Translate this page into:
Plain X-ray findings of post sleeve gastrectomy gastric leak

*Corresponding author: Sultan R Alharbi, Department of Radiology and Medical Imaging, College of Medicine, King Saud University, Riyadh, Saudi Arabia. drsultan000@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Alharbi SR. Plain X-ray findings of post sleeve gastrectomy gastric leak. J Clin Imaging Sci 2022;12:28.
Abstract
Gastric leak following sleeve gastrectomy (SG) is a rare but significant cause of morbidity and mortality. A high clinical index of suspicion is the most sensitive approach to detect gastric leaks. Computed tomography (CT) is the gold standard diagnostic technique, although it might not be performed due to unavailability, and the inability to image superobese patients due to limited CT gantry space. Early detection and management are critical for attaining a better prognosis.
The following pictorial review discusses the various plain X-ray radiographic findings that indicate a gastric leak. These findings may be overlooked, however, they remain valuable in patients with clinically suspected gastric leaks. This pictorial review illustrates the spectrum of findings related to post-SG gastric leak encountered in plain X-ray radiography.
Keywords
Sleeve gastrectomy
Gastric leak
Plain radiograph
X-ray chest
X-ray abdomen
INTRODUCTION
Sleeve gastrectomy (SG) is the most common type of obesity surgery worldwide. Post-SG gastric leak is a rare but fatal complication that is challenging to diagnose and manage. Early diagnosis and management lead to a better prognosis. Late diagnosis and management can lead to chronic difficulties in healing fistulas, and sepsis that may result in septic shock and even death.[1,2]
Post-sleeve gastrectomy gastric leak commonly occurs at the gastroesophageal junction. This gastric leak causes an inflammatory process mostly seen in the left subphrenic area near the most common site of a gastric leak. This unique location causes variable symptoms in the patient, including chest and upper abdominal symptoms.[1,3] Majority of patients develop intermediate (3-14 days) to late (more than 14 days) postoperative gastric leak (98.75%). Early gastric leak constitutes only 1.25% of the reported postoperative gastric leak.[1] For that reason, intraoperative tests like gas or methylene blue tests are negative. Similarly, early routine postoperative radiology examinations like early CT and upper gastrointestinal contrast fluoroscopy on the first and second postoperative days are almost always negative.[3,4]
The most used imaging examinations for symptomatic suspected gastric leak patients are upper gastrointestinal contrast fluoroscopy study and CT. Plain radiography is believed to be of limited value in the detection of post sleeve gastrectomy gastric leak.[5,6] CT is considered the gold standard diagnostic tool, whereas upper gastrointestinal contrast fluoroscopy studies have a high false-negative rate. Although CT is the gold standard, it might not be available at some centers, and it can’t accommodate superobese patients due to limited CT gantry space.[4-6]
Plain radiography has been a well-known screening examination for several years in medical practice due to its availability, speed, low cost, and low radiation dose. It is the most requested radiological investigation in the emergency department for acute abdomen requiring admission. The American College of Radiology (ACR) guidelines for plain radiography indications include the evaluation of pneumoperitoneum and follow-up of postoperative patients.[7]
METHOD
A retrospective review of 88 patients with post-SG gastric leak based on CT diagnosis was conducted. The median date of presentation was 13 postoperative days ranging from 5-62 postoperative days. Most patients presented with suspected clinical gastric leak post-SG underwent plain radiography of the abdomen or chest as an initial evaluation. These radiographs were retrospectively evaluated in correlation with the CT abdominal examination and revealed abnormal findings in most radiographs.
In this pictorial review, we illustrate the plain X-ray radiographic findings in correlation with the CT abdominal findings commonly seen in patients with post-SG leaks [Table 1].
| Abdominal findings | Chest findings |
|---|---|
| Free air under the diaphragm | Left pleural effusion |
| Localized air under the left diaphragm | Elevated left diaphragm |
| Left basal lung consolidation/collapse |
Normal radiograph
Following sleeve gastrectomy, abdominal X-ray radiograph shows a stapler line of hyperdense surgical material and absence of gastric fundus gas bubble [Figure 1]. Chest radiography showed unremarkable findings. Pleural effusion and lung consolidation or collapse are not expected postoperatively [Figures 2].
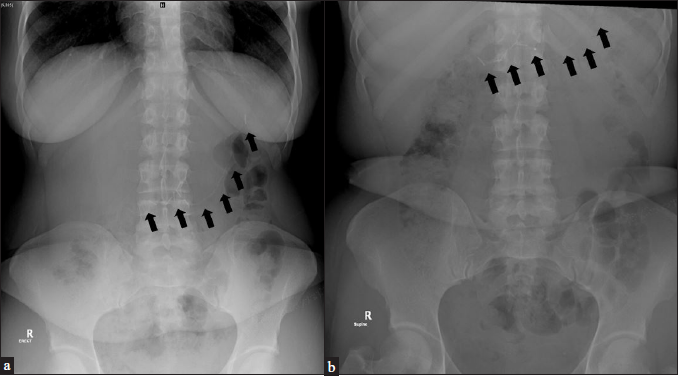
- (a) A 29-year-old female patient status post sleeve gastrectomy day 21. Abdominal radiographs erect showing postoperative radiopaque surgical materials (black arrows). (b) Abdominal radiographs supine showing postoperative radiopaque surgical materials (black arrows).

- (a) A 36-year-old male patient status post sleeve gastrectomyday four. Chest radiograph presurgery showing normal findings. (b) Chest radiograph postsurgery showing radiopaque surgical clips (black arrow). Note lack of gastric fundus gas bubble.
Free air under the diaphragm
As with most viscous perforation, post-SG gastric leaks can lead to pneumoperitoneum, which appears as free air under the diaphragm on chest or abdomen X-ray radiographs [Figure 3].[5]

- (a) A 37-year-old female patient status post sleeve gastrectomy day five presented with abdominal pain. Frontal chest radiograph showing free air under the right diaphragm (black arrow). (b) Erect abdominal radiograph showing free air under both diaphragms (black arrow). (c) Enhanced axial CT abdomen showing gastric leak with free air around the gastric remnant and around the liver.
Localized air under the left diaphragm (pseudo gastric bubble sign)
Gastric leaks following SG can be localized and appear as localized air pockets under the left diaphragm mimicking gastric fundus bubbles (pseudo gastric bubble sign) [Figures 4 and 5].[6]

- (a) A 40-year-old female patient status post sleeve gastrectomy day eight presented with vomiting and abdominal pain. Frontal chest radiograph showing localized pocket of air with air/fluid level at left sub diaphragm (black arrow). (b) Abdominal radiograph showing localized pocket of air with air/fluid level at left sub diaphragm (black arrow). (c) Coronal CT abdomen showing large air collection at left sub diaphragm indicating gastric leaks.

- (a) A 33-year-old male patient status post sleeve gastrectomy day 11 presented with tachycardia. Frontal chest radiograph showing localized pocket of air with air/fluid level at left sub diaphragm mimicking gastric fundus gas (black arrow). (b) Enhanced axial CT abdomen showing large perigastric collection with air/fluid level indicating gastric leaks.
Elevated left diaphragm
Gastric content leakage causes an inflammatory reaction that leads to phlegmon or abscess formation commonly seen in the left subphrenic area. The left hemidiaphragm can be elevated secondary to the subphrenic phlegmon reaction, localized peritonitis, and abscess [Figure 6].[8]

- (a) A 30-year-old male patient status post sleeve gastrectomy day seven presented with chest pain. Lateral chest radiograph showing elevated hemidiaphragm (black arrow). (b) Coronal enhanced CT abdomen showing elevated left hemidiaphragm and mesenteric fast stranding and infiltration at the subphrenic area.
Left pleural effusion
Left pleural effusion is the most common chest complication following SG, and it is highly associated with postoperative complications, especially gastric leaks. It is usually mild, appearing as blunting of the costophrenic angle [Figure 7].[9]

- (a) A 36-year-old female patient status post sleeve gastrectomy day eight presented with vomiting. Frontal chest radiograph showing blunting of left costophrenic angle (black arrow) indicating pleural effusion. (b) Lateral chest radiograph showing blunting of costophrenic angle (black arrow). (c) Enhanced sagittal CT abdomen showing pleural effusion (black arrow) and subphrenic collection.
Left basal consolidation/collapse
Left subphrenic collection and abscess formation secondary to gastric leak can cause irritation to the diaphragm or erosion and extension into the left pleural cavity or lung, appearing as left lung basal consolidation or atelectasis [Figures 8 and 9].[10]

- (a) A 26-year-old male patient status post sleeve gastrectomy day ten presented with upper abdominal and chest pain. Frontal chest radiograph showing left lung basal consolidation (white arrow), pleural effusion, and localized air pocket in the subphrenic area (black arrow). (b) Axial CT abdomen showing large perigastric collection with air/fluid level indicating gastric leaks. (c) Axial CT chest showing left pleural effusion with basal lung consolidation.

- (a) A 29-year-old female patient status post sleeve gastrectomy day 60 presented with cough. Frontal chest radiograph showing left basal lung consolidation (white arrow). (b) Enhanced coronal CT abdomen showing gastropleural fistula (white arrow). (c) Enhanced coronal CT chest showing gastropleural fistula with left lung basal consolidation.
Plain X-ray radiograph of abdomen and chest can show findings of post sleeve gastrectomy intermediate to late gastric leak. This illustration may help radiologists and physicians to be familiar with different radiological findings. There is a potential role of plain X-ray to be used as a screening test for asymptomatic patients on fifth to ten postoperative days to detect intermediate gastric leaks that need further research to validate it.
CONCLUSION
We illustrated multiple plain radiographic findings associated with post-SG gastric leaks in this pictorial essay that can be seen in the initial evaluation [Figure 10]. These findings may aid in the detection and stratification of patients before definite diagnosis using CT or upper gastrointestinal contrast fluoroscopy study.
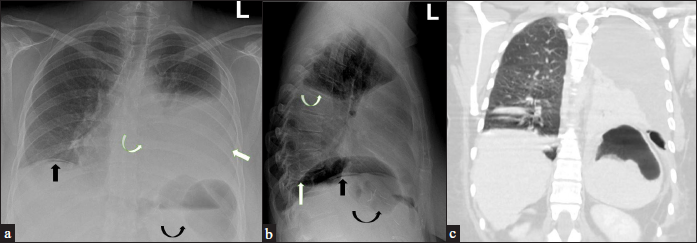
- (a) A 44-year-old female patient status post sleeve gastrectomy day nine presented with chest pain vomiting, and tachycardia. Frontal chest radiograph showing free air under the right diaphragm (black arrow), left subphrenic localized air pockets (curved black arrow), left pleural effusion (white arrow), and left basal lung consolidation (curved white arrow). (b) Lateral chest radiograph showing free air under the diaphragm (black arrow), localized air pocket under the diaphragm (curved black arrow), elevated hemidiaphragm (white arrow), and pleural effusion (curved white arrow). (c) Coronal CT chest showing left pleural effusion, left basal lung collapse/consolidation, left subphrenic large air pocket, and elevated left diaphragm.
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Challenges in the diagnosis of leak after sleeve gastrectomy: Clinical presentation, laboratory, and radiological findings. Obes Surg. 2021;31:612-6.
- [CrossRef] [PubMed] [Google Scholar]
- Management of leak after sleeve gastrectomy: Outcomes of 73 cases, treatment algorithm and predictors of resolution. Obes Surg. ;2020Obes Surg. ;30:515-20.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous CT-guided drainage of gastric leaks post-sleeve gastrectomy. Open J Radiol. 2020;10:1.
- [CrossRef] [Google Scholar]
- Prospective evaluation of routine early computed tomography scanner in laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12:1483-90.
- [CrossRef] [PubMed] [Google Scholar]
- Laparoscopic sleeve gastrectomy: A radiological guide to common postsurgical failure. Can Assoc Radiol J. 2018;69:184-96.
- [CrossRef] [PubMed] [Google Scholar]
- Computed tomography-based diagnosis of post-laparoscopic sleeve gastrectomy gastric leak. J Clin Imaging Sci. 2020;10:8.
- [CrossRef] [PubMed] [Google Scholar]
- ACR-SPR practice guideline for the performance of abdominal radiography. Available from: http://www.acr.org/-/media/ACR/Files/Practice-Parameters/radabd.pdf?la=en
- Elevated right hemidiaphragm: A clue in acute cholecystitis? Cureus. 2021;13:e14571.
- [CrossRef] [PubMed] [Google Scholar]
- Can left pleural effusion be an indicator of gastric leaks after laparoscopic sleeve gastrectomy? Open J Radiol. 2021;11:11-8.
- [CrossRef] [Google Scholar]
- When is pneumonia not pneumonia? BMJ Case Rep. 2015;2015:bcr2014207588.
- [CrossRef] [PubMed] [Google Scholar]






