Radiological Imaging Findings of a Case with Vertebral Osteoid Osteoma Leading to Brachial Neuralgia
Address for correspondence: Dr. Erkan Gokce, Department of Radiology, Faculty of Medicine, Gaziosmanpaşa University, Tokat - 60200, Turkey. E-mail: erkangokce@mynet.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Osteoid osteoma is a small, benign osteoblastic tumor consisting of a highly vascularized nidus of connective tissue surrounded by sclerotic bone. Three-quarters of osteoid osteomas are located in the long bones, and only 7-12% in the vertebral column. The classical clinical presentation of spinal osteoid osteoma is that of painful scoliosis. Other clinical features include nerve root irritation and night pain. Osteoid osteoma has characteristic computed tomography (CT) findings. Because magnetic resonance imaging (MRI) findings of the osteoid osteomas causing intense perinidal edema can be confusing, these patients should be evaluated with clinical findings and other imaging techniques. In this study, we present X-ray, CT, and MRI findings of a case with osteoid osteoma located in thoracic 1 vertebra left lamina and transverse process junction leading to brachial neuralgia symptoms.
Keywords
Brachial neuralgia
cervical X-ray
computed tomography
magnetic resonance imaging
osteoid osteoma
INTRODUCTION

First described by Jaffe in 1935, osteoid osteoma is a benign bone tumor that accounts for nearly 10% of all skeletal system benign tumors.[1] Although it is rarely seen in vertebrae, it should be considered in the differential diagnosis of patients, especially those in the younger age group, with back and lumbar pain complaints which increase during the night. Early diagnosis is important to aleviate symptoms and decrease the structural spinal deformity risks such as scoliosis.[2] In this study, X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) findings of a case with osteoid osteoma located on thoracic 1 (T1) vertebra left lamina-transverse process junction leading to left brachial neuralgia symptoms are presented.
CASE REPORT
An 18-year-old male patient presented with a 6-month history of pain in the neck, shoulder, and left arm. The pain had increased over 6 months and become more evident during the night. He had no infection or history of trauma. He had been treated with salicylates and other painkillers that reduced his complaints. On physical examination, hypoesthesia was found on his C7-T1 dermatomas and no pathological finding was evident in the laboratory evaluation.
On anteroposterior cervical X-ray of the patient, a well-contoured radiolucent nodular lesion, 1.5 cm in diameter, which had a thin highly sclerotic rim around was evident on T1 vertebra left lamina-transverse process junction. In addition, minimal scoliosis whose opening was toward left was noticed on cervical vertebral axis [Figure 1]. Upon finding the brachial neuralgia and nodular lithic lesion on the bone, contrast-enhanced MRI examination was performed to determine the possible association of lesion with brachial plexus elements and neighboring tissues as well as to rule out other causes of brachial neuralgia such as disc lesions. On MRI of the patient, about 1.5 cm diameter bone lesion of slightly expansile nature located on T1 vertebra left transverse process-lamina junction was observed. There was a rim around the lesion, which was well-contoured and had focus areas void of signal on all MRI series, suggesting millimetric calcification and hypointense sclerosis. There were hypointense signals on T1-weighted series and slightly hypointense signals on T2-weighted series, concordant with intense edema in the paravertebral soft tissues and in the bone marrow of vertebra where the lesion was located and in adjacent vertebrae [Figures 2 and 3]. After the application of paramagnetic contrast agent, a heterogeneous mild enhancement was noticed on the lesion and intense medullary bone marrow enhancements were seen on adjacent bone structure. Intense enhancement was observed on the left apical pleural surface and soft tissues around the truncus, on left C7-T2 nerve roots, and paravertebral soft tissues adjacent to the lesion [Figures 4 and 5]. Although MRI findings of the lesion showing extensive edema in surrounding tissues suggested osteoid osteoma, CT examination was performed to make a more detailed evaluation of vertebral bone structures and to confirm the diagnosis. A well-contoured hypodense lesion showing typical osteoid osteoma features having heterogeneous hyperdense calcified bone matrix in T1 vertebra left lamina-transverse process junction was observed on cervicothoracic vertebra CT. Density increase concordant with intense sclerosis was noticed on adjacent bone structures [Figure 6]. After the operation, pathologic diagnosis confirmed the radiologic diagnosis of osteoid osteoma.

- 18-year-old male with a 6-month history of pain in left half of the neck, left shoulder and arm, which was more severe at the night, diagnosed with osteoid osteoma. Anteroposterior cervical X-ray shows radiolucent nodular, well-contoured lesion (arrow) having a mild sclerotic rim located in left neural arch on T1 vertebra.
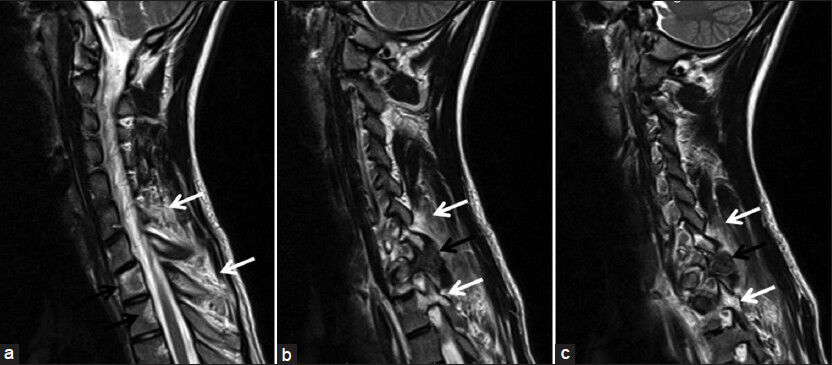
- 18-year-old male with a 6-month history of pain in left half of the neck, left shoulder and arm, which was more severe at the night, diagnosed with osteoid osteoma. T2-weighted spinal magnetic resonance imaging in sagittal plane (a) shows signals that belong to heterogeneous hyperintense edema in T1 and T2 vertebrae bodies (black arrow) and paravertebral soft tissues (white arrows) and (b and c) show slightly heterogeneous hypointense osteoid osteoma (black arrows) of a 1.5 cm diameter with hypointensities that belong to millimetric calcific matrix in T1 vertebra left lamina-transverse process junction. Edema is present in paravertebral soft tissues and in pedicules adjacent to the lesion (white arrows).
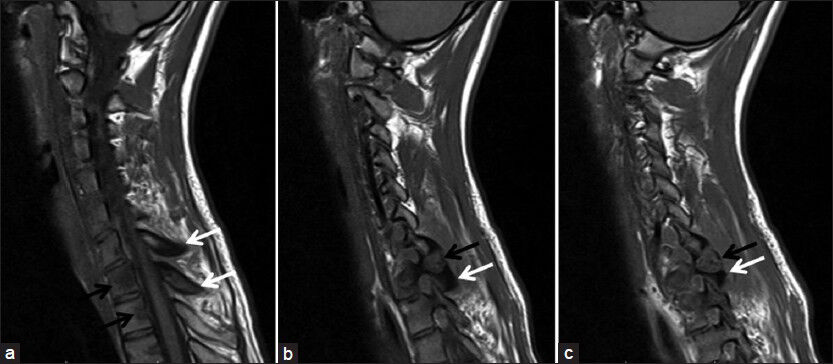
- 18-year-old male with a 6-month history of pain in left half of the neck, left shoulder and arm, which was more severe at the night, diagnosed with osteoid osteoma. T1- weighted spinal magnetic resonance imaging examination images sagittal plane show (a) signal decreases in T1 and T2 vertebra bodies concordant with edema (black arrows) and cortical sclerosis in C7-T1 spinous processes (white arrows) and (b and c) millimetric hypointense calcific foci within osteoid osteoma in T1 vertebra left lamina-transvers process junction (black arrows) and prominent sclerosis in the bone tissue around it (white arrows).
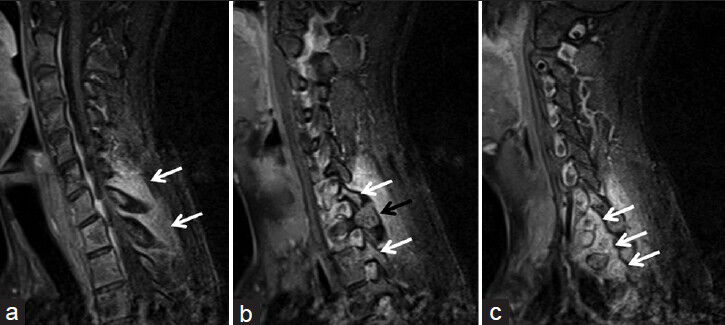
- 18-year-old male with a 6-month history of pain in left half of the neck, left shoulder and arm, which was more severe at the night, diagnosed with osteoid osteoma. Contrast-enhanced T1-weighted fat suppression spinal magnetic resonance imagingexamination images in sagittal plane show (a) marked contrast enhancement secondary to inflammation-edema in
paravertebral soft tissues, (b) osteoid osteoma (black arrow) and enhancement in the medullar bone marrow (white arrows) in the vicinity, and c) marked contrast enhancement secondary to inflammation-edema around left brachial plexus roots (white arrows).
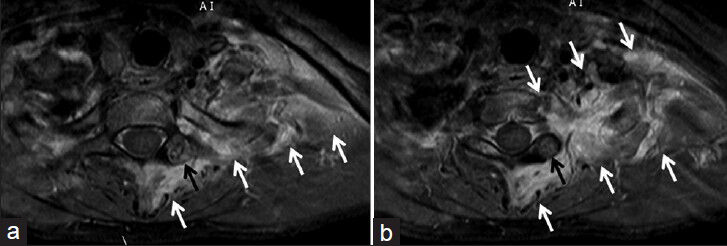
- 18-year-old male with a 6-month history of pain in left half of the neck, left shoulder and arm, which was more severe at the night, diagnosed with osteoid osteoma. Contrast-enhanced T1-weighted fat suppression spinal MRI examination obtained in (a and b) axial plane images show heterogeneous enhancement of osteoid osteoma (black arrows) and marked contrast enhancement (white arrows) around brachial plexus root-truncus on the left, in paravertebral soft tissues and in apex pleural surfaces of lung.
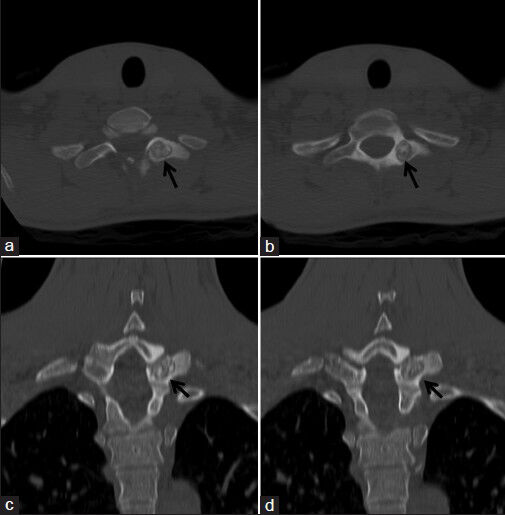
- 18-year-old male with a 6-month history of pain in left half of the neck, left shoulder and arm, which was more severe at the night, diagnosed with osteoid osteoma. Cervicothoracic spinal computed tomography examination after magnetic resonance imaging, (a and b) axial plane images, (c and d) coronal plane reformatted consecutive images show slightly contoured lobule, straight edged osteoid osteoma (black arrows) with calcific foci in T1 vertebra left lamina-transverse process junction.
DISCUSSION
Osteoid osteoma is a small benign osteoblastic tumor that has a nidus of high vascularized connective tissue surrounded by a sclerotic bone.[1] Nidus diameter is approximately 10-15 mm.[13] Nidus should be considered as osteoblastoma if it is larger than 15-20 mm.[4] These two lesions differ on the basis of size, localization, and clinical findings rather than the histologic patterns. Although three out of four of the osteoid osteomas are localized in long bones, only 7-12% develop in the vertebral column. Nearly 90% of the patients are young people below 25 years of age and it is slightly more frequently encountered in males.[24] Classical clinical finding of the spinal osteoid osteomas is painful scoliosis, nerve root irritation, and pain during the night.[2] Classically, the pain is relieved with acetylsalicylic acid.[24] In the vertebral column, osteoid osteoma is most frequently seen in the lumbar area.[13] It tends to be found in the vertebral arch and it is rarely seen in the vertebra body.[124] Osteoid osteoma more frequently occupies the lamina and pedicules on the vertebral arch, but cases involving the transverse and spinous processes have also been reported.[1]
Radiographic appearance of cortical osteoid osteomas in the shaft of long bones have a characteristic appearance.[3] Osteoid osteoma includes a structure called nidus which is radiolucent and which shows variable opacity due to varying amounts of mineralized tissue.[3] Dense fusiform reactive osteosclerosis is seen around the nidus.[3] When osteoid osteoma is in the vertebras, its diagnosis based on imaging features can be difficult.[3] In most case of spinal osteoid osteoma, radiographs demonstrate an area of neural arch sclerosis at the apex of the concavity of a scoliosis.[2] In the thoracic region particularly, the nidus is usually not evident.[2] In our case, the lesion was visualized as radiolucent area with a mild sclerotic rim around on X-ray. Before the introduction of CT imaging, scintigraphy was considered the preferred modality for osteoid osteoma diagnosis. But now, CT is considered highly sensitive for the diagnosis of these lesions. Characteristic appearance of osteoid osteoma on CT is the presence of nidus with low-attenuation and central mineralization.[2] Typical CT findings were seen in the lesion in our case. Because nidus of the osteoid osteoma have highly heterogeneous and variable appearance on MRI, its characterization is generally difficult. Enhanced and dynamic series obtained after gadolinium application have been mentioned to improve the detection of nidus. Nidus is typically seen as low signal on T2-weighted images and as intermediate signal on T1-weighted images. Because of matrix mineralization, area void of focal signal is the evidence of nidus.[2] Due to the accompanying soft tissue mass, bone marrow edema and presence of joint effusion, MRI can result in deceptive images and wrong diagnoses.[2] In our case, signal that belonged to an area of intense edema extended to a large area around the vertebrae, paravertebral soft tissues, and left brachial plexus. Nidus of osteoid osteoma had focal signal void areas in all series due to matrix mineralization, showing typical MRI features with hypointense signals in T2-weighted series and intermediate signals in T1-weighted series.
Intense perinidal edema in osteoid osteoma is considered to develop due to high level of cyclooxygenase-2 expression of neoplasmic osteoblasts in the nidus.[2] Vertebra corpus and bone marrow edema in pedicles are not specific for osteoid osteoma.[2] In differential diagnosis, degenerative disc disease, facet joint diseases, and pediculosis should be considered. Moreover, extensive edema extending to pedicle is not generally seen in degenerative disc diseases. In addition, edema extending to vertebra body does not generally exist in pediculosis developed as a result of pars defect.[2] Diagnosis of characteristic findings on MRI and evaluating MRI together with other imaging methods can minimize misdiagnosis of bone marrow edema caused by the osteoid osteoma with that due to a previous trauma edema or malignity edema.[2] Perinidal edema pattern is divided into four grades using MRI.
These are:
Grade 1: No perinidal edema
Grade 2: Perinidal edema in thin rim style
Grade 3: Edematous changes disseminated in an annular ring around nidus
Grade 4: Extensive edema larger than in grade 3, which may or may not occupy the adjacent soft tissues.[2]
Our case was determined to be Grade 4 on MRI, and we concluded that irritation caused by the intense edema was responsible for the brachial plexus neuralgia.
Traditional surgical treatments of osteoid osteoma range from local resection with a burr and curettage to wide resection with bone grafting and metallic fixation. Surgical therapy is successful in 88-100% of cases in the published series.[5] However, surgery involves longer inpatient treatment with longer anesthesia times, more extensive tissue exposure, tissue damage, scarring, morbidity, and recovery time.[5] Surgery still has a role for those appendicular lesions where the neurovascular bundle is within 1-1.5 cm of the nidus, where the histology of the lesion is in doubt or where the symptoms persist after two ablative procedures.[5] In recent years, the use of the CT-guided percutaneous radiofrequency thermoablation (PRT) has been reported with good results and this has been shown to have similar recurrence rates to open surgery, but with fewer complications and shorter periods of hospital stay.[5] However, use of PRT in spinal osteoid osteomas need to be discussed. In early studies, use of PRT was not recommended on the grounds that it could cause damage to spinal neural structures.[6] However, recent studies mention safe use of PRT in the treatment of spinal osteoid osteomas.[78] Due to the presence of a lesion located in lamina-transverse process junction with a large nidus of 1.5 cm diameter in our case, an operative approach rather than PRT was considered to be better. Magnetic resonance-guided focused ultrasound surgery which has been gaining importance in recent years is a completely noninvasive thermal ablation modality.[9] Its palliative use in bone lesions primarily for the treatment of pain in metastatic tumors indicates its possible use in primary bone tumors such as osteoid osteoma in the near future.
CONCLUSION
Recognizing radiologic features is essential for early diagnosis and treatment of osteoid osteoma. Because MRI findings can be confusing in patients with intense perinidal edema, these patients should be evaluated with other imaging methods and on clinical findings. Although they are infrequent cause of brachial neuralgia, osteoid osteomas located on upper thoracic vertebrae should be considered in the differential diagnosis of diseases that manifest themselves as brachial neuralgia.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/54/122324
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Imaging features of spinal osteoid osteoma with emphasis on MRI findings. Eur Radiol. 2005;15:2396-403.
- [Google Scholar]
- Osteoid osteoma: A rare cause of brachial neuralgia. Childs Nerv Syst. 2002;18:161-3.
- [Google Scholar]
- Computed-tomography-guided percutaneous radiofrequency thermoablation for the treatment of osteoid osteoma-2 to 5 years follow-up. Int Orthop. 2009;33:215-8.
- [Google Scholar]
- Osteoid osteoma: Percutaneous treatment with radiofrequency energy. Radiology. 2003;229:171-5.
- [Google Scholar]
- CT-guided percutaneous radiofrequency ablation of spinal osteoid osteoma. Chin Med J (Engl). 2011;124:4083-5.
- [Google Scholar]
- Osteoid osteoma of the spine: CT-guided monopolar radiofrequency ablation. Eur J Radiol. 2009;71:564-9.
- [Google Scholar]
- MR-guided focused ultrasound surgery (MRgFUS) for the palliation of pain in patients with bone metastases: Preliminary clinical experience. Ann Oncol. 2007;18:163-7.
- [Google Scholar]






