Translate this page into:
Radiation Reduction in Low Dose Pulsed Fluoroscopy versus Standard Dose Continuous Fluoroscopy during Fluoroscopically-Guided Lumbar Punctures: A Prospective Controlled Study
Address for correspondence: Dr. Shyam Sabat, Department of Radiology, H066, Penn State Milton S Hershey Medical Center, Hershey, PA 17033, USA. E-mail: ssabat@pennstatehealth.psu.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Purpose:
The purpose of this study was to evaluate radiation dose reduction in fluoroscopically guided lumbar punctures (FGLP) using “pulsed fluoroscopy in a low dose mode” compared with the commonly used “continuous fluoroscopy in a standard dose mode” while maintaining the technical success.
Materials and Methods:
Thirty-five consecutive patients who underwent FGLP divided randomly to seventeen patients in the control group with standard dose continuous FGLP and eighteen patients in the study group with low-dose low-frame-rate of 3 frames per second (fps) FGLP. Entrance surface dose measurements from a dosimeter device were recorded as well as the dose area product (DAP).
Results:
A total of 35 patients with average age of 52 years (range: 15–87 [±17 standard deviation [SD]]) were evaluated. Average entrance surface dose of the study group was significantly lower (3.81 mGy [range: 0.21–11.14, [±2.8 SD]]) compared with the control group (22.45 mGy [range: 1.23–73.44, [±19.41 [SD]]). The average DAP of the study group (10 mGy·cm2 [range: 1–41, [±9.8 SD]]) was also significantly lower than the control group (65 mGy·cm2 [range: 5–199, [±53 SD]]). Success rate was similar between the study and control groups.
Conclusion:
Low dose pulsed fluoroscopy of 3 fps significantly reduces radiation exposure by about 600% compared with standard dose continuous fluoroscopy in FGLP. Utilizing this radiation saving strategy will allow to dramatically reduce radiation exposure, without impacting the technical success rate.
Keywords
Fluoroscopy
lumbar puncture
radiation

INTRODUCTION
Lumbar puncture (LP) is generally performed using anatomic landmarks, however, in some cases, such as large body habitus or significant lumbar spondylosis, these methods are unsuccessful, and image guidance is required.[1] Fluoroscopically-guided (FGLP) is an effective alternative to bedside LP as it can visualize the bony structures and guide the operator to accurately place the needle in the spinal canal in real time.[2] FGLP is a common neuroradiologic procedure, with the main disadvantage of ionizing radiation that can lead to cumulative radiation doses, potentially increasing the long-term risk of cancer.[3]
The fluoroscopic X-ray beams for FGLP can be produced in either a continuous or a pulsed fashion. Changing the tube dose output (instantaneous dose rate; mGy/s) or the number of frames per se cond (fps) or both will change the cumulative radiation dose.[4] FGLP is operator dependent, and the radiologist should try to keep both parameters as low as possible; in a way that the radiologist's clinical confidence is not degraded by the inadequate image quality. Selecting and using the fluoroscopic dose rate and frame rate that optimizes the balance between aspects of image quality and the patient dose is important to patient management.
The default mode in most fluoroscopic machines is the continuous mode which has a frame rate of about 30 fps. Such high rates while useful for temporally changing information as in angiography is wasteful for static structures such as the spine, and result in unnecessary, harmful radiation to the patient as well as the physician operator. Early studies did not find significant dose reduction in pulsed compared with continuous fluoroscopy due to the “ramp and trail effect” of older X-ray tubes. However, newer X-ray tubes can now deliver a more uniform current in a pulsed fashion that reduces radiation dose.[5]
To the best of our knowledge, no previous study has compared radiation dose received in the continuous mode with the pulsed mode in FGLPs. The purpose of this study was to evaluate whether this change of mode would result in a radiation dose reduction and to evaluate the feasibility and technical success rate.
To further reduce radiation doses, we performed the “pulsed fluoroscopy in a low dose tube output” setting and compared it to the usual default of “continuous fluoroscopy in a standard dose tube output” setting.
MATERIALS AND METHODS
The present study was approved by the Local Institutional Review Board.
Patient population
The study was carried out as a randomized control study without any blinding.
Thirty-seven consecutive patients who underwent FGLP at our institution from May 1, 2011 to July 30, 2011 (3 months) were included in our study. The first 19 patients were allocated for the control group and the following 18 patients constituted the study group. Two patients from the control group were excluded due to technical measurements failure.
FGLPs were performed in the fluoroscopy suite on adult outpatients, inpatients, and emergency room (ER) patients.
As per the standard policy in the radiology department, inpatients and ER patients had at least one failed attempt at bedside LP.
Procedure technique
Following a written informed consent for the LP procedure and for participating in the study, all patients underwent FGLP in the prone position by using a standard fluoroscopy machine unit (Philips Super 80 CP) in the fluoroscopy suite.
A radiopaque BB marker was taped to an optically stimulated luminescent (OSL) dosimeter (Landauer, Glenwood Illinois) which was then taped to the patients’ abdomen above the umbilicus along the patients’ centerline. The marked device position was evaluated and corrected to prevent overlap with the LP access site and to assure presence in the radiation field during the entire procedure. This OSL measured the entrance surface radiation dose.
The fluoroscopy setting was designed to be on continuous mode (30 fps) for the control group as the standard care used in our institution, and on pulsed mode (3 fps) for the study group [Figure 1]. To further reduce the radiation dose, we also changed the tube output in the study group, from a standard mode to low-dose mode. The tube output for the control group was kept at standard dose. We avoided the pediatric dose mode due to consensus opinion that the images were too noisy for high body mass index (BMI) patients. Positioning time of the fluoroscopy tube was also included in the calculations and were performed by the radiologist.

- The fluoroscopy settings for control (a) and study (b) groups.
FGLPs were performed using techniques as dictated by the American Society of Neuroradiology (ASNR) guidelines and American College of Radiology – ASNR –Society for Pediatric Radiology (ACR-ASNR-SPNR) parameters.[6] Under fluoroscopy, the X-ray tube was maneuvered to an oblique orientation to optimize the view of the lumbar interlaminar spaces. The lumbar spinal canal was accessed using strict aseptic technique mostly at the L2–L3 or L3–L4 level but also at the level of L4–5 and L5–1S. A 3.5 inch or 5.0 inch beveled tip 22G spinal needle was advanced into the lumbar spinal canal using intermittent fluoroscopy until egression of CSF fluid after the removal of the stylet, confirmed access to the thecal sac.
A Scout film was avoided in all (control as well as study group) but 2 cases where it was inadvertently taken by radiologic technicians despite being asked not to; but the dosimeter had not been placed by then. Fluoroscopic image grab was used to document the position of the needle and film exposures were avoided. Collimation was kept as minimum necessary to perform the procedure while including the dosimeter in the direct radiation field. When myelogram was performed following FGLP, the dosimeter was removed prior to tracking the contrast or taking films, and hence, dosimeter measured only the fluoroscopic radiation related to the lumbar puncture. Hence for overall data analysis and conclusion purposes, the myelograms could be considered FGLPs.
FGLPs were performed by diagnostic radiology residents or neuroradiology fellows, under the supervision of a neuroradiology attending or directly by an attending (attending experience in FGLPs ranged from 2 to 15 years).
Following the procedure, the skin dosimeter was removed and analyzed using the Landauer microStar dosimeter reader with the 80 kVp X-ray calibration setting.
Data collection
A standard LP reporting template was used by all providers performing and reporting FGLPs in the Neuroradiology Department.
Demographic data including patient's age, BMI, and gender were recorded. The clinical indication, level of procedure, needle size, operator's training level, fluoroscopy setting, fluoroscopy time (FT), and dose area product (DAP) were recorded. The primary operator was assumed to be the most junior operator. Dose measurements from the dosimeter device were recorded as well.
Raw data were imported into the STATA statistical software for visualization and statistical analysis. Continuous variables were described as a mean ± standard deviation (SD) and categorical variables as frequencies (percentage).
Two sided t-test was performed for continuous variable and nonparametric test was performed for categorical variables. Linear regression was performed for two sided t-test for body-dose and DAP. P ≤ 0.05 was defined as the threshold for statistical significance.
RESULTS
A total of 37 patients (15 males and 22 females) with an average age of 52 years (range: 15–87 [±17 SD]) had undergone FGLPs in our institution. Of them, 2 cases were excluded from statistical calculation; one due to using a higher pulse rate and one because the dosimeter was not included in the field of view.
The control group consisted of 17 consecutive patients undergoing standard dose continuous FGLPs and the study group consisted of 18 consecutive patients undergoing low dose pulsed FGLPs. No significant demographic differences were found between the study and control groups. Table 1 shows the baseline characteristics of the study and the control group.

A total of 20 FGLPs (57%) were performed for an indication of LP and 15 FGLPs (43%) were performed for the indication of myelogram. FGLP were mostly performed in levels in L2–L3 and L3–L4 (n = 30, 85%) and were not significantly different between control and study group. More FGLPs were performed at lower levels in the study group L4–5 and L5–S1 (n = 5, P < 0.05).
The mean FT was longer in the control group (39 s vs. 32 s), but this was not statistically significant (P = 0.37). Two patients from the control group required two puncture sites to complete the procedure, and their FT was not significantly longer compared to the rest of the patients who underwent puncture at only one site. Eighty-two percent of FGLPs were performed by diagnostic radiology resident/neuroradiology fellow supervised by an attending (12:17, control: Study), and 18% were performed using a neuroradiology attending (5:1, control: Study).
The average entrance surface dose for the control group was 22.45 mGy (range: 1.23–73.44, [±19.41 SD]) and for the study group was 3.81 mGy (range: 0.21–11.14, [±2.8 SD]). The average DAP for the control group was 65 dGy·cm2 (range: 5–199, [±53 SD]) and for the study group was 10 dGy·cm2 (range: 1–41, [ ±9.8 SD]) [Table 2].

Unadjusted entrance surface dosage received was significantly lower among the study group compared with the control group (3.81 vs. 22.45, P < 0.001). This represents a very significant 5.9 times reduction (approximately 600%) of entrance surface dose [Table 2]. Similarly, DAP was significantly lower among the study group compared with the control group (10 vs. 65, P < 0.001); which is a 6.5 times reduction in dose.
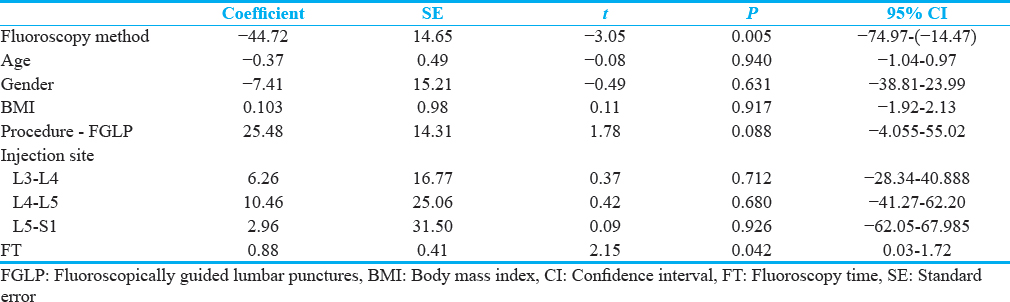
The fluoroscopy mode had the strongest influence on the significant dose reduction between the study and control groups. The FT had a significant positive coefficient on the dose reduction but negligible compared to the fluoroscopy mode [Tables 3 and 4].

Technical success rate was similar in both the study and the control group. In both groups, there was not any failure to perform the procedure. Assessment of the quality of images was only qualitative and was done during the procedure by the performing physician.
DISCUSSION
FGLPs has been increasing in the past two decades with radiology now being the overall dominant provider.[7] There are very few studies evaluating radiation reducing strategies in FGLPs. One of the strategies is changing from continuous fluoroscopy mode to pulsed fluoroscopy mode, which has been known as a radiation sparing technique, but has never been validated in FGLPs.[8] The study results show a significant dose reduction with similar clinical outcomes and success rates. We suggest that this common procedure can be safely and easily performed using low dose pulsed fluoroscopy mode.
Our results show that the FT was longer in the control group compared with the study group, but this was not statistically significant (P = 0.37). Even though most of the examinations in the control group were performed by an attending, while most studies in the study group were performed by a trainee, the FT was longer in the control group. This is indeed in contrast to previous results which found inverse relation between the level of training and the FT.[7] We attribute the slightly longer FT in the control group to two cases requiring LP punctures at two lumbar spine levels.
BMI of the patients in this study was over 30 in both the study and the control groups and was not significantly different. This result is in correlation with previous studies indicating an overall increase in FGLPs performed by radiologists in the past two decades mostly due to the indication of obesity.[9] Obese patients present with multiple potential difficulties with longer FT for LP access, limited ability to visualize bony landmarks, particularly as the radiation dose decreases, and the absence of anatomical landmarks with increasing subcutaneous fat.[10] Patients in the study and control groups had nearly identical BMI which removes any bias of one group being more difficult than the other.
Pulsed fluoroscopy was initially developed to decrease patient FT by reducing the number of exposures per se cond. Early fluoroscopy units, however, produced pulses with a “ramp and trail” effect (bell-shaped curve of increasing and decreasing current) which increased the radiation dose per pulse causing conventional pulsed fluoroscopy to offer minimal dose savings over continuous fluoroscopy.[5] Newer X-rays units minimize the “ramp and trail effect” and produce an image at a set amount of radiation and reduce the exposure time.[11] This technology potentially reduces radiation exposure with a lower pulse rate while maintaining image contrast.[12]
To the best of our knowledge, no previous study has directly compared radiation dose received in the continuous mode and the pulsed mode in FGLPs. We revealed a significant dose reduction in radiation dosage between low dose pulsed fluoroscopy compared with standard dose continuous fluoroscopy. Usually, the radiation doses per se cond are higher in the pulsed mode versus the continuous mode and the increased number of pulses per pedal depression in the continuous mode accounts for the overall greater radiation dose. We wanted to evaluate whether additional radiation saving strategy (low dose) can be applied without affecting the technical success of the procedure. Moreover indeed, the image quality and technical success were not significantly different between the study and control groups. We cannot estimate as to how much the radiation dose reduction was due to the used of pulsed fluoroscopy and how much is attributed to the low dose technique. This matter can be evaluated in further studies differentiating these two techniques of dose reduction.
Brook et al. have evaluated the radiation doses of FGLP while comparing them to computed tomography guided LPs, and found a mean DAP of 10 Gy × cm2 and average estimated effective dose of 2.9 mSv.[13] Our radiation results were similar, especially when looking at the study group, while the radiation results of the control group were significantly higher. The fluoroscopy mode (continuous/pulsed) was not detailed in their study while other radiation reducing strategies were used. Therefore, we suggest that using the low dose pulsed techniques can be safely used for FGLPs.
One potential limitation of pulsed fluoroscopy is a potential loss of diagnostic information. High frames rate is usually useful for dynamic procedures where the data changes rapidly. However, where neither the patient nor the anatomic part being imaged is moving fast, a low frame rate should suffice. FGLP is a study with minimal temporal change, which makes low rate pulsed fluoroscopic examinations very feasible with high successful outcome of the procedure. Image quality, although inferior, resulted in success rate of 100% in both control and the study group [Figure 2].

- Fluoroscopically-guided lumbar puncture of the control (a) and study (b) groups. Images quality was sufficient for the procedure.
We also were able to perform most of the studies without using scout films for guidance in the study as well as control groups. A fluoroscopic last image grab was used for initial guidance and planning without exposing the patient to more radiation.
There are some limitations to this study. The study involved a single center, relatively small study group and the operators were not blinded to which mode of operation they were using. Moreover, the operators were not homogeneous among the study and control group. Despite these limitations, this study reveals that pulsed fluoroscopy dramatically reduces exposure compared with continuous fluoroscopy. This study also demonstrates that low rate fluoroscopy produced images that are adequate to perform FGLP with high success rates.
To the best of our knowledge, only one previous study performed on patients undergoing percutaneous urologic procedures has demonstrated decreased entrance surface dose radiation by changing default setting on fluoroscopic equipment from continuous to pulsed radiation and the default tube output dose to half-dose.[14]
CONCLUSION
Low dose pulsed fluoroscopy of 3 fps with a low-dose tube output significantly reduces radiation exposure by means of almost 600% compared with the default standard dose continuous fluoroscopy in FGLPs. Utilizing this radiation saving strategy will allow to dramatically reduce radiation exposure, while maintaining success rate. We strongly recommend the use of the lowest available frame rate and in a low-dose mode setting when performing FGLP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/9/227044.
REFERENCES
- Dose reduction in gastrointestinal and genitourinary fluoroscopy: Use of grid-controlled pulsed fluoroscopy. AJR Am J Roentgenol. 2000;175:1453-7.
- [Google Scholar]
- ACR–ASNR–SPR practice parameter for the performance of myelography and cisternography. 2013. Available from: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/myelog-cisternog.pdf?la=en
- [Google Scholar]
- Trends in lumbar puncture over 2 decades: A dramatic shift to radiology. AJR Am J Roentgenol. 2015;204:15-9.
- [Google Scholar]
- Radiation exposure during continuous and pulsed fluoroscopy. J Endourol. 2013;27:384-8.
- [Google Scholar]
- Difficult lumbar puncture: Pitfalls and tips from the trenches. AJNR Am J Neuroradiol. 2017;38:1276-83.
- [Google Scholar]
- Fluoroscopic-guided lumbar puncture: Fluoroscopic time and implications of body mass index – A baseline study. AJNR Am J Neuroradiol. 2014;35:1475-80.
- [Google Scholar]
- Radiation exposure reduction during voiding cystourethrography in a pediatric porcine model of vesicoureteral reflux. Radiology. 2006;238:96-106.
- [Google Scholar]
- Reduction of radiation dose in pediatric patients using pulsed fluoroscopy. AJR Am J Roentgenol. 1996;167:1247-53.
- [Google Scholar]
- Comparison of CT and fluoroscopic guidance for lumbar puncture in an obese population with prior failed unguided attempt. J Neurointerv Surg. 2014;6:324-8.
- [Google Scholar]
- Changing default fluoroscopy equipment settings decreases entrance skin dose in patients. J Urol. 2016;195(4 Pt 1):992-7.
- [Google Scholar]






