Translate this page into:
Practice enhancements with FastStroke ColorViz analysis in acute ischemic stroke

*Corresponding author: Vivek Pai, Division of Neuroradiology, Joint Department of Medical Imaging, University of Toronto, Toronto, Canada. vivhekpai@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pai V, Ti JP, Tan LQ, Ho TS, Tham C, Sitoh YY. Practice enhancements with FastStroke ColorViz analysis in acute ischemic stroke. J Clin Imaging Sci 2022;12:19.
Abstract
In acute ischemic stroke (AIS), large vessel occlusion (LVO) and the status of pial collaterals are important factors in decision-making for further treatment such as endovascular therapy. Multiphasic CT Angiogram (mCTA) is the mainstay of AIS imaging, allowing detection of LVO, evaluation of intracranial arterial dynamics, and quantification of pial collaterals. However, thorough mCTA evaluation entails scrutiny of multiple image datasets, individually and then simultaneously, which can be time-consuming, causing a potential delay in treatment. ColorViz (FastStroke, GE Healthcare, Milwaukee, Wisconsin) is a novel CT application which combines mCTA information into a single color-coded dataset for quick, unequivocal evaluation of pial collaterals. In our practice, ColorViz is both time-saving and increases the diagnostic accuracy of LVO and pial collaterals as well as medium vessel, multivessel and posterior circulation occlusions. In this article, we discuss the practical aspects of ColorViz in patients presenting with AIS.
Keywords
Stroke
Pial Collaterals
ColorViz
INTRODUCTION
Cerebral ischemia triggers the recruitment of multiple subsidiary anastomotic vascular pathways known as pial collaterals.[1] This homeostatic response helps preserve cerebral perfusion and prolongs sustenance of the penumbra, resulting in reduced infarct volume.[2,3] Greater collateralization has also been associated with the enhanced benefit of endovascular therapy (EVT) and intravenous thrombolysis as well as a reduced risk of hemorrhagic transformation. This ultimately translates into better neurological outcomes and reduced mortality.[3,4] Over the years, the combination of unenhanced CT of the brain followed by a CT angiogram has emerged as the standard investigation in the setting of acute ischemic stroke (AIS), mainly due to its easy availability and speed of image acquisition.[5,6] A single-phase CT angiogram can accurately identify the site of occlusion; however, it lacks temporal resolution, limiting the evaluation of pial collaterals.[7]
It is in this context that multiphasic CT Angiogram (mCTA) was developed with the aim to provide time-resolved images of the intracranial arteries for quantification of collaterals.[7] mCTA consists of an arterial phase angiogram obtained from the arch of the aorta to the vertex followed by two venous phases (equilibrium/peak venous and delayed/post-venous phases) acquired from the base of the skull to the vertex.[7,8] Postprocessed mCTA thus consists of three gray-scale image datasets of the craniocervical vasculature, with multiplanar reconstructions. The technique needs no additional contrast material injection or special vendor package for postprocessing.[8] Evaluation of collaterals requires the operator to either assess the three phases individually or to manually co-register all the phases and scroll through them simultaneously.[7] It also requires expertise and is often time-consuming which is a major limitation in an already time-sensitive clinical setting.[7]
FastStroke and ColorViz
FastStroke (GE Healthcare, Milwaukee, Wisconsin) is a CT software used in AIS imaging. It provides a comprehensive, progressive workflow for image analysis with autogenerated multiplanar reformats of the CT stroke imaging protocol (unenhanced CT of the brain, mCTA). In addition, it auto-registers all phases of the mCTA side-by-side, to facilitate collateral vessel review, and also generates CT perfusion images for analysis.
The ColorViz application of FastStroke combines vascular information from all phases of mCTA into a single color-coded imaging series. It displays consolidated information of intracranial arterial dynamics which helps quantify the overall and phase specific extent of pial collaterals.[9] Vessels are assigned colors based on the temporal distribution of maximum contrast opacification; the arterial phase is coded red, the venous phase in green, and the delayed phase in blue.[9] The display layout is split into three viewports, showing colorized maximum intensity projections (MIP) in the axial, coronal, and sagittal planes. These color maps are available for review within 5–10 seconds.[9]
Evaluation of pial collaterals
Upon localizing the occlusion, the operator can visually assess pial collaterals using ColorViz by determining the predominant color in the affected vascular territory (color present in >40% of vessels).[9] Predominantly red vessels indicate no delay while green or blue vessel predominance indicate a 1-phase or 2-phase delay, respectively.[9] With a single imaging series, ColorViz combines the visual advantages of color and technical advantages of mCTA.[9] It potentially expedites the assessment of pial collaterals (a few seconds) compared to conventional gray-scale mCTA, which impacts further treatment.[9] Verdolotti et al. used a 3-point grading scale for evaluating collaterals:[10]
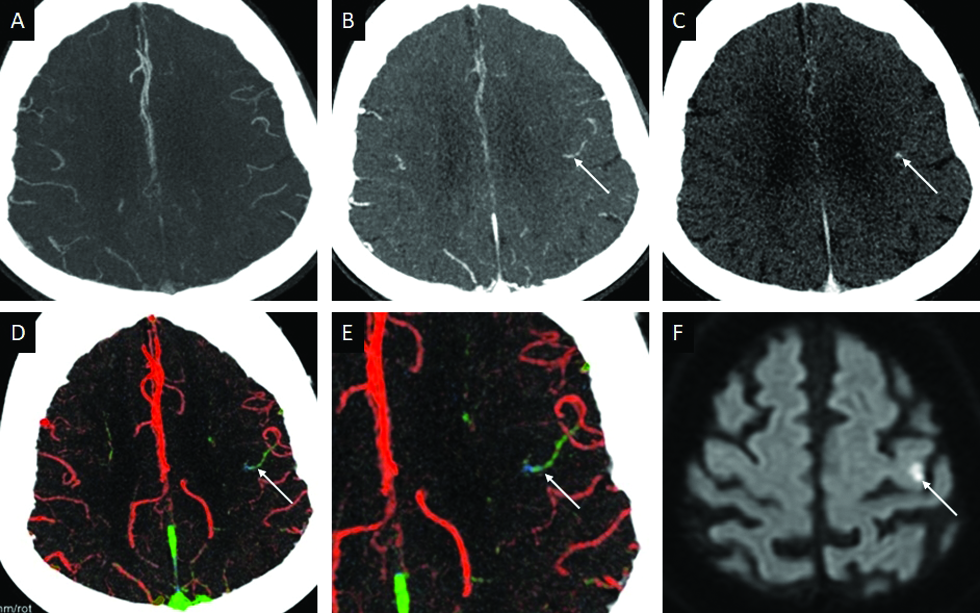
“Good” collateral circulation (score 3): Prevalence of red vessels distal to the occlusion with only slightly reduced pial collateral representation [Figure 1].
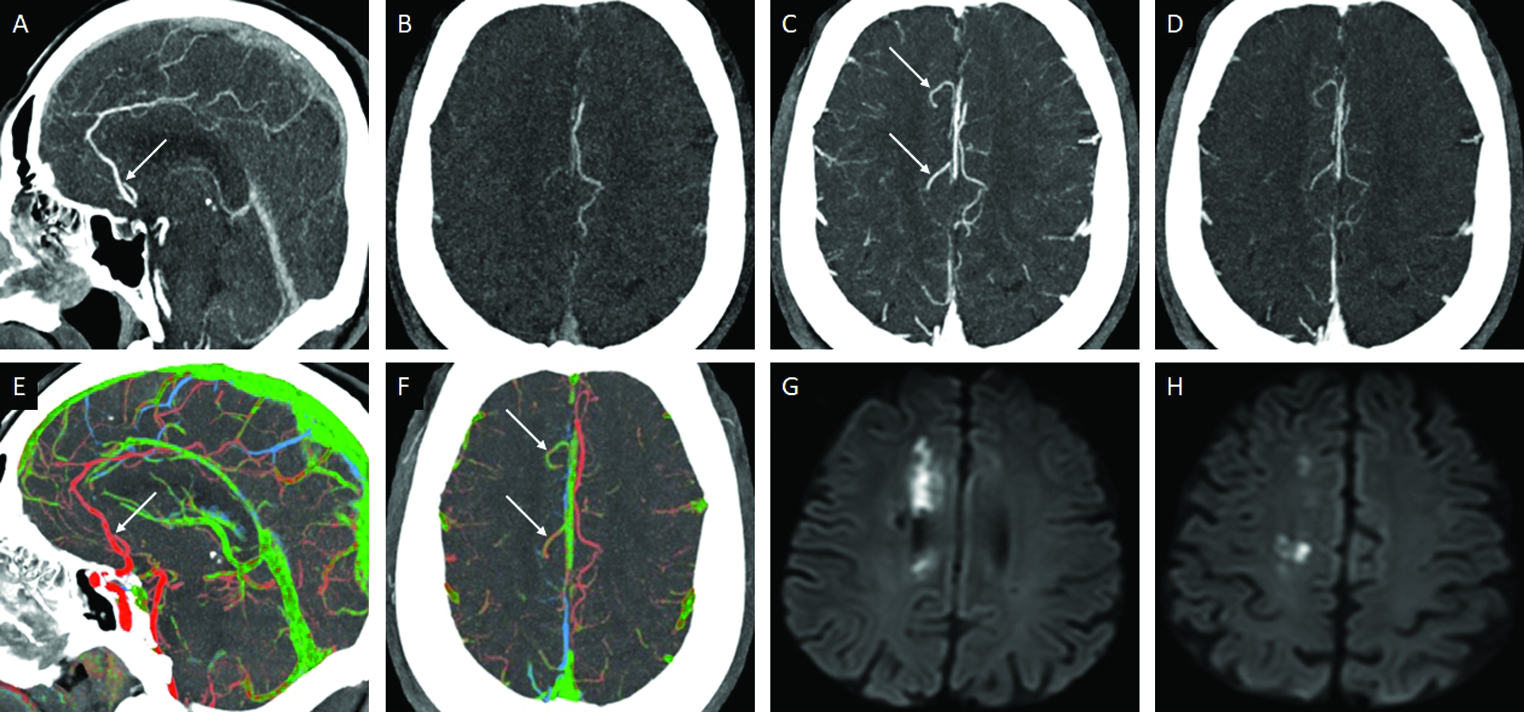
“Intermediate” collateral circulation (score 2): Equal or slightly reduced collaterals, compared to the unaffected hemisphere, but predominantly green colored vessels [Figure 2].
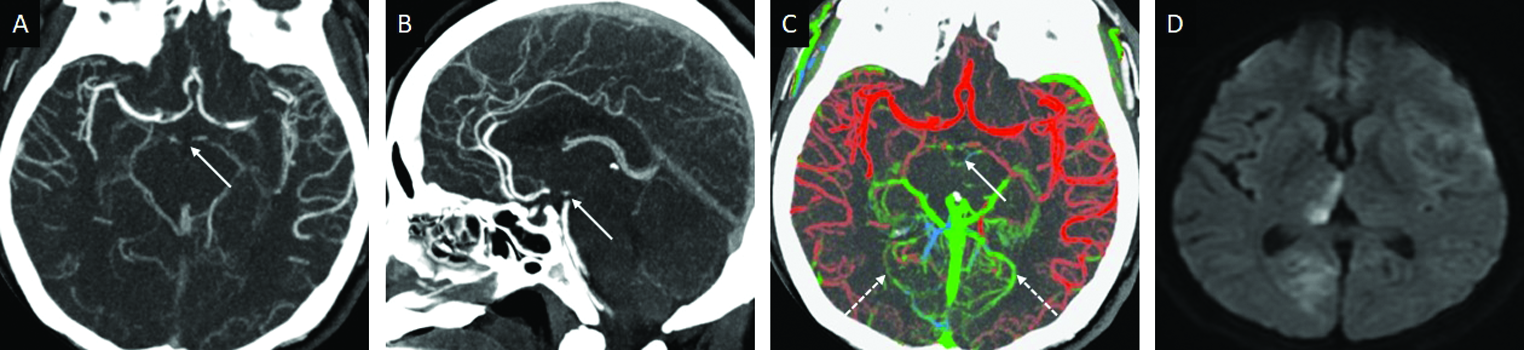
“Poor” collateral circulation (score 1): Significant reduction in the extent of collaterals (even in the presence of few red/green vessels) or if the prevalent color is blue (suggesting significant delay) [Figure 3].
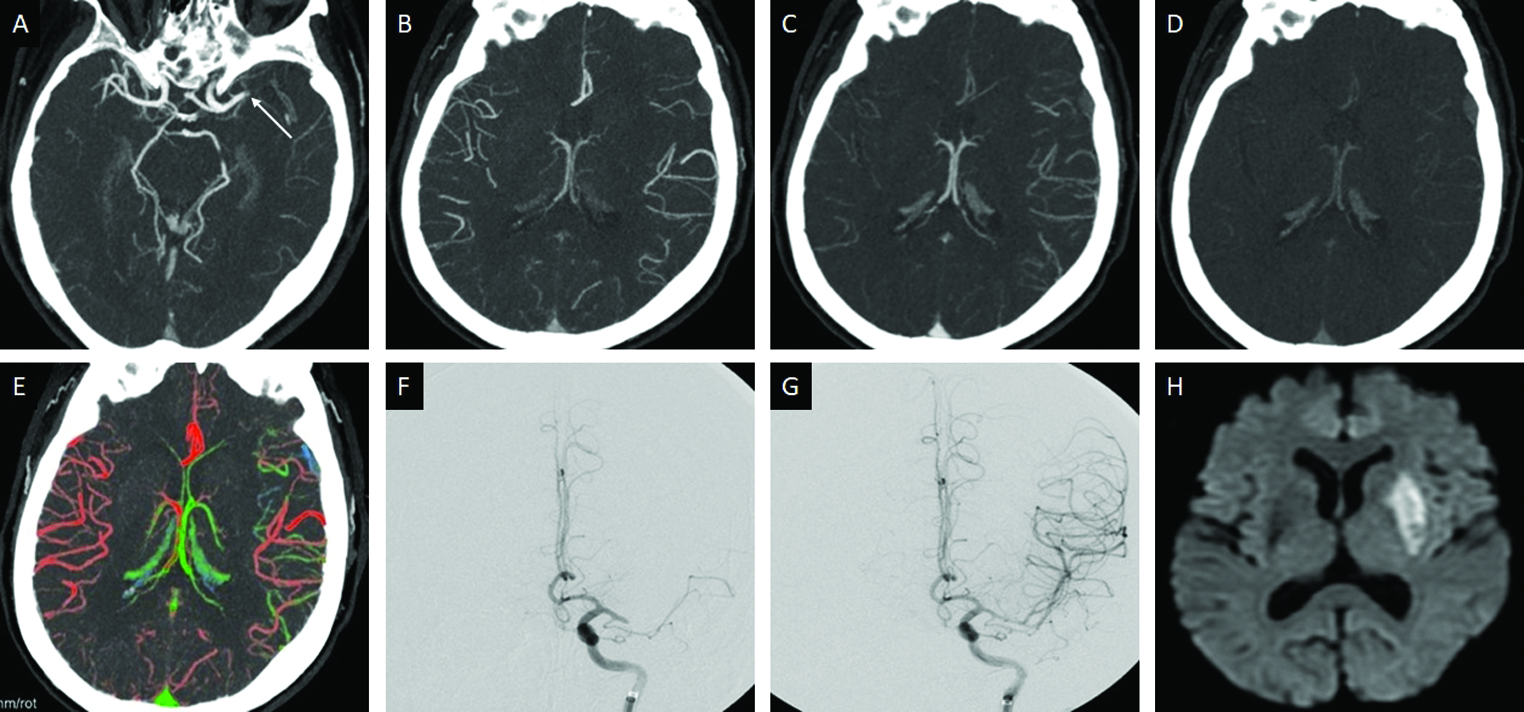
- Grade 3 (good) collaterals in a 69-year-old male patient presenting with acute right hemiplegia. Axial arterial phase MIP-CTA (A), demonstrates thrombo-occlusion (arrow) of the left M1-MCA. Axial MIP images distal to the occlusion in the arterial (B), venous (C), and post-venous (D), phases depict good pial collaterals. Axial ColorViz map (E), reveals red, and few green, colored collaterals. Recombinant tissue plasminogen activator (rTPA) was promptly administered and the patient subsequently underwent successful mechanical thrombectomy (MT) (F,G), 24-hour diffusion weighted imaging (DWI) follow-up (H) shows an acute infarct in the left lentiform nucleus, sparing the left MCA cortex.
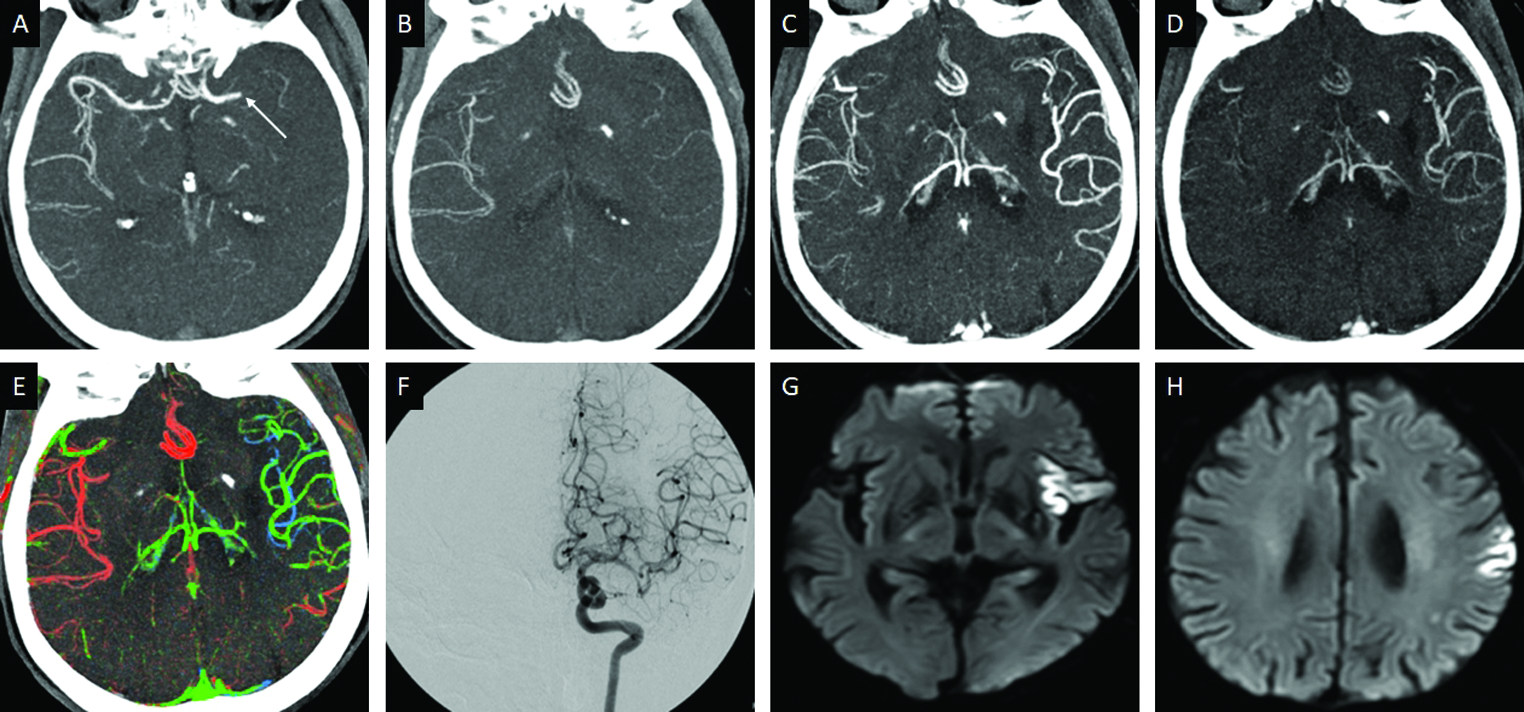
- Grade 2 (intermediate) collaterals in an 81-year-old male patient presenting with acute right hemiplegia and slurring of speech. Axial arterial phase MIP-CTA (A), demonstrates thrombo-occlusion (arrow) of the left M1-MCA. Axial MIP images distal to the occlusion in the arterial (B), venous (C), and post-venous (D), phases demonstrate a 1-phase delay in the appearance of the collateral vessels. Axial ColorViz map (E) reveals predominantly green, and few blue, collaterals. rTPA was administered, leading to recanalization of the left MCA (F), 24-hour DWI follow-up reveals acute infarcts scattered in the left MCA territory (G, H).
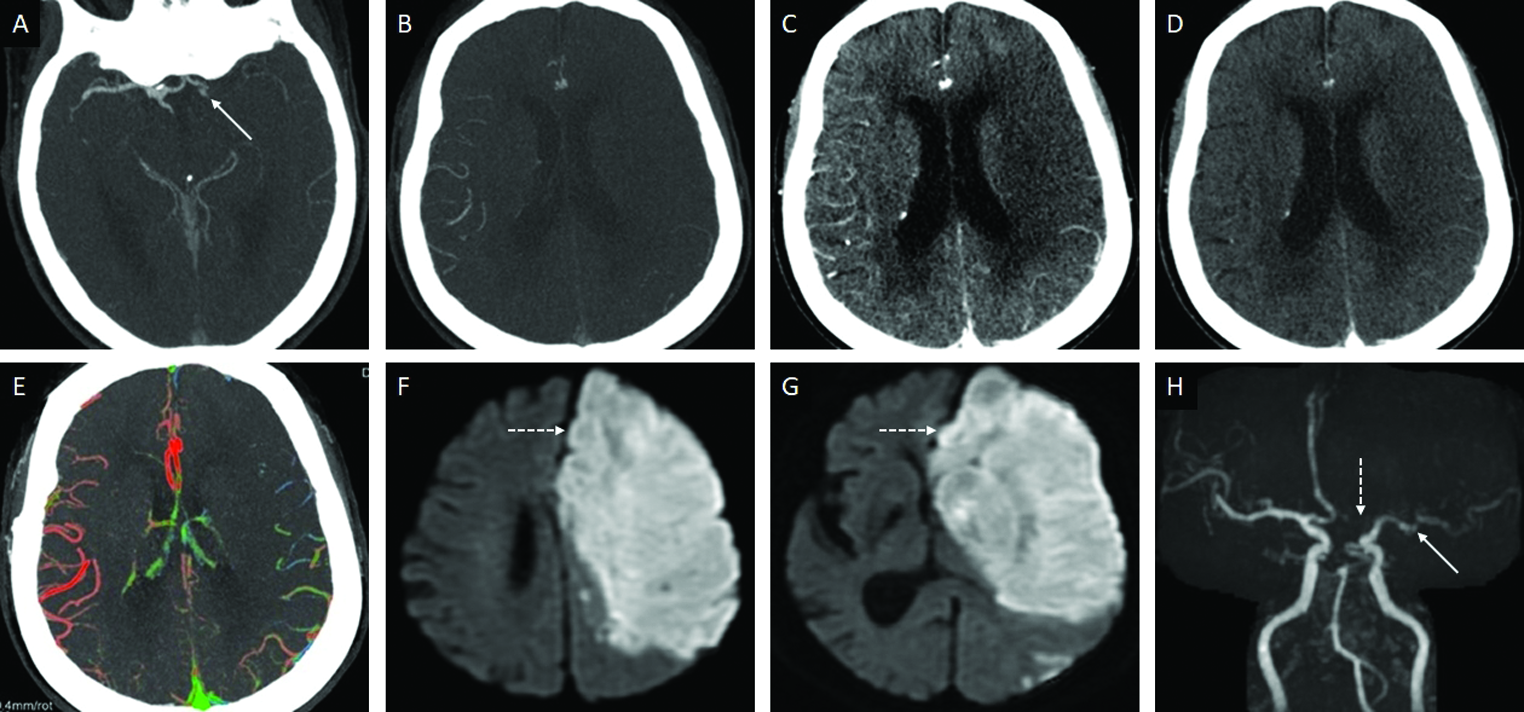
- Grade 1 (poor) collaterals in an 83-year-old female patient presenting with acute left hemispheric syndrome. Axial arterial phase MIP-CTA (A), demonstrates thrombo-occlusion (arrow) of the proximal left M1-MCA. Axial MIP images distal to the occlusion in the arterial (B), venous (C), and post-venous (D), phases demonstrate near complete absence of pial collaterals. Axial ColorViz map (E) confirms sparse collaterals in the left MCA territory. rTPA and MT were not performed in view of the large infarct core with no penumbra on the CTP (not shown). 24-hour DWI follow-up (F, G) confirms an extensive acute infarct involving the left MCA territory. A new acute infarct was also detected in the left ACA territory (dotted arrows). Time-of-Flight MR Angiogram (H) shows interval partial recanalization of the left MCA (arrow) with a new occlusion of the left ACA (dotted arrow).
Using this grading system, Verdolotti et al. found ColorViz to be statistically comparable to mCTA with a good interobserver agreement in the evaluation of collateral circulation.[10] In a retrospective study by Lin et al., a 6-point scoring system, previously proposed by Menon et al., was used for the evaluation of collaterals. They found that color-coded mCTA, using ColorViz, had diagnostic performance equivalent to conventional mCTA, but better than CT Perfusion (CTP), in predicting favorable outcome.[11] In another study to compare the role of mCTA color maps versus conventional mCTA in the prediction of final clinical outcome and infarct volume, Ospel et al. used two trichotomized scales for evaluation of collaterals. Their grading system was an extended version of the scoring used by Verdolotti et al. taking into account collateral extent and collateral filing separately, rather than as a single function. In their study of 285 patients, they found color-coded grading of collateral extent performed similarly to conventional mCTA in predicting 90-day outcome and final infarct volume, but grading for color-coded collateral dynamics did not.[12]
Augmented practice
Color-coded displays have been proven to be beneficial in facilitating visual search and recognition tasks in cerebral vascular pathologies.[4,13] The potential value of colored display, and hence the color indicator effect, of ColorViz can be exploited in identifying medium vessel occlusions (MeVO) and distal cortical branch occlusions of the middle cerebral artery (MCA).[9,11] Such occlusions are difficult to identify, especially in an emergent situation, but are relevant as multiple studies have recognized such occlusions to be amenable to thrombolysis therapy and thrombectomy.[14-17] The imaging hallmark of a distal occlusion is the delayed contrast opacification, beyond the site of occlusion. This appearance has been termed the “delayed vessel sign.”[18] It is attributed to retrograde filling via pial collaterals.[18] On ColorViz, this manifests in green and/or blue [Figures 4 and 5].[9,11] Lin et al. found that ColorViz may increase the speed and accuracy of detection of MeVO, which could not be sensitively detected on conventional mCTA images.[11]
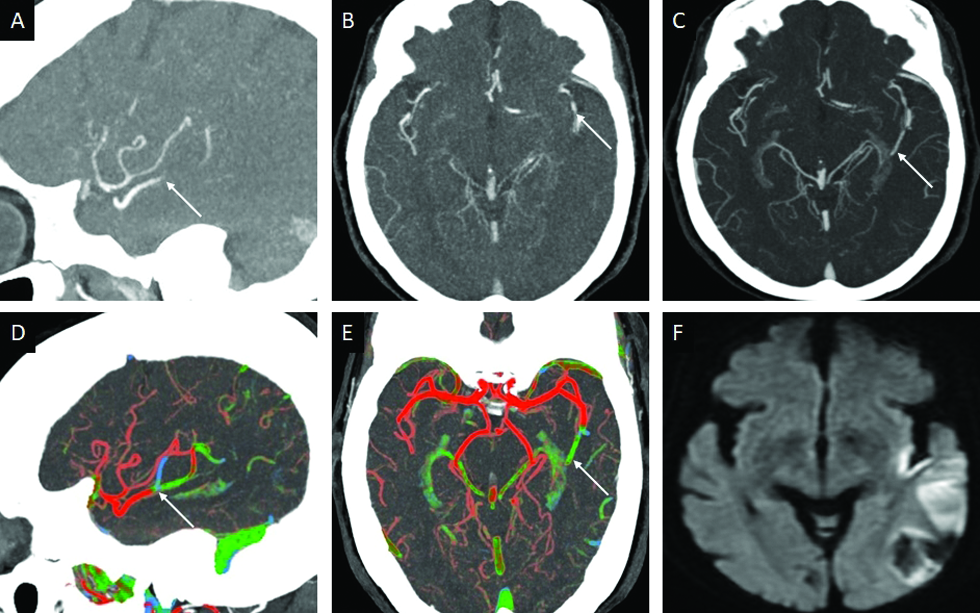
- Left M2-MCA occlusion (MeVO) in an 80-year-old female patient presenting with a fall subsequent to acute right hemiplegia. Sagittal (A) and axial (B) arterial phase MIP-CTA images demonstrate thrombo-occlusion of the inferior division of the left MCA (arrow). Axial MIP images obtained in the venous (C) phase demonstrate preserved opacification beyond the occlusion (arrow) in keeping with the “delayed vessel sign.” Sagittal (D) and axial (E) ColorViz maps show an abrupt change in color (arrow) along the occluded left M2-MCA from red to green-blue. 24-hour DWI follow-up (F) confirms an acute infarct involving the posterior left insular cortex and left M3 region.
- Distal M4 occlusion in a 77-year-old male patient presenting with the right pure motor syndrome. No LVO or MeVO was detected. Axial MIP-CTA images obtained in the arterial (A), venous (B), and postvenous (C) phases show delayed opacification (arrow in B) and washout (arrow in C) in one of the peri-Rolandic M4-MCA branches. Axial ColorViz maps (D, E) demonstrate corresponding blue-green color (arrow). The color-indicator effect of ColorViz helped in identifying the hemodynamic alteration and rTPA was administered. 24-hour DWI follow-up (F) confirms an acute infarct (arrow) in the left precentral gyrus, corresponding to the site of presumed occlusion.
The visual impact of color may be extended to the identification of anterior cerebral artery (ACA) occlusion.[9] ACA occlusions are rare and pose a challenge clinically (due to their atypical presentation) as well as radiologically (due to the primary focus on the MCA circulation in AIS).[19] CTP may show perfusion delays in the affected ACA territories which would guide inexperienced readers. However, adequate coverage of the ACA territory is necessary for diagnosis; limited coverage, with the imaging slab often placed at the ganglionic level (as in most older CT scanners), is known to limit the evaluation of the ACA territory.[9,19] Clue to identify an ACA occlusion lies in the lack of symmetric opacification, and hence differences in color, of pericallosal arteries on axial images [Figure 6].[9,19] Though there still remains a lack of high-level evidence from a randomized trial to prove the benefit of EVT in ACA occlusions, continued strategies to improve techniques and thrombectomy devices would soon warrant accurate and precise localization of ACA occlusions for prompt EVT.[19]
- Occlusion of the A2-ACA in a 67-year-old patient presenting with acute left lower limb numbness and weakness. Sagittal arterial phase MIP-CTA image (A) shows thrombo-occlusion of the right A2-ACA segment (arrow). Axial MIP images obtained distal to the site of occlusion in the arterial (B), venous (C) and postvenous (D) phases show delayed distal filling within the cortical branches of the right ACA (arrows in C, D). Sagittal (E) and axial (F) ColorViz maps confirm the site of occlusion (arrow in E) and enable the easy identification of the delayed distal filling (arrow in F). The patient promptly received rTPA. 24-hour DWI follow-up (G, H) confirms multiple acute infarcts scattered in the right ACA territory.
Another potential role of ColorViz is the identification of occlusions of the posterior circulation, including the vertebrobasilar system [Figure 7].[9] Infarcts in the posterior fossa are difficult to identify on unenhanced CT scans and CTP evaluation may be limited due to artifacts from the skull base.[9,20] mCTA, being less susceptible to artifacts as compared to CTP, remains an important tool in identifying posterior circulation occlusions.[9] However, it must be acknowledged that further characterization of collateral status in posterior circulation stroke, except for those of the posterior cerebral artery (PCA), is still not established given its variable vascular anatomy and poorly understood pial collateral supply.[7,8]
- Top of basilar occlusion in a 49-year-old patient with acute loss of consciousness. Axial (A) and sagittal (B) arterial phase MIP-CTA image demonstrate the basilar occlusion (arrows). Axial (C) ColorViz maps confirm the occlusion (arrow) and absent red-colored arteries distally in the PCA territories (dotted arrows). The patient underwent EVT. 24-hour DWI follow up (D) reveals acute infarcts involving the right PCA territory.
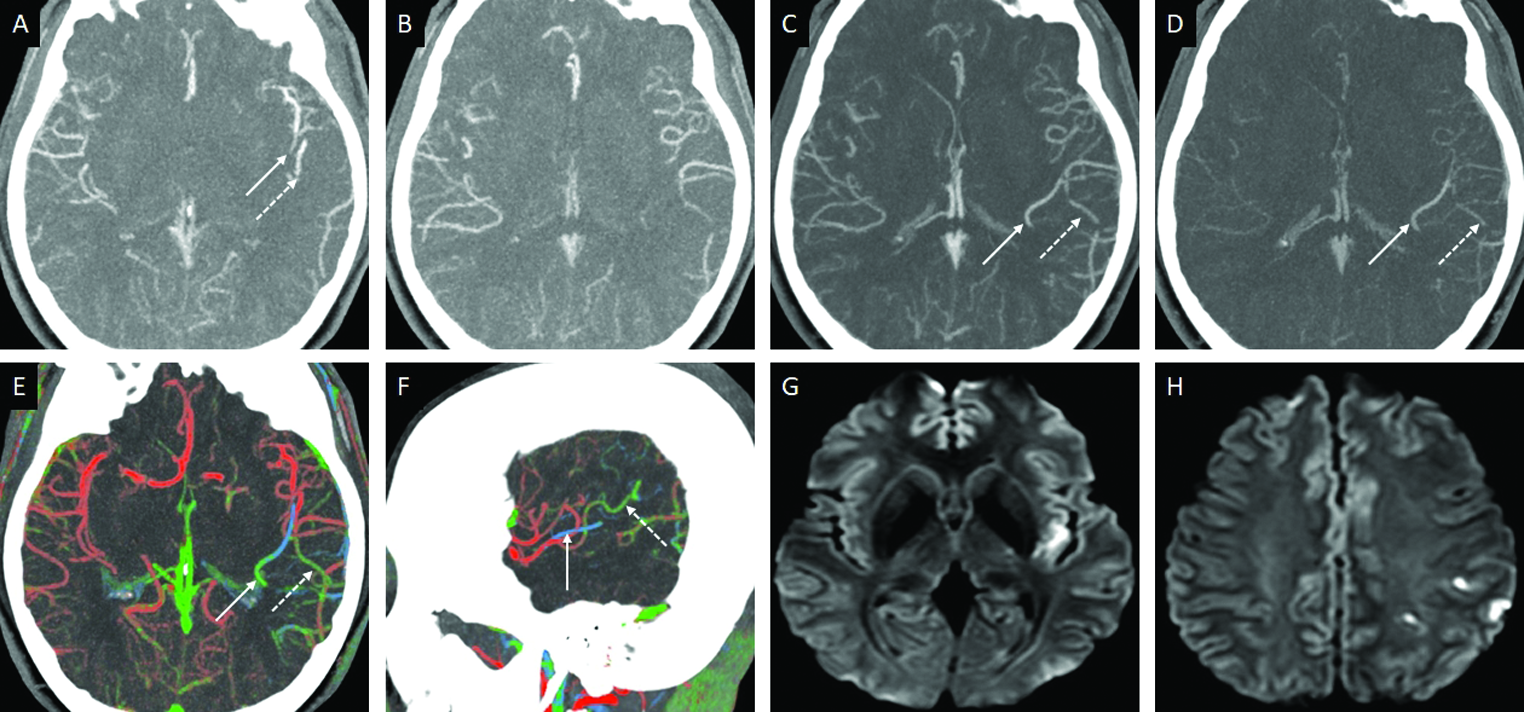
A proposed use of the color-indicator effect of ColorViz is in the identification of multivessel occlusions (MVO) in downstream or different vascular territories [Figures 8 and 9].[9] In a study on 720 patients with large vessel occlusion (LVO) subjected to endovascular therapy, MVO was found in 10.7% of patients, however, MVO was only prospectively identified in 54.5% cases.[21] The presence of MVO may impact treatment decisions, angiographic success, and clinical outcomes.[21] While most studies so far evaluate ColorViz in anterior circulation LVO, it does seem to show promise in MVO detection as well.[9] Such an extended application of ColorViz would need validation with more prospective studies.
- Downstream MVO in a 37-year-old male patient presenting with acute right facial droop. Axial arterial phase MIP-CTA image (A) demonstrates thrombo-occlusion of superior (arrow) and inferior (dotted arrow) divisions of the left MCA. Axial MIP images obtained in the arterial (B), venous (C), and postvenous (D) phases, depict a “delayed vessel sign” distal to the sites of occlusion (C,D). Axial (E) and sagittal (F) ColorViz maps help in easy identification of the MVO characterized by an abrupt change in color from red to green-blue. 24-hour DWI follow-up (G,H) reveals an incomplete left MCA territory infarct involving the posterior insular cortex (G) and the left parietal cortices (H).
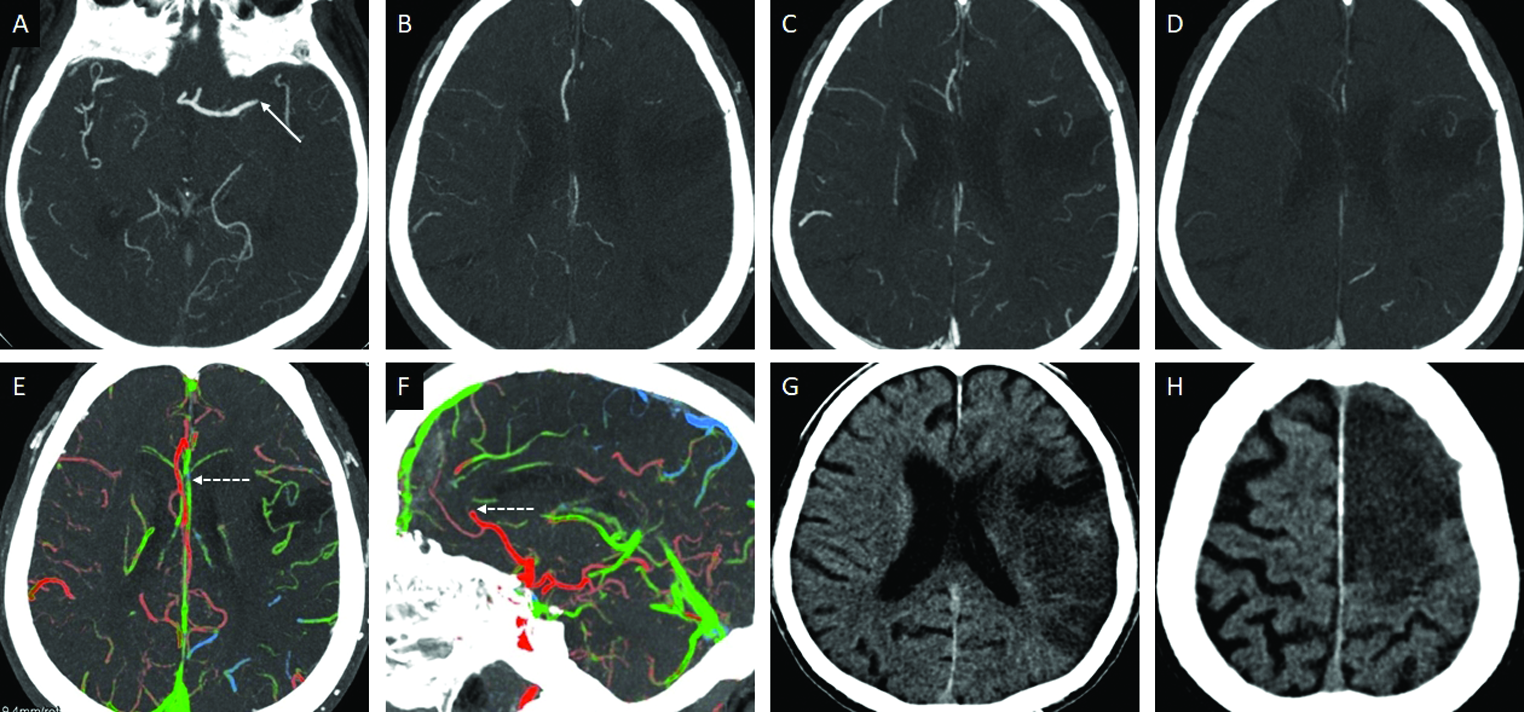
- Multiterritorial MVO in a 74-year-old patient presenting with left hemispheric syndrome. Axial arterial phase MIP-CTA image (A) demonstrates thrombo-occlusion of the left M1-MCA (arrow). Axial MIP images obtained distal to the site of occlusion in the arterial (B), venous (C) and postvenous (D) phases demonstrate a 1-phase delay in the appearance of the collateral vessels. Axial ColorViz map (E) shows intermediate left MCA pial collaterals, with predominant green collaterals, however, of note there is impaired filling in the left ACA territory (dotted arrow). Sagittal ColorViz map (F) confirms occlusion of the pericallosal branch of the left ACA (dotted arrow). The color indicator effect of ColorViz helped identify both the occlusions, which was retrospectively confirmed on the mCTA. Follow up CT (G,H) confirms an acute infarct involving the left MCA and ACA territories.
LIMITATIONS
ColorViz seems to be promising, but its role in clinical practice still needs to be validated using large-scale prospective clinical trials. The limited published studies so far have been retrospective in nature and have not put ColorViz to the test in an emergent setting of AIS. The true utility of ColorViz in clinical practice would need a prospective, multicentric clinical trials. Moreover, its use in posterior circulation stroke and MVO has been speculated, but not proven. The current FastStroke software does not allow manual change of the color-coding system as per the comfort of the operator. This may be confusing for some who are comfortable with a different color scheme.[12]
Adequate evaluation of occlusion relies on the asymmetry between the affected and affected vascular territory. Since the standard of comparison of pial collaterals is based on the assumption that the contralateral side is unaffected, bilateral occlusions may confound interpretation or even result in a missed occlusion.[9] Global or unilateral delayed arterial opacification due to conditions such as congestive heart failure and proximal critical stenosis, respectively, may cause erroneous interpretation of an occlusion or collateral status based on the prevalence of green and/or blue-colored arteries.[7,9]
CONCLUSION
The automatic synchronization of all mCTA phases, using FastStroke, and subsequent depiction in a color-coded, single composite view (ColorViz) reduces the time for post-processing and evaluation of mCTA. ColorViz is a powerful addition to stroke workflow enabling quick, intuitive evaluation of pial collaterals. Additionally, its promising potential in the identification of MeVO and MVO as well as posterior circulation occlusions would make it a valuable asset, especially for inexperienced radiologists.
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Acute stroke: Prognostic value of quantitative collateral assessment at perfusion CT. Radiology. 2019;290:760-8.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for evaluation and management of cerebral collateral circulation in ischaemic stroke 2017. Stroke Vasc Neurol. 2018;3:117-30.
- [CrossRef] [PubMed] [Google Scholar]
- Color-coded cerebral computed tomographic angiography: Implementation of a convolution-based algorithm and first clinical evaluation in patients with acute ischemic stroke. Invest Radiol. 2015;50:361-5.
- [CrossRef] [PubMed] [Google Scholar]
- CT protocol for acute stroke: Tips and tricks for general radiologists. Radiographics. 2008;28:1673-87.
- [CrossRef] [PubMed] [Google Scholar]
- CTA-for-all: Impact of emergency computed tomographic angiography for all patients with stroke presenting within 24 hours of onset. Stroke. 2020;51:331-4.
- [CrossRef] [PubMed] [Google Scholar]
- Multiphase CT angiography: A new tool for the imaging triage of patients with acute ischemic stroke. Radiology. 2015;275:510-20.
- [CrossRef] [PubMed] [Google Scholar]
- Multiphase CT angiography: A useful technique in acute stroke imaging—collaterals and beyond. AJNR Am J Neuroradiol. 2020;42:221-7.
- [CrossRef] [PubMed] [Google Scholar]
- Displaying Multiphase CT Angiography Using a Time-Variant Color Map: Practical Considerations and Potential Applications in Patients with Acute Stroke. AJNR Am J Neuroradiol. 2020;41:200-5.
- [CrossRef] [PubMed] [Google Scholar]
- ColorViz, a new and rapid tool for assessing collateral circulation during stroke. Brain Sci. 2020;10:882.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive value of time-variant color-coded multiphase CT angiography (mCTA) regarding clinical outcome of acute ischemic stroke: In comparison with conventional mCTA and CT perfusion. Acta Radiol. 2022;63:84-92.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of time-variant multiphase CTA color maps in outcome prediction for acute ischemic stroke due to anterior circulation large vessel occlusion. Clin Neuroradiol. 2021;31:783-90.
- [CrossRef] [PubMed] [Google Scholar]
- Parametric Color Coding of Digital Subtraction Angiography. AJNR Am J Neuroradiol. 2010;31:919-24.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of CTA evaluations in daily clinical practice for large and medium vessel occlusion detection in suspected stroke patients. Eur Stroke J. 2021;6:357-66.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical course of acute ischemic stroke due to medium vessel occlusion with and without intravenous alteplase treatment. Stroke. 2020;51:3232-40.
- [CrossRef] [PubMed] [Google Scholar]
- A review of endovascular treatment for medium vessel occlusion stroke. J NeuroIntervent Surg. 2021;13:623-30.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical thrombectomy in medium vessel occlusions. Stroke. 2020;51:3224-31.
- [CrossRef] [PubMed] [Google Scholar]
- Improved detection of anterior circulation occlusions: The “delayed vessel sign” on multiphase CT angiography. AJNR Am J Neuroradiol. 2017;38:1911-6.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular treatment of anterior cerebral artery occlusions. J NeuroIntervent Surg. 2021;13:1007-11.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of CT perfusion in the setting of cerebral ischemia: Patterns and pitfalls. AJNR Am J Neuroradiol. 2010;31:1552-1563.
- [CrossRef] [PubMed] [Google Scholar]
- Multivessel occlusion in patients subjected to thrombectomy: Prevalence, associated factors, and clinical implications. Stroke. 2018;49:1355-62.
- [CrossRef] [PubMed] [Google Scholar]







