Translate this page into:
Radiology Performed Fluoroscopy-Guided Lumbar Punctures Decrease Volume of Diagnostic Study Interpretation – Impact on Resident Training and Potential Solutions

*Corresponding author: Ameya P. Nayate, Department of Radiology, University Hospitals, Cleveland Medical Center 11100 Euclid Avenue, Cleveland, Ohio, 44106, United States. Ameya.Nayate@UHhospitals.org
-
Received: ,
Accepted: ,
How to cite this article: Richards TJ, Schmitt JE, Wolansky LJ, Nayate AP. Radiology performed fluoroscopy-guided lumbar punctures decrease volume of diagnostic study interpretation – impact on resident training and potential solutions. J Clin Imaging Sci 2021;11:39.
Abstract
Objectives:
Lumbar punctures performed in radiology departments have significantly increased over the last few decades and are typically performed in academic centers by radiology trainees using fluoroscopy guidance. Performing fluoroscopy-guided lumbar punctures (FGLPs) can often constitute a large portion of a trainee’s workday and the impact of performing FGLPs on the trainee’s clinical productivity (i.e. dictating reports on neuroradiology cross-sectional imaging) has not been studied. The purpose of the study was to evaluate the relationship between the number of FGLPs performed and cross-sectional neuroimaging studies dictated by residents during their neuroradiology rotation (NR).
Material and Methods:
The number of FGLPs and myelograms performed and neuroimaging studies dictated by radiology residents on our neuroradiology service from July 2008 to December 2017 were retrospectively reviewed. The relationship between the number of FGLPs performed and neuroimaging studies (CT and MRI) dictated per day by residents was examined.
Results:
Radiology residents (n = 84) performed 3437 FGLPs and myelograms and interpreted 33402 cross-sectional studies. Poisson regression demonstrated an exponential decrease in number of studies dictated daily with a rising number of FGLPs performed (P = 0.0001) and the following formula was derived: Number of expected studies dictated per day assuming no FGLPs × e-0.25 x number of FGLPs = adjusted expected studies dictated for the day.
Conclusion:
We quantified the impact performing FGLPs can have on the number of neuroimaging reports residents dictate on the NR. We described solutions to potentially decrease unnecessary FGLP referrals including establishing departmental guidelines for FGLP referrals and encouraging bedside lumbar punctures attempts before referral. We also emphasized equally distributing the FGLPs among trainees to mitigate procedural burden.
Keywords
Fluoroscopy
Lumbar
Puncture
Residents
Training
INTRODUCTION
Requests for lumbar punctures (LPs) performed with image guidance have increased over the past two decades, and radiology is now the dominant provider of LPs in Medicare patients.[1] Fluoroscopy is typically used for image guidance as it allows the operator to visualize important anatomic landmarks and the path of the spinal needle.[2] In academic centers, fluoroscopy-guided lumbar punctures (FGLPs) are typically performed by radiology residents or neuroradiology fellows in fluoroscopy suites under the supervision of neuroradiology attendings.
The clinical utility of FGLPs is high due to its high success rate[3] and ability to provide valuable information for diagnosis and treatment of patients. However, performing FGLPs can have negative implications including exposing patients to radiation and disrupting workflow for both radiologists and trainees.[1] Gaining expertise in performing FGLPs is an integral part of radiology residency and performing image-guided procedures is a core competency;[4] however, it is important to consider the time investment of trainees while performing these procedures and its impact on other essential training in neuroradiology including interpreting cross-sectional neuroimaging (CSNI) studies. Monitoring trainee progress in neuroradiology is especially important as a recent survey of neuroradiologists demonstrated some perceived decline in the capabilities of radiology trainees in the last several years.[5]
A prior study described image guided procedures as one of the primary disruptors of image interpretation tasks for trainees on the neuroradiology service.[6] In our experience, FGLPs are the mostly commonly performed procedure on neuroradiology services and to the best of our knowledge, no study has directly assessed the impact of performing FGLPs on the number of CSNI studies interpreted per day by radiology residents. The primary goal of our study is to quantify the effect that performing increasing numbers of FGLPs has on the number of CSNI studies a resident dictates in a day. We provide suggestions to mitigate burdening trainees and radiology departments with performing excessive numbers of FGLPs.
MATERIAL AND METHODS
Institutional review board
This study was given exemption from approval by the local Institutional Review Board, because the study did not access patient’s charts or protected health information.
Data collection and sorting
Number, type, and time of CSNI studies dictated and FGLPs and myelograms (FGLP-Ms) performed by radiology residents at our institution between July 1, 2008, and December 31, 2017, were extracted from our Centricity-IDX radiology information system and retrospectively reviewed. Inclusion criteria included resident dictated reports on CT/ MR studies of the head, neck, and spine in both pediatric and adult patients, FGLPs for both diagnostic and therapeutic purposes, and FGLP-Ms. Only studies dictated by radiology residents between 8 A.M. and 5 P.M. during their dedicated neuroradiology rotations (NRs) were included in the study. The reports dictated by “float” residents covering the service for only that day were excluded from the study. We excluded fellows from our data since we only have 1–2 fellows/year compared to approximately 10 radiology residents/year. Our neuroradiology division does not interpret ultrasound or radiograph examinations.
The data were categorized by the resident who dictated the study, year of training of the resident, and type of study (i.e. CT, MR, FGLP, or FGLP-M). The resident who dictated the FGLP or FGLP-M study was the assumed primary operator.
Neuroradiology resident rotations
Typically, three radiology residents (1st year residents [R1s] through 4th year residents [R4s]) and 1–2 neuroradiology fellows train on the neuroradiology service every month. Usually, R1s rotate 1–2 times/year on the neuroradiology service, 2nd years residents (R2s) rotate once per year, and 3rd year residents (R3s) and R4s rotate variably based on resident requests, scheduling limitations, and interest.
FGLP planning and procedure
Trainees reviewed the indication for the FGLP and discussed each case with the neuroradiology attending. The FGLPs were performed by residents under the supervision of the attending using the techniques outlined in the American College of Radiology-American Society of Neuroradiology-Society for Pediatric Radiology practice parameters[7] using one standard biplanar fluoroscopy machine (Phillips BV Pulsera) in one fluoroscopy suite.
Total neuroradiology studies dictated (regular workday + overnight and weekend call)
A subset of the data including the total number of CSNI studies dictated by residents on their regular NR, on-call (5 P.M.–8 A.M. and weekends), and on float rotations to cover the neuroradiology service were tracked from July 1, 2015, to June 30, 2016. The subset of the data including total CSNI studies dictated by the R1–R4 classes in the 2015–2016 years were compared to published data on the number of studies dictated by approximately 40 residents at another institution (Johns Hopkins University) from November 1, 2012, to October 31, 2013.[8] We chose to analyze the data from the 2015 to 2016 academic year since before this time period, residents were not required to submit full dictations for on-call CSNI studies and only dictated short reports describing the major clinically impactful findings and a brief interpretation. These short reports were not traceable within the RIS system. This was also the closest time range of call and regular workday data that we had to compare to the other institution’s range from 2012 to 2013.
Data analysis
The total number of CT, MR, FGLP, and FGLP-M reports dictated by each resident for each day while on the NR was tallied from July 1, 2008, to December 31, 2017. Data were imported into the R statistical environment for analysis.[9] Descriptive statistics on frequencies of cross-sectional and FGLP studies were tabulated and displayed graphically. Neither FGLP nor cross-sectional study counts were normally-distributed, but instead both followed Poisson distributions. Therefore, to understand the relationship between FGLPs and the number of cross-sectional studies, we employed log linear (i.e. Poisson) regression. We first examined data for R1s alone, including individual resident and day on the neuroradiology service as covariates. We repeated these analyses using data from residents at all levels of training (R1–R4), adding year of training as an additional covariate in the regression model. P ≤ 0.05 was defined as the threshold for statistical significance.
RESULTS
Total number of FGLPs and FGLP-Ms
From July 1, 2008, to December 31, 2017, radiology residents (n = 84) performed a total of 2706 FGLPs and 731 FGLPMs for a total of 3437 combined FGLPs/FGLP-Ms (69.3% of the total for the neuroradiology division [n = 4962]). The remainder was performed by fellows or attendings. R1s performed the majority of the FGLPs and FGLP-Ms (81.4% and 85.8%, respectively), while R4s performed the least (2.1% and 1.9%, respectively). Figure 1 for a summary of the mean FGLP and FGLP-M performed per day by resident year and Table 1 for additional summary statistics of FGLPs and FGLP-Ms performed by year of training.
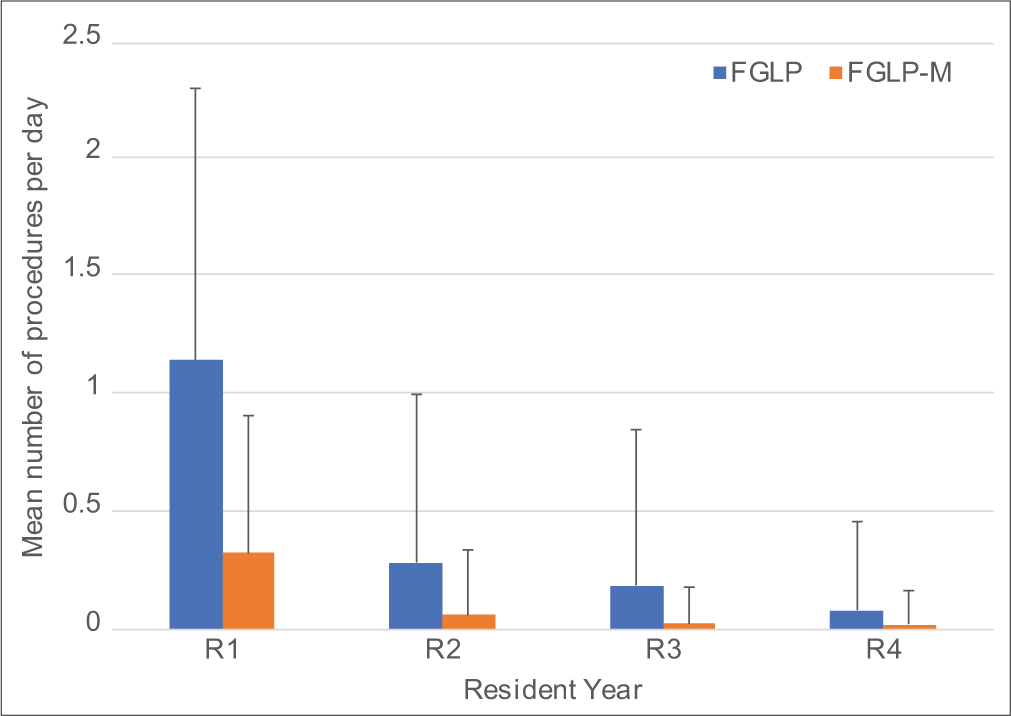
- Mean number of fluoroscopy-guided lumbar punctures (FGLP) and myelograms (FGLP-M) performed per day by resident year (R) with positive standard deviation error bars.
| 1st year residents | 2nd year residents | 3rd year residents | 4th year residents | All residents | |
|---|---|---|---|---|---|
| Total day on NR rotation | 1936 | 1327 | 398 | 685 | 4346 |
| Number residents that had NR rotation | 82 | 73 | 29 | 30 | 84 |
| FGLP | |||||
| Total | 2203 | 373 | 74 | 56 | 2706 |
| Percentage of total | 81.4 | 13.8 | 2.7 | 2.1 | |
| Mean per day | 1.14 | 0.28 | 0.19 | 0.08 | 0.62 |
| Mean per resident | 26.87 | 5.11 | 2.55 | 1.87 | 32.21 |
| FGLP-M | |||||
| Total | 627 | 80 | 10 | 14 | 731 |
| Percentage of total | 85.8 | 10.9 | 1.4 | 1.9 | |
| Mean per day | 0.32 | 0.06 | 0.03 | 0.02 | 0.17 |
| Mean per resident | 7.65 | 1.10 | 0.34 | 0.47 | 8.70 |
| FGLP+FGLP-M | |||||
| Total | 2830 | 453 | 84 | 70 | 3437 |
| Percentage of total | 82.3 | 13.2 | 2.4 | 2.0 | |
| Mean per day | 1.46 | 0.34 | 0.21 | 0.10 | 0.79 |
| Mean per resident | 34.51 | 6.21 | 2.86 | 2.33 | 40.90 |
FGLPs: Fluoroscopy guided lumbar punctures, FGLP-Ms: Fluoroscopy-guided lumbar punctures-myelograms, NR: Neuroradiology rotation
Days on rotation and diagnostic neuroradiology studies
Radiology residents rotated the greatest number of days through the neuroradiology service as R1s (n = 1936) and the least as R3s (n = 398). R1s dictated the highest number of CTs per day at 5.88 studies/day for a total of 11,392 CTs. The R4s dictated the highest number of MRIs per day at 8.37 studies/day and the highest number of total CSNI studies at 11.08 studies/day. Figure 2 for a summary of the distribution of both CSNI and FGLP/FGLP-M procedures performed by radiology trainee year and Table 2 for additional summary statistics on diagnostic studies read by year of training.
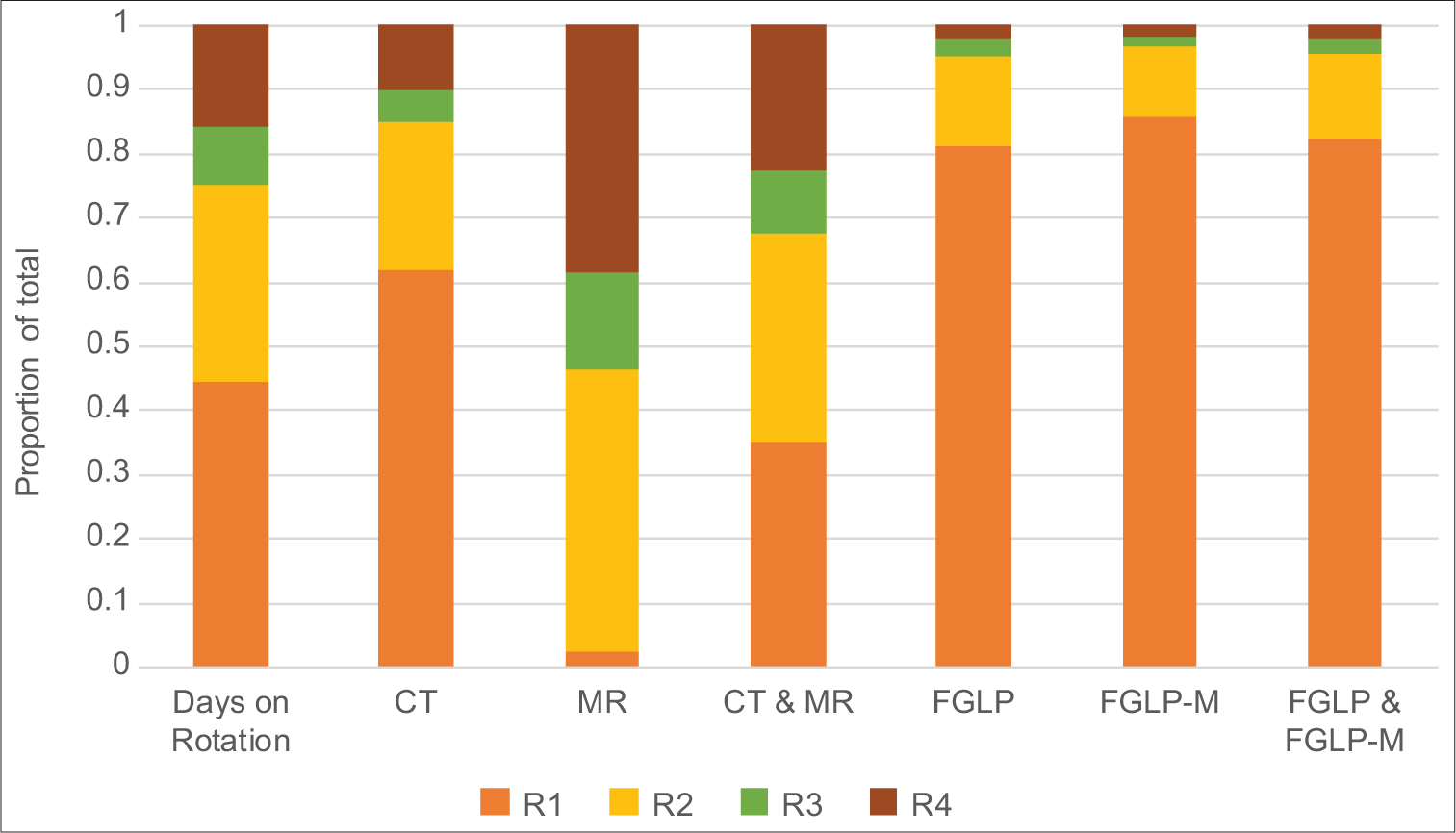
- Proportion of the total days on rotation, studies dictated (CT, MR, and CT and MR), and FGLP and/or FGLP-M procedures performed by resident year (R).
| 1st year residents | 2nd year residents | 3rd year residents | 4th year residents | All residents | |
|---|---|---|---|---|---|
| CT | |||||
| Total | 11392 | 4297 | 878 | 1861 | 18428 |
| Percentage of total | 61.8 | 23.3 | 4.8 | 10.1 | |
| Mean per day | 5.88 | 3.24 | 2.21 | 2.72 | 4.24 |
| Mean per resident | 138.9 | 58.9 | 30.3 | 62.0 | 219.4 |
| MR | |||||
| Total | 361 | 6571 | 2310 | 5732 | 14974 |
| Percentage of total | 2.4 | 43.9 | 15.4 | 38.3 | |
| Mean per day | 0.19 | 4.95 | 5.80 | 8.37 | 3.45 |
| Mean per resident | 4.40 | 90.0 | 79.7 | 191.1 | 178.3 |
| CSNR studies | |||||
| Total | 11753 | 10868 | 3188 | 7593 | 33402 |
| Percentage of total | 35.2 | 32.5 | 9.5 | 22.7 | |
| Mean per day | 6.07 | 8.19 | 8.01 | 11.08 | 7.69 |
| Mean per resident | 143.3 | 148.9 | 109.9 | 253.1 | 397.6 |
CSNI: Cross-sectional neuroimaging, NR: Neuroradiology rotation
Relationship between FGLPs and CSNI studies
The R1s performed a mean of 1.46 FGLPs/FGLP-Ms/day (range 0–7), including a mean of 1.14 FGLPs (range 0–6) and 0.32 FGLP-Ms/day (range 0–4) and interpreted a mean of 6.07 CSNI studies/day (range 0–32). R1–R4s performed a mean of 0.79 FGLPs/FGLP-Ms/day (range 0–7) and interpreted a mean of 7.69 CSNI studies/day (range 0–41). There was a significant inverse relationship between the number of FGLPs performed and CSNI studies dictated for both the R1 and R1–R4 groups (P = 0.0001). The relationship between the number of FGLPs/FGLP-Ms performed and CSNI studies dictated by residents on a given day followed a Poisson regression logarithmic relationship which can be represented by the following equation:
Eq 1:bx= b0*e(r*x)
In the equation, “bx” is the adjusted expected number of CSNI studies dictated in a day, “bo” is the number of studies which would be dictated without any FGLPs or FGLP-Ms performed (for our trainee population bo = 9.25), “r” is a constant calculated in our study to be −0.249259, and “x” is the number of FGLPs and FGLP performed that day. Figure 3 and Table 3 for further details on the relationship of FGLPs/ FGLP-Ms and CSNI studies dictated by residents.

- Daily cross-sectional neuroimaging studies versus lumbar punctures for all residents. The scatterplot demonstrates the relationship between the number of cross-sectional neuroimaging studies (CT+MR) dictated and fluoroscopy-guided lumbar punctures or myelograms performed by all residents (1st year through 4th year). To facilitate visibility of individual data points, the data are jittered at each level. Means and standard deviations are overlaid in red. The Poisson logarithmic relationship described in Eq 1 bx = b0*e(r*x) with our calculated values of bo = 9.25 and r = −0.249259 is overlaid as a dashed line.
| Number of FGLPs and FGLP-Ms | Number of days residents performed given number (% of total days on rotation) | Number of days 1st year radiology residents performed given number (% of total days on rotation) | Mean CSNI dictated all residents | Mean CSNI dictated 1st year radiology residents only |
|---|---|---|---|---|
| 0 | 2584 (59.46) | 523 (27.01) | 9.25 | 7.97 |
| 1 | 744 (17.12) | 565 (29.18) | 6.86 | 6.72 |
| 2 | 563 (12.95) | 459 (23.71) | 5.05 | 5.26 |
| 3 | 302 (6.95) | 253 (13.07) | 3.84 | 4.07 |
| 4 | 114 (2.62) | 101 (5.22) | 2.80 | 2.78 |
| 5 | 31 (0.71) | 28 (1.45) | 1.61 | 1.54 |
| 6 | 6 (0.14) | 5 (0.26) | 1.33 | 1.60 |
| 7 | 2 (0.05) | 2 (0.10) | 8.00 | 8.00 |
CSNI: Cross-sectional neuroimaging, FGLPs: Fluoroscopy guided lumbar punctures, FGLP-Ms: Fluoroscopy-guided lumbar punctures-myelograms
The mean total number of CSNI studies dictated by our resident (n = 39) including both while on the NR and on-call for the academic year of July 1, 2015, to June 30, 2016, along with comparison of mean yearly dictations by radiology residents (n ≈ 40) at another institution are displayed in Table 4.
| Residents at our institution Mean MR/CT studies per resident (2015–2016) |
Other academic institution[8] Mean MR/CT studies per resident (2012–2013) |
|
|---|---|---|
| R1 | 150.45 | 232.20 |
| R2 | 805.33 | 442.90 |
| R3 | 123.89 | 366.30 |
| R4 | 380.30 | 224.90 |
| Overall | 364.99 | 316.58 |
DISCUSSION
Study findings
Our study demonstrates a significant inverse relationship between the number of FGLPs/FGLP-Ms performed and CSNI studies dictated by radiology residents, both for R1–R4s and separately for R1s (P = 0.0001). This inverse relationship may seem intuitive but needs to be emphasized as it further builds on the results of a prior study which demonstrated the magnitude of disruption procedures can cause on the trainee workflow in neuroradiology.[6] Radiology trainees typically manage the FGLP workflow and perform majority of FGLPs in academic hospitals with supervision from attending radiologists. FGLP duties in the section may minimally affect the workflow of attending radiologists, but our findings demonstrate that these duties can significantly affect the diagnostic productivity of trainees. We derived an equation using our data, which describes the relationship between the number of CSNI studies our trainees dictated and the number of FGLP/FLGP-Ms they performed in a given day. For example, if R1s are expected to dictate 10 CSNI studies on days without the added responsibility of performing FGLPs (a = 10), then on days that they perform 1, 2, 3, or 4 FGLPs/FGLP-Ms, they would be expected to dictate approximately 7.8, 6.1, 4.7, and 3.7 CSNI studies, respectively. We realize that neuroradiology sections might have slightly different expectations of their residents, but we believe our results are generalizable to some degree since our average case volume for residents over a 1 year period was similar to another institution with approximately the same number of residents per class.[8] Furthermore, while we acknowledge that other institutions perform some of the image guided LPs using CT, we think our results would still be useful given the similar workflow of image guided LPs performed using each modality.
Developing FGLP skills in trainees
Gaining expertise in image-guided procedures is a core competency in radiology residency;[4] however, the number of image guided LPs trainees need to perform to attain competence is unknown and likely variable. The mean number of FGLPs performed by our 1st-year residents was 34.5, and although not explicitly assessed, we believe that most of our residents are comfortable performing independent FGLPs during their 2nd year call judged by their very high success rate overnight. In our experience, neuroradiology attendings determine trainee competency in performing FGLPs primarily based on subjective evaluations. More objective parameters, such as mean number of FGLPs performed by trainees, to determine competency could be established in future studies and analysis of these parameters is beyond the scope of this paper.
Previous studies have demonstrated a decline in fluoroscopy time (FT) per FGLP performed for neuroradiology fellows throughout the academic year, and a benchmark FT of 0.26 min for competency in fellows has been suggested.[10,11] Therefore, success rate of introducing the needle into the spinal canal and trends in FT could be followed for residents while on the neuroradiology service and serve as methods to track progress. Although, even as a trainee’s procedural efficiency improves, the time for preprocedural workup including lab work up, imaging review, consent, and sorting out patient transport logistics as well as waiting while collecting CSF is difficult to reduce. To the best of our knowledge, there is no published data on the mean total time required for pre-procedural workup and performing FGLPs, however based on our experience we estimate it to be 30–60 min. A prior study demonstrated a median time of approximately 50 min for neuroradiology procedures performed by trainees.[6]
Monitoring diagnostic neuroradiology training
In our section, R1s performed the highest number of daily FGLPs and dictated the highest number of CT studies per day. R2s performed the second largest number of FGLPs per day and dictated the second largest number of daily CT studies. R3s and R4s performed the least number of daily FGLPs and combined dictated the largest number of MRI studies. This distribution is consistent with our neuroradiology section’s training goals. Training of R1 and R2s is geared for them to recognize emergent imaging findings and perform FGLPs and FGLP-Ms on call. Training of R3 and R4s is geared toward recognizing subtle and complicated diseases processes, predominantly on MRI.
The relationship between the number of CSNI studies interpreted and gaining proficiency in diagnostic neuroradiology is variable. Two recent studies demonstrated a positive correlation between the number of studies dictated and both board scores and resident clinical performance.[12,13] Therefore, it is important to maximize exposure of trainees to CSNI cases, but also set reasonable expectations when residents are performing image guided LPs. Our calculated logarithmic equation could be used to adjust expectations on the number of CSNI studies a resident should dictate while performing a given number of FLGP/FGLP-Ms in a day. Our results support the assertion that attendings should not expect residents to gain efficiency in dictating studies if they have to perform image-guided LPs during the day (i.e. the resident will dictate reports faster since he/she has to perform image-guided LPs). Finally, tracking objective parameters such as board scores are also an important component of radiology training and future studies will need to further evaluate the relationship between studies read, procedural work, and board scores while controlling for confounding factors.
Potential strategies to better control image-guided LP referrals
A proper balance needs to be attained in which neuroradiology training is maximized and unnecessary image-guided LP referrals are reduced. We believe to achieve this will require strictly managing image-guided LP referrals, encouraging better training for non-radiology clinicians and trainees to perform bedside LPs.
To perform image-guided LPs on patients that truly require it, guidelines should be established and clearly communicated to the referral services. This is important both for limiting the number of unnecessary imaged-guided LP referrals and decreasing the time spent on pre-procedural tasks including ensuring appropriate patient labs and imaging studies are available and the necessary orders have been placed by the referring clinician. Our department met with clinical services that commonly order FGLPs and discussed the detrimental impact of high number of FGLP referrals on trainee education, increased cost, and unnecessary radiation. We also established departmental guidelines which were modified from the University of Wisconsin guidelines[14] and communicated these to the referring teams. We anticipate these guidelines will help decrease the number of future FGLPs referrals and will be the focus of future investigation.
As radiology continues to perform more image-guided LPs, referrals will likely continue to increase as traditional providers might lose LP technical expertise due to diminishing case load.[1] A recent study demonstrated that 84% of LPs performed on inpatients admitted to the internal medicine service at a hospital were performed by radiology or a dedicated hospital procedural service rather than by the primary internal medicine team.[15] To decrease reliance on image-guided LPs, steps should be taken to increase the frequency of successful non-image-guided LPs. In fact, the need to better prepare residents to perform bedside procedures is recognized by internal medicine training programs and solutions such as attending and resident run procedure teams have been established.[16,17] Simulation-based bedside LP training models have also been shown to increase procedural success in a prior study.[18] LP training simulators typically cost $2000–$2700 and are relatively inexpensive compared to their potential cost saving benefits.[19,20] Despite their effectiveness, a survey conducted by the Association of American Medical Colleges found that only 44% of teaching hospitals had simulation equipment available to teach trainees to perform LPs.[21]
After reducing the number of unnecessary image-guided LP referrals, the next challenge is to optimize the distribution of the imaged-guided LPs among the available personnel. Our distribution of the FGLP workload among radiology residents was initially imbalanced with the R1s performing the bulk of the FGLPs. This asymmetric distribution of performing procedures among the residency classes may seem like an anomaly, however, we suspect it is also present at many other radiology and non-radiology training programs. For example, a prior study involving neurology residents at another institution demonstrated that 76% of LPs were performed by PGY-3s due to organization of their clinic and training program,[22] which is similar to the 81.4% of FGLPs performed by R1 (PGY-2s) in our department.
While there are benefits to this model including the R1s becoming proficient to independently perform FGLPs while on call as R2s, there were detrimental effects including reduced exposure to CSNI cases. Overall, compared to another academic institution, our residents as a whole dictated a similar number of mean CSNI studies per resident per year (365.0 compared to 316.6); however, our R1s dictated a substantially lower number of studies 150.5 compared to 232.2.[8] This is at least partially due to the high number of FGLPs our R1s were performing given that the same institution reported in another article that neuroradiology fellows performed the majority of their FGLPs.[11] To mitigate this burden on R1s, the FGLPs duties were restructured toward the end of our study period by more equally distributing performance of FGLP among the R1–R4 classes. Our future study will focus on the outcome of redistribution of the FGLP workflow among R1–R4s.
Another strategy is to reduce the pre-procedural workup duties of the resident. In the surgery literature, Reines et al. suggested hiring medical students or trained secretarial staff members to help with logistical work including contacting referring team members, gathering necessary information in the medical record, and assuring appropriate orders are in place to assist residents.[23] A well-integrated PACS and electronic medical record system with customizable tools will also aid in efficiently gathering patient data.
Finally, hiring midlevel providers to perform image-guided LPs can also help decrease the burden on trainees. This allows the flexibility for residents to achieve competence in performing image-guided LPs and then primarily focus on honing their diagnostic neuroradiology skills.
Study limitations
Our study has limitations that must be considered when interpreting our results. First, ours is a retrospective study which could be affected by confounding factors such as resident interest in neuroradiology and performing procedures. Second, our data were only collected from one institution, and the resident responsibility and radiology workflow may differ from other institutions to varying degrees. Although, we believe that our residents have similar responsibilities to other institutions such as answering clinical consultations, protocoling studies, and educating other trainees and although not explicitly tested, we do not believe that these factors will disproportionately affect the number of studies our residents dictated compared to other institutions. Third, the study only accounts for FGLPs and CSNI studies for which the resident dictated the report. There may be days when residents dictated a small number of CSNI studies but had additional exposure to other neuroimaging studies by discussing additional cases in depth with an attending without dictating the study. Fourth, the primary operator for the FGLPs/FGLP-Ms was assumed to be the resident operator that dictated the study report; however, this method does not account for the time spent by other residents that may have helped with but not dictated the procedure. Finally, while variable day to day volume in the number of CSNI studies acquired in the neuroradiology section likely had some effect on the number of studies dictated by residents, our neuroradiology division generally has a surplus of CSNI studies to be interpreted and many of the studies are dictated by the attending alone without involving any trainees.
CONCLUSION
We quantified the impact of performing FGLPs has on the number of neuroradiology studies radiology residents dictate while on the NR. We offered suggestions to help decrease the burden of performing FGLPs on diagnostic radiology trainees. Our findings can be utilized by radiology departments to set reasonable expectations for trainees while performing FGLPs as well as to monitor and advance residency training. Future studies could similarly evaluate the impact of performing procedures on diagnostic training in other radiology subspecialties.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Trends in lumbar puncture over 2 decades: A dramatic shift to radiology. AJR Am J Roentgenol. 2015;204:15-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fluoroscopically guided lumbar puncture. AJR Am J Roentgenol. 2015;205:W442-50.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with traumatic fluoroscopy-guided lumbar punctures: A retrospective review. AJNR Am J Neuroradiol. 2009;30:512-5.
- [CrossRef] [PubMed] [Google Scholar]
- The Diagnostic Radiology Milestone Project. 2015. United States: Accreditation Council for Graduate Medical Education; Available from: http://www.acgme.org/portals/0/pdfs/milestones/diagnosticradiologymilestones.pdf [Last accessed on 2017 Aug 22]
- [Google Scholar]
- Baseline survey of the neuroradiology work environment in the United States with reported trends in clinical work, nonclinical work, perceptions of trainees, and burnout metrics. AJNR Am J Neuroradiol. 2017;38:1284-91.
- [CrossRef] [PubMed] [Google Scholar]
- Radiology workflow disruptors: A detailed analysis. J Am Coll Radiol. 2016;13:1210-4.
- [CrossRef] [PubMed] [Google Scholar]
- ACR-ASNR-SPR Practice Parameter for the Performance of Myelography and Cisternography. 2013. United States: The American College of Radiology; Available from: https://www.acr.org/-/media/acr/files/practice-parameters/myelog-cisternog.pdf [Last accessed on 2017 Aug 20]
- [Google Scholar]
- Comparing preliminary and final neuroradiology reports: What factors determine the differences? AJNR Am J Neuroradiol. 2016;37:1977-82.
- [CrossRef] [PubMed] [Google Scholar]
- R: A Language and Environment for Statistical Computing. 2014. Vienna, Austria: R Foundation for Statistical Computing; Available from: https://www.r-project.org [Last accessed on 2018 Nov 19]
- [Google Scholar]
- Trends in fluoroscopy time in fluoroscopy-guided lumbar punctures performed by trainees over an academic year. Acad Radiol. 2017;24:373-80.
- [CrossRef] [PubMed] [Google Scholar]
- Benchmarking lumbar puncture fluoroscopy time during fellowship training. AJNR Am J Neuroradiol. 2017;38:656-8.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation between radiology ACGME case logs values and ABR core exam pass rate. Acad Radiol. 2020;27:269-73.
- [CrossRef] [PubMed] [Google Scholar]
- Resident case volume correlates with clinical performance: Finding the sweet spot. Acad Radiol. 2019;26:136-40.
- [CrossRef] [PubMed] [Google Scholar]
- Image Guided Spine Procedures: Guidelines for Clinicians. 2018. Available from: https://www.radiology.wisc.edu/wp-content/uploads/2017/10/lp_myelo_lab_guidelines.pdf [Last accessed on 2021 May 01]
- [Google Scholar]
- Examining invasive bedside procedure performance at an Academic Medical Center. South Med J. 2016;109:402-7.
- [CrossRef] [PubMed] [Google Scholar]
- Supervising the supervisors-procedural training and supervision in internal medicine residency. J Gen Intern Med. 2010;25:351-6.
- [CrossRef] [PubMed] [Google Scholar]
- The procedure coordinator: A resident-driven initiative to increase opportunity for inpatient procedures. J Grad Med Educ. 2018;10:583-6.
- [CrossRef] [PubMed] [Google Scholar]
- Economic outcomes of the addition of fluoroscopic guidance to the lumbar puncture procedure: A call for standardized training. J Spine. 2017;6:2. Available from: https://www.omicsgroup.org/journals/economic-outcomes-of-the-addition-of-fluoroscopic-guidance-to-thelumbar-puncture-procedure-a-call-for-standardized-training-2165-7939-1000359.php?aid=85756 [Last accessed on 2018 Nov 19]
- [CrossRef] [Google Scholar]
- Simulation-based education with mastery learning improves residents' lumbar puncture skills. Neurology. 2012;79:132-7.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of M43B lumbar puncture simulator-II as a training tool for identification of the epidural space and lumbar puncture. Anaesthesia. 2011;66:493-6.
- [CrossRef] [PubMed] [Google Scholar]
- Medical Simulation in Medical Education: Results of an AAMC Survey. 2011. Washington, DC: Association of American Medical Colleges; Available from: https://www.aamc.org/download/259760/data [Last accessed on 2017 Aug 14]
- [Google Scholar]
- Residency training: A failed lumbar puncture is more about obesity than lack of ability. Neurology. 2015;84:e69-72.
- [CrossRef] [PubMed] [Google Scholar]
- Defining service and education: The first step to developing the correct balance. Surgery. 2007;142:303-10.
- [CrossRef] [PubMed] [Google Scholar]






