causing damage to tissues and tissue edema. These changes in the physiological mechanisms cause movement abnormalities. Applying this hypothesis in our case suggests tissue edema involving the bilateral basal ganglia, and thus, complete resolution without residual changes. Complete resolution of neurological abnormalities was noted in our patient within 6 days after increasing the number of hemodialysis sessions from three to five per week. Follow-up MRI obtained 4 weeks after the first one showed complete resolution of the bilateral basal ganglia lesions. A review of literature shows that resolution of clinical abnormalities may be complete in one-fifth of the cases, partial in half of the cases, and no resolution is observed in 30% of the cases.[1] Resolution of the radiologically observed abnormalities is observed in almost 90% of the cases.[15] Although the resolution of neurological abnormalities occurs is most cases, the overall long-term outcome for these cases is poor.[1] Early mortality is observed in these cases secondary to various complications like cardiac diseases, sepsis, and metabolic abnormalities.[1]
CONCLUSION
In conclusion, we report here a very rare case, the second Asian Indian case affected with reversible acute symmetrical basal ganglial lesions seen on MRI, related to diabetic ESRD, and exhibiting acute onset of chorea, altered mental status, behavioral changes, and slurred speech. Our aim is to educate the clinicians and radiologists about this condition, so that more such cases can be detected.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/29/133264
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Acute movement disorder with bilateral basal ganglia lesions in diabetic uremia. Ann Indian Acad Neurol. 2011;1:211-3.
- [Google Scholar]
- Acute movement disorders with bilateral basal ganglia lesions in uremia. Mov Disord. 1998;13:952-7.
- [Google Scholar]
- Acute bilateral basal ganglia lesions in diabetic uremia: Diffusion weighted MRI. Neuroradiology. 2007;49:1009-13.
- [Google Scholar]
- Bilateral basal ganglia lesions in patients with end-stage diabetic nephropathy. Nephrology (Carlton). 2008;13:68-72.
- [Google Scholar]
- Acute chorea and bilateral basal ganglia lesions in a haemodialysis patient. Kidney Int. 2008;73:1087-91.
- [Google Scholar]
- Reversible acute parkinsonism and bilateral Basal Ganglia lesions in a diabetic uremic patient. Case Rep Neurol. 2012;4:156-8.
- [Google Scholar]
- Hypoglycemia as a trigger for the syndrome of acute bilateral basal ganglia lesions in uremia. J Neurol Sci. 2010;297:74-5.
- [Google Scholar]
- Parkinsonism with basal ganglia lesions in a patient with uremia: Evidence of vasogenic edema. Parkinsonism Relat Disord. 2006;12:93-6.
- [Google Scholar]
- Unusual basal ganglia lesions in a diabetic uraemic patient proven to be demyelination: First pathological observation. BMJ Case Rep 2012 2012
- [Google Scholar]
- Acute extrapyramidal disorder with bilateral reversible basal ganglia lesions in a diabetic uremic patient: Diffusion-weighted imaging and spectroscopy findings. J Neurol Sci. 2010;293:119-21.
- [Google Scholar]






