Translate this page into:
Percutaneous n-butyl cyanoacrylate glue embolization combined with arterial embolization for extracranial arteriovenous malformations

*Corresponding author: Jie-Sheng Qian, Department of Vascular Surgery, The Third Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China. qjsyf@163.com
-
Received: ,
Accepted: ,
How to cite this article: Tong YC, Zhao Y, He HP, Lin R, Lv JB, Zhang YB, et al. Percutaneous n-butyl cyanoacrylate glue embolization combined with arterial embolization for extracranial arteriovenous malformations. J Clin Imaging Sci. 2025;15:19. doi: 10.25259/JCIS_33_2025
Abstract
Objectives:
Congenital arteriovenous malformations (AVMs) are characterized by abnormal connections between arteries and veins, often presenting challenges in treatment due to their complex vascular structure. Endovascular therapies, including embolization techniques, have become integral in managing AVMs, yet optimal treatment strategies remain under investigation. This retrospective study aimed to evaluate the safety and efficacy of percutaneous glue embolization of n-butyl cyanoacrylate (nBCA) combined with arterial embolization in treating extracranial AVMs.
Material and Methods:
This retrospective study included 11 patients with extracranial AVMs who underwent percutaneous injection of nBCA glue embolization combined with arterial embolization at our institution between May 2015 and October 2023. Angiographic classification was performed using the Cho-Do vascular imaging system and the Schobinger classification system to categorize the AVMs. Treatment efficacy was assessed based on the percentage of vessel occlusion observed in angiography or imaging studies. The occurrence of major and minor complications was also evaluated.
Results:
Eleven patients received 16 treatments, involving a combination of arterial and percutaneous embolization techniques. Five cases achieved complete recovery, while four cases showed significant improvement, resulting in an overall treatment success rate of 81.8%. Favorable outcomes were observed in terms of symptom alleviation and lesion occlusion. Adverse events were minimal, with transient pain and edema being the most common postoperative complaints. Only one case of mild post-operative complication occurred.
Conclusion:
Percutaneous glue embolization combined with arterial embolization proves to be a safe and effective treatment modality for extracranial AVMs, with acceptable rates of complications and favorable treatment outcomes.
Keywords
Arteriovenous malformations
Embolization
n-butyl cyanoacrylate
Percutaneous
INTRODUCTION
Congenital arteriovenous malformations (AVMs) are a form of high-flow vascular malformations characterized by underdeveloped arteries and veins directly interconnected through a convoluted vascular mass termed the “nidus.”[1] AVMs can be classified into central and peripheral types, with the head and neck representing the most common sites for peripheral AVMs,[2] followed by the limbs. Symptoms vary depending on the location and size of the lesion, including pain, swelling, skin discoloration, pulsatile masses, ulceration, bleeding, and necrosis.[3] In massive AVMs, direct arterial blood flow into the venous system can lead to increased cardiac pre-load and subsequent heart failure.[4] According to the Schobinger classification, AVMs can be divided into four stages based on clinical symptoms: Quiescence (Stage I), expansion (Stage II), destruction (Stage III), and decompensation (Stage IV).[5] Advancement to higher stages indicates more severe clinical symptoms and typically necessitates more intricate clinical management.
Resecting AVMs surgically presents challenges, including achieving complete excision for larger lesions, the risk of recurrence, intraoperative hemorrhage, and potential damage to surrounding structures.[6,7] Endovascular therapy employing diverse embolic agents and sclerosants has emerged as a principal treatment modality for AVMs.[8,9] Among these, an extensively used embolic agent is absolute ethanol, which has demonstrated superior efficacy compared to other embolic materials in numerous studies.[10,11] The complete cure rate of AVMs with ethanol embolization ranges from 40% to 88%.[4] However, the use of absolute ethanol is associated with a high incidence of complications, with an overall complication rate ranging from 10% to 52%.[12] In addition to absolute ethanol, other commonly used embolic materials include liquid embolic agents such as n-butyl cyanoacrylate (nBCA),[13] Onyx,[14] particulate embolic agents like polyvinyl alcohol (PVA) embolic particles,[15] and detachable coils.[16]
Arterial embolization using nBCA, also known as tissue glue embolization, is frequently employed in the clinical management of AVMs.[17] However, relying solely on nBCA may not always achieve complete occlusion of AVMs, particularly in cases involving multiple feeding arteries and draining veins,[18] often leading to incomplete occlusion and subsequent recurrence.[19]
When arterial access poses challenges or complete occlusion cannot be achieved via arterial approaches, percutaneous puncture approaches serve as valuable alternatives.[20] Percutaneous injection of ethanol via catheter or needle puncture has shown promising outcomes but is associated with an increased risk of complications.[5,21] Combining arterial embolization with nBCA and percutaneous sclerotherapy using ethyl oleate has been reported as a safe and effective treatment method with an acceptable risk profile.[22] Similarly, PVA embolization combined with nBCA arterial embolization has shown promising results for extracranial AVMs with an acceptable rate of complications.[17]
Percutaneous injection of nBCA has demonstrated pathological success in embolizing AVMs,[23,24] venous malformations,[25] and pseudoaneurysms[26] in various patient populations. However, clinical studies specifically focused on percutaneous nBCA glue embolization therapy remain relatively limited, particularly in China. Therefore, this study aimed to evaluate the safety and efficacy of percutaneous glue embolization of nBCA combined with arterial embolization in the treatment of extracranial AVMs.
MATERIAL AND METHODS
Study population
This was a retrospective study conducted on all patients with AVMs who received treatment involving percutaneous injection of tissue glue embolization, either with or without adjunctive arterial embolization, at our institution between May 2015 and October 2023.
All enrolled patients underwent at least one embolization treatment. Exclusion criteria included other types of vascular malformations such as vascular tumors, venous malformations, and patients who did not undergo percutaneous injection of tissue glue embolization treatment.
The diagnosis of AVMs was established through a combination of clinical history, physical examination, and imaging studies including magnetic resonance imaging, computed tomography, and duplex ultrasonography.
The data collected included patients’ medical records such as demographic data, pre-operative imaging studies, details of all embolic agents and embolization approaches used during surgery, post-operative imaging studies, and follow-up information. This study was approved by the institutional review board of the Third Affiliated Hospital of Sun Yat-sen University (No. II2023-250-01). Written informed consent was obtained from each patient.
Angiographic classification
All patients, except one, underwent selective angiography through arterial access to acquire detailed anatomical and hemodynamic data. Prior to embolization, two interventional radiologists independently reviewed angiographic images and categorized AVMs based on Cho et al.’s classification,[27] reaching a consensus. A highly experienced vascular surgeon made the final decision. The AVMs were classified into four types based on their angiographic morphology.
Procedures
All embolization procedures were conducted under local anesthesia and guided by digital subtraction angiography (DSA). Initially, diagnostic angiography was performed to confirm the diagnosis and comprehend the vascular architecture of AVMs. When the draining veins of the lesion were identifiable and relatively large, methods such as compression, tourniquet application, or ligation were employed to decelerate blood flow. Subsequently, suitable microcatheters were chosen based on angiographic images to attempt superselection of each feeding artery of the AVMs. After verifying the position with repeat angiography, appropriate embolic agents were meticulously prepared and slowly injected through the microcatheter. Injection was halted upon stagnation or retrograde flow of blood toward the microcatheter tip, followed by angiography to confirm the extent of embolization. Comprehensive angiography was performed upon achieving satisfactory embolization of all superselected feeding arteries to evaluate the efficacy of embolization.
In instances where small, tortuous feeding arteries of the AVMs were challenging to superselect via arterial access alone, a combined approach was implemented to augment treatment efficacy, involving arterial embolization followed by percutaneous embolization. Utilizing techniques like compression of superficial feeding arteries and draining veins to attenuate blood flow, a 7-French scalp needle was initially employed for percutaneous puncture of the lesion until blood was visualized. Subsequent angiography through the puncture needle confirmed its position, assessed vascular structure and size, and facilitated the preparation of tissue glue embolic agents in varied proportions based on the flow rate. Under DSA guidance, tissue glue was slowly injected until favorable outcomes were attained, followed by subsequent arterial angiography to assess treatment outcomes. Multiple sessions of arterial/percutaneous embolization were conducted for larger lesions to achieve complete nidus occlusion.
Follow-up
During hospitalization and outpatient or telephone follow-up, all patients were closely monitored, and occurrences of complications or changes in symptoms were recorded. Assessment of treatment efficacy was conducted 3–6 months after the final treatment session. Additional embolization or sclerotherapy was recommended if symptoms recurred or worsened post-treatment, affecting quality of life, or if residual AVMs were detected on follow-up imaging examinations.
Statistical analysis
Statistical analysis was performed using Fisher’s exact test to determine the relationship between AVM staging/types and treatment efficacy. IBM Statistical Package for the Social Sciences Statistics Version 22.0 (IBM, New York, USA) was utilized for statistical analysis, with P < 0.05 being considered statistically significant.
RESULTS
Patients and demographics
Demographic and clinical characteristics of patients with AVM are presented in Table 1. A total of 11 patients meeting the inclusion criteria were included. Among them, there were 5 male and 6 female patients, with a mean age of 36.1 ± 7.1 years (range: 12–66 years). Pain and swelling were the most common symptoms, with 5 cases classified as Schobinger II and 6 cases as Schobinger III [Table 1]. All patients had type IIIb AVMs, except for Patient 8, who had a combination of type IIIa and IIIb. AVMs were predominantly located in the limbs and head, including the fingers, forearms, lower legs, thighs, and head. Notably, the highest prevalence of AVMs was observed in the hands (including fingers and forearms).
| Patient ID | Gender | Age | Location | Type | Stage | Past treatments | Symptoms |
|---|---|---|---|---|---|---|---|
| 1 | Female | 38 | Left lower jaw | IIIb | II | None | Swelling |
| 2 | Female | 22 | Right calf | IIIb | III | Embolization | Swelling, Pain |
| 3 | Male | 66 | Right forearm | IIIb | II | Excision | Swelling |
| 4 | Female | 23 | Left finger | IIIb | III | None | Swelling, Pain, Vascular tufts |
| 5 | Female | 26 | Left hand, Left forearm | IIIb | II | 2 times Embolization | Vascular tufts |
| 6 | Male | 49 | Left finger | IIIb | III | Excision | Swelling, Pain |
| 7 | Female | 27 | Left forehead | IIIb | III | Excision | Swelling, Pain |
| 8 | Female | 12 | Left thigh, Left knee | IIIa, IIIb | II | Excision | Swelling |
| 9 | Male | 36 | Forehead | IIIb | II | None | Swelling |
| 10 | Male | 42 | Right forearm, Right hand | IIIb | III | 2 times Excision | Swelling, Pain, Vascular tufts |
| 11 | Male | 28 | Right forearm | IIIb | III | None | Swelling, Pain |
Treatment details
The detailed treatment procedures are outlined in Table 2. Among the 11 patients, 5 achieved complete devascularization of AVM lesions. Notably, in one case [Patient 3], due to tortuous and small feeding arteries, a direct percutaneous injection of glue was performed after ligation and dilation of the draining vein. A patient (Patient 7) diagnosed with a left frontal AVM (Figures 1a-c) initially underwent the release of spring coils followed by n-butyl cyanoacrylate (NBCA) embolization via arterial access under manual compression of superficial drainage veins (Figure 1d). Subsequently, percutaneous glue injection was performed (Figure 1e). Post-embolization angiogram demonstrated complete occlusion of the AVM nidus (Figure 1f). Another patient (patient 11) diagnosed with a right forearm AVM (Figures 2a-b) underwent spring coils release via arterial access under manual compression of superficial drainage veins (Figure 2c). Subsequently, percutaneous glue injection was performed (Figure 2d). Post-embolization angiogram demonstrating complete occlusion of the AVM nidus (Figure 2e). One-month post-embolization MRI showed a reduction in the lesion size compared to previous imaging, with no visible flow voids (Figure 2f). Patient 8, diagnosed with a left thigh and left knee AVM (Figures 3a-b), underwent polyvinyl alcohol (PVA) and glue embolization via arterial access under tourniquet compression (Figure 3c). Post-embolization angiography demonstrated near-complete occlusion of the AVM nidus (Figure 3d). Subsequently, percutaneous glue injection was performed for the residual left knee AVM (Figure 3e). Final angiogram confirmed complete occlusion of the entire AVM nidus (Figure 3f).
| Patient ID | Number of Treatments | Treatment Pathway | Transarterial | Percutaneous | Transvenous |
|---|---|---|---|---|---|
| 1 | 1 | TA, TP | PVA, gelatin sponge, coil, glue | Glue | None |
| 2 | 3 | TA, TV, TP+TP+TA, TV, TP | Glue+0+PVA | Glue+polyvinyl alcohol foam+glue | Ligation+ None+Ligation |
| 3 | 1 | TV, P | None | Glue | Ligation |
| 4 | 2 | TA, TV, TP+TA | PVA+PVA | Glue+None | Ligation+None |
| 5 | 2 | P+P | Compression +Compression |
Glue+Glue | Compression +Compression |
| 6 | 1 | P | Compression | Glue | Compression |
| 7 | 1 | A, P | Coil, Glue | Glue | Compression |
| 8 | 1 | A, P | PVA, Bleomycin | Glue | Tourniquet |
| 9 | 2 | A,P +A | Glue+PVA | Glue+None | Compression +Compression |
| 10 | 1 | A, P | PVA, Bleomycin | Glue | Compression |
| 11 | 1 | A, P | Coil | Glue | Compression |
| Patient ID | Occlusion rate (%) | Outcome | Complications | Follow-up time (months) | |
| 1 | >90 | Significant improvement | None | 75 | |
| 2 | 50–90 | Partial improvement | None | 67 | |
| 3 | 100 | Complete recovery | None | 53 | |
| 4 | >90 | Significant improvement | None | 55 | |
| 5 | <50 | No change | None | 3 | |
| 6 | >90 | Significant improvement | None | 41 | |
| 7 | 100 | Complete recovery | None | 25 | |
| 8 | 100 | Complete recovery | None | 6 | |
| 9 | 100 | Complete recovery | None | 5 | |
| 10 | >90 | Significant improvement | Mild | 4 | |
| 11 | 100 | Complete recovery | None | 4 | |
TA: Transarterial, TP: Percutaneous, TV: Transvenous, PVA: Polyvinyl alcohol, A,P: Transarterial combined with percutaneous
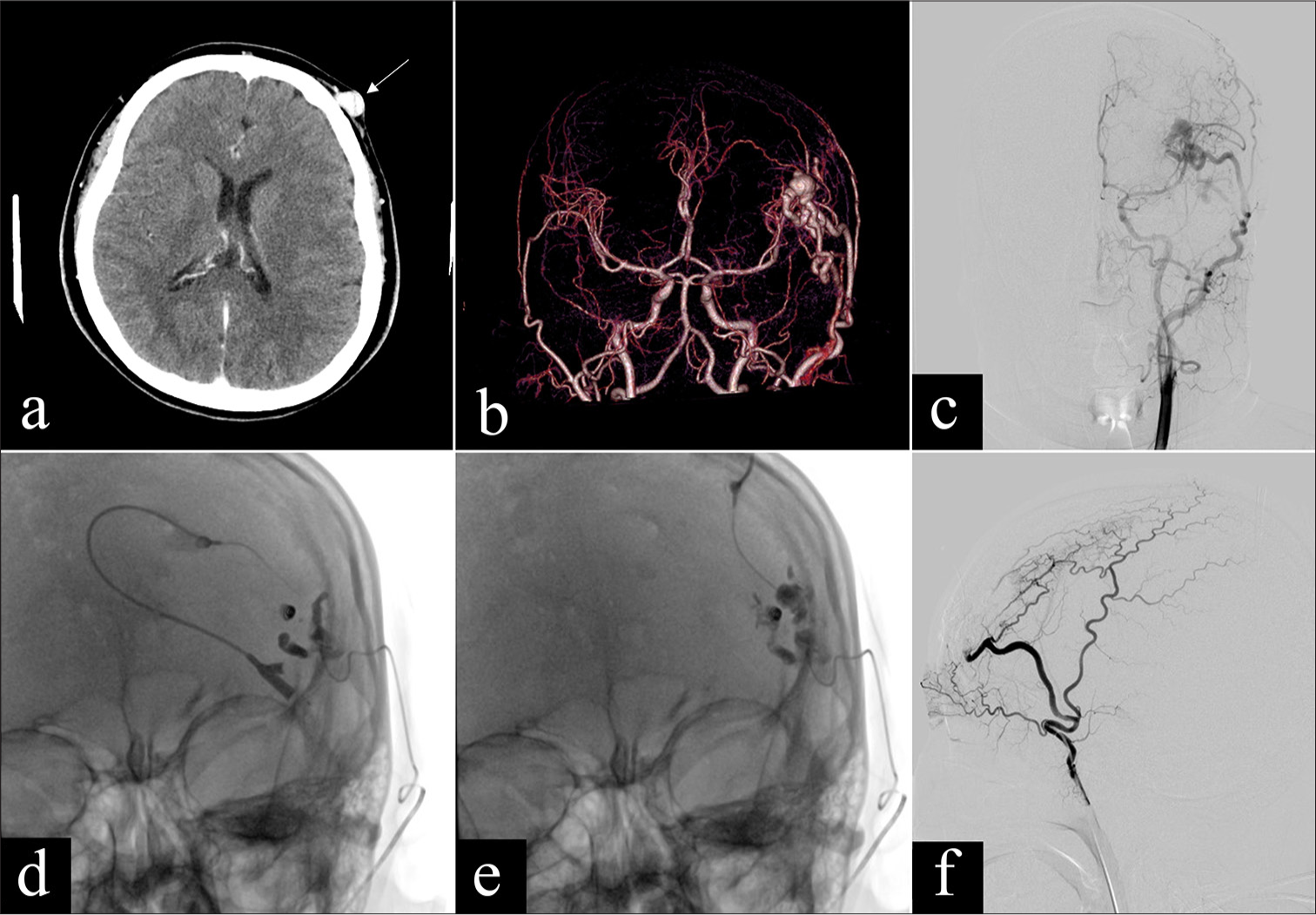
- A 27-year-old female (Patient 7) diagnosed with left frontal arteriovenous malformation (AVM), characterized by swelling, locally elevated skin temperature, occasional throbbing pain, and palpable tremor, classified as type IIIb. (a) Axial enhanced computed tomography (CT) revealing subcutaneous AVMs in the left frontal region, with visible abnormal vascular clusters (yellow arrow). (b) CT angiography displaying the vascular architecture of the AVM, highlighting multiple dilated feeding arteries and draining veins. (c) Angiography revealing the vascular structure and dilated feeding arteries and draining veins. (d) Fluoroscopic image after the release of spring coils (3 mm and 4 mm each) via arterial access and subsequent use of tissue glue embolization, depicting the coils in place and n-butyl cyanoacrylate (nBCA)/iodized oil cast. (e) Fluoroscopic image after percutaneous injection of tissue glue, displaying nBCA/iodized oil cast. (f) Post-embolization angiogram demonstrating complete occlusion of the AVM nidus. Following the procedure, the patient experienced complete resolution of symptoms, with no recurrence observed during follow-up. The treatment outcome was categorized as “complete recovery.”
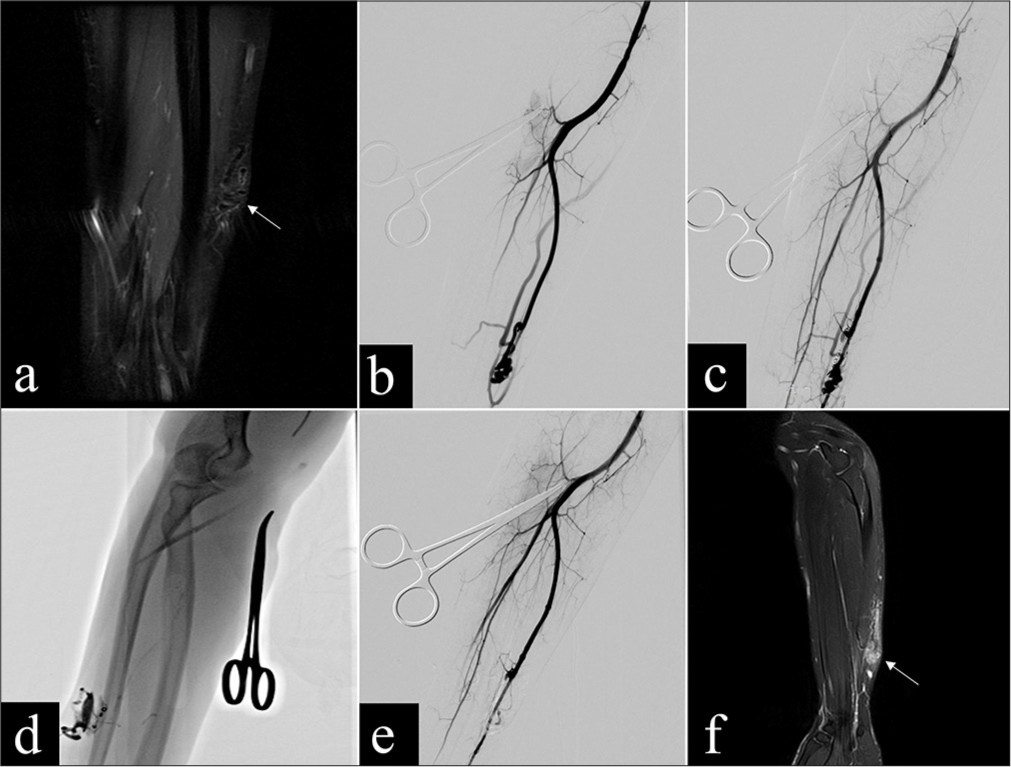
- A 28-year-old male (Patient 11) diagnosed with arteriovenous malformations (AVMs) on the ulnar side of the right forearm, presenting symptoms including swelling, pain, locally elevated skin temperature, and palpable pulsation, classified as type IIIb. (a) Coronal T2-weighted magnetic resonance imaging (MRI) sequence revealing a lesion on the ulnar side of the right forearm, with evident flow voids indicating blood vessels (yellow arrow). (b) Angiography displaying the AVM nidus (yellow arrow). (c) Post-release of spring coils via arterial access (two coils of 3 mm and one coil of 4 mm), angiography showing partial occlusion of the nidus and reduced blood flow in the AVMs. (d) Fluoroscopic image during percutaneous injection of tissue glue. (e) Post-embolization angiogram showing complete occlusion of the AVMs nidus. (f) One-month post-embolization, coronal T2-weighted MRI sequence indicating a reduction in the lesion size compared to previous images, with no visible flow voids (yellow arrow). Following the procedure, the patient experienced significant improvement in swelling, normalization of skin temperature, and basic disappearance of pain. No symptom exacerbation was observed during follow-up. The treatment outcome was categorized as “complete recovery.”
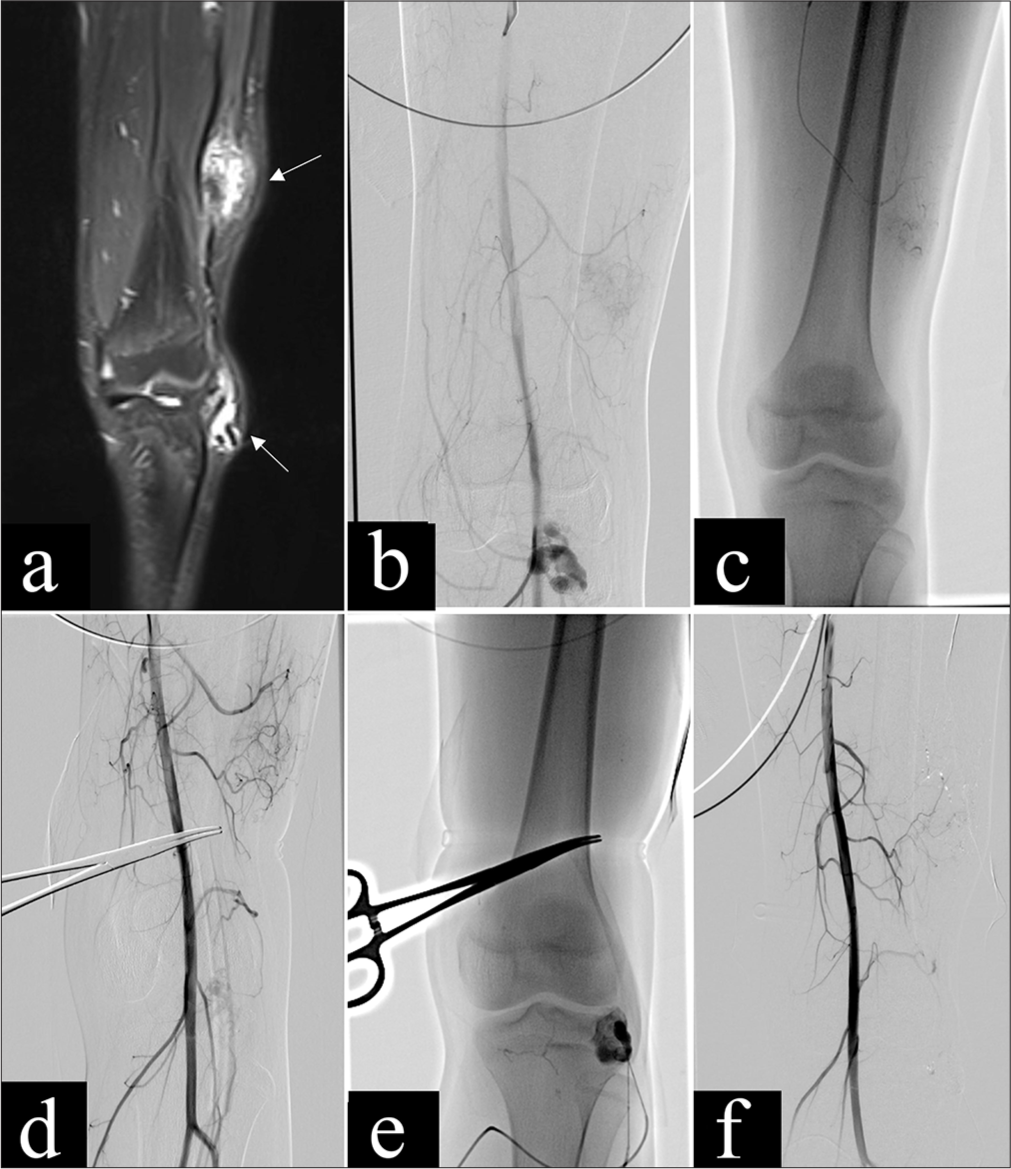
- A 12-year-old girl (Patient 8) with arteriovenous malformations (AVMs) in the mid-lower segment of the left thigh and left knee joint, presenting with pulsatile masses. The AVM in the left thigh was classified as type IIIa, while the AVM in the left knee was classified as type IIIb. (a) Coronal T2-weighted magnetic resonance imaging sequence showed two lesion sites in the mid-lower segment of the left thigh and left knee joint, with visible abnormal vascular clusters (yellow arrows). (b) Angiography displayed the vascular architecture of the AVM lesions at both sites and the dilated feeding arteries and draining veins (yellow arrow). (c) Fluoroscopic image after arterial embolization using PVA and Onyx, showed cast formation within the nidus. (d) Post-arterial embolization angiogram demonstrated partial occlusion of the AVM nidus in the mid-lower segment of the left thigh. (e) Fluoroscopic image after percutaneous injection of tissue glue into the AVM nidus in the left knee joint showed n-butyl cyanoacrylate /iodized oil cast. (f) Post-embolization angiogram demonstrated complete occlusion of the AVM nidus. Following the procedure, the pulsatile masses in the left thigh and left knee decreased in size compared to before. No enlargement of the masses or other symptoms were observed during follow-up. The treatment outcome was categorized as “complete recovery.”
Four patients achieved over 90% occlusion of AVM vessels. In one case (Patient 6), direct percutaneous glue injection was performed due to tortuous and small feeding arteries. In two cases (Patient 1 and 10), arterial embolization was performed initially followed by percutaneous glue injection. Patient 4 underwent staged embolization due to the large lesion, with residual nidus embolization during the second hospitalization.
One patient had an occlusion rate between 50 and 90%. This patient (Patient 2) underwent three embolization treatments. Initially, after ligation of the draining vein, arterial embolization with glue was performed, followed by percutaneous glue injection. During the second hospitalization, the patient underwent percutaneous polidocanol sclerotherapy. During the third hospitalization, after ligation of the draining vein, arterial embolization with PVA was performed, followed by percutaneous glue injection.
One patient had an occlusion rate below 50%. In this case (Patient 5), direct percutaneous glue injection was performed under manual compression of veins due to tortuous and small feeding arteries.
Treatment outcomes
The comprehensive treatment outcomes of AVM patients are summarized in Table 2. Clinical symptoms completely disappeared in three patients, with two experiencing pain cessation and three exhibiting complete regression of swelling. In addition, clinical symptoms significantly improved in four patients, with three reporting notable alleviation of pain, four showing considerable reduction in swelling, and one displaying marked reduction in varicose vein clusters. Moreover, partial relief of symptoms was observed in four patients, with three demonstrating reduced swelling and two showing decreased vascular clusters, while one experienced partial relief of pain.
Thus, 5 (45.4%) cases achieved complete recovery, 4 (36.4%) cases showed significant improvement, 1 (9.1%) case was categorized as partial improvement, and 1 (9.1%) case showed no change. The overall treatment success rate was 81.8% (9/11). During the follow-up period, none of the patients experienced symptom exacerbation or recurrence.
There were no significant differences in treatment efficacy among patients with different Schobinger stages and Cho-Do subtypes [Table 3].
| Treatment successful | Treatment unsuccessful | P-value | |
|---|---|---|---|
| Schöbinger stages | successful | unsuccessful | P-value |
| II | 4 | 1 | P=1.00 |
| III | 5 | 1 | |
| Cho-Do subtypes | successful | unsuccessful | P-value |
| II | 1 | 0 | P=1.00 |
| IIIa; IIIb | 1 | 0 | |
| IIIb | 7 | 2 |
Adverse events and complications
Most patients experienced transient local pain and accompanying edema after surgery, which was attributed to inflammatory reactions. Among a total of 16 procedures, one case of mild complication occurred. The patient presented with multiple serpentine and tortuous vascular clusters on the surface of the right forearm and hand before treatment, with involvement of the index and middle fingers. A single embolization treatment was performed, preceded by arterial angiography for diagnostic confirmation. Subsequently, the lesion nests and draining veins were embolized percutaneously under compression of superficial drainage veins using tissue glue, while PVA and bleomycin were administered transarterially to embolize the feeding arteries and residual nests. The patient experienced persistent pain in the surgical area for over 2 months post-embolization, with partial relief achieved through analgesic medication. Visible pigmentation deposits were observed on the skin of the right index and middle fingers. Over the course of more than 3 months post-surgery, the pain gradually subsided and eventually disappeared, with the pigmentation on the skin of the right index and middle fingers remaining largely unchanged.
DISCUSSION
AVMs typically comprise feeding arteries, draining veins, and a nidus, with the latter being the primary focus of therapeutic intervention due to its role in sustaining abnormal circulation. Effective treatment strategies aim to disrupt the abnormal flow within the nidus, reducing hemorrhage risk and alleviating associated symptoms.
nBCA, a widely used liquid embolic agent, polymerizes rapidly upon contact with ionic substances like blood or water,[28] offering advantages such as affordability and accessibility. Its liquid form enables distal embolization via a flow-directed strategy, facilitating precise vessel occlusion within the AVM nidus.[29] Upon injection, nBCA initiates a polymerization reaction, leading to acute inflammatory response and eventual vascular occlusion.[30,31] In our center, nBCA is typically mixed with iodized oil to enhance visibility and control the rate of polymerization. nBCA exhibits a high thrombogenic potential, allowing for progressive and permanent occlusion.[32] Despite its validated efficacy in AVM embolization, studies have indicated a possibility of recurrence, particularly in cases of partial embolization without complete nidus occlusion.[18,31]
Although ethylene vinyl alcohol copolymer (EVOH)-based agents such as Onyx and Squid have emerged as effective embolic materials for the treatment of both intracranial and extracranial AVMs over the past decade,[33,34] their use was not incorporated in this study. This was primarily due to cost limitations and regional accessibility issues. In addition, our team possessed greater familiarity with nBCA, allowing for safer and more controlled embolization in our local context. Nonetheless, we recognize the growing body of evidence supporting EVOH as a valuable tool in AVM management and plan to incorporate it in future investigations as access and clinical experience expand.
The intricate anatomical structures of AVMs, including tortuous feeding arteries, pose challenges in positioning microcatheter tips near the nidus for complete occlusion. In clinical practice, percutaneous access appears to facilitate better tissue adhesive infiltration into the nidus, achieving more thorough AVM embolization. Although the use of nBCA as a liquid embolic agent is well established for AVM management, our study specifically investigates the synergistic effect of combining percutaneous glue embolization with arterial embolization. This dual technique allows for more comprehensive occlusion of the AVM nidus, particularly in cases where arterial access is limited or insufficient due to small, tortuous feeding vessels. By integrating both access routes, this approach enhances the likelihood of complete nidus embolization, thereby reducing recurrence risk. Consequently, our study initially focuses on arterial occlusion of the nidus and subsequently employs percutaneous embolization for residual nidus occlusion. In Israrahmed et al.’s study on scalp AVMs, tissue adhesive was exclusively used as an embolic agent for complete occlusion of small lesions or as adjunctive therapy prior to resection of large lesions.[23] With accumulated experience, the researchers found that direct percutaneous injection of tissue adhesive could penetrate lesions more effectively, achieving more complete embolization. Thus, in the later stages of their study, the investigators primarily adopted the percutaneous approach for embolization therapy, which yielded favorable outcomes. The findings of Israrahmed et al.’s[23] study align closely with our observations.
Le Fourn et al. utilized nBCA, PVA particles, and absolute ethanol for the treatment of limb and head-and-neck AVMs, achieving a vessel occlusion rate exceeding 75% in 56% of patients (18/32). However, the complication rate was 55% (23/42).[35] Bissacco et al. employed nBCA for AVM embolization in limbs, with 18 out of 21 (86%) patients achieving optimal or suboptimal results. Specifically, 10 patients exhibited optimal response, indicating complete vessel occlusion, while 8 patients showed suboptimal response, with residual flow within the treated vessels but decreased flow compared to before treatment. It is noteworthy that only 2 (9.4%) complications occurred in this study.[8] Kitagawa et al.’s study confirmed the safety and efficacy of percutaneous ethanol sclerotherapy combined with arterial embolization using tissue glue for extracranial AVMs. In the study, 87% (20/23) of patients achieved a vessel occlusion rate exceeding 75%, with 2 cases of minor complications.[17]
Different anatomical locations and angioarchitectural features of AVMs can influence both treatment strategy and risk of complications. For example, digital AVMs may involve end-arterial circulation and pose a higher risk of ischemia and possible amputation. Cirsoid AVMs, particularly those involving the scalp or face, may have complex vascular networks, including potential extracranial-intracranial arterial anastomoses, increasing the risk of cerebral embolism or pulmonary embolism due to high-flow shunts. In our cohort, no major complications such as amputation or embolic events were observed, likely due to careful case selection, thorough pre-procedural angiographic evaluation, and real-time DSA-guided embolization. Nonetheless, further studies with larger sample sizes are warranted to better understand complication risks across different AVM subtypes.
In this study, 5 (45.4%) cases attained complete recovery, while 4 (36.4%) cases exhibited significant improvement, yielding an overall treatment success rate (vessel occlusion rate exceeding 90%) of 81.8% (9/11). Only one complication was encountered and resolved conservatively. Considering the tendency for AVM recurrence, the efficacy evaluation criteria adopted in this study were stringent. However, compared to previous relevant studies,[8,17,35] this study demonstrated a higher treatment success rate and a lower complication rate. This outcome may be attributed to the comparatively gentle nature of tissue glue embolization. This suggests that percutaneous injection of tissue glue combined with arterial embolization is safe and effective, with an acceptable complication rate, for superficial AVMs. In this study, there was no statistically significant difference in efficacy among patients with different Schobinger stages and Cho-Do subtypes, possibly due to the small sample size.
This study has several limitations. First, the retrospective nature introduces inherent biases and limits the establishment of causal relationships. The small sample size, only 11 patients over an 8-year period, was primarily due to the rarity of extracranial AVMs and the retrospective design, which limits the ability to accumulate a large number of cases in a short timeframe. Second, the study cohort was heterogeneous, involving various anatomical sites such as the hand, limbs, and scalp (including one case of cirsoid aneurysm). This heterogeneity may introduce variability in clinical presentation and treatment response. However, it also mirrors real-world clinical scenarios and broadens the applicability of our findings. Third, the lack of continuous and standardized follow-up data hampers the comprehensive evaluation of treatment efficacy, and the risk of AVM recurrence over time remains a concern. Furthermore, treatment outcomes were primarily assessed based on imaging, while clinical symptom relief was not thoroughly evaluated. Future prospective, multicenter studies with larger and more homogeneous populations are warranted to validate our conclusions and to compare the long-term efficacy of different embolization techniques.
CONCLUSION
The combined approach of percutaneous glue embolization with arterial embolization proves to be safe and effective in treating extracranial AVMs. However, further research validation and broader data analysis are needed to strengthen the evidence base and optimize treatment strategies.
Ethical approval:
The research/study was approved by the Institutional Review Board of the Third Affiliated Hospital of Sun Yat-sen University, number No. II2023-250-01, dated September 2023.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflict of interest:
There are no conflict of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Arteriovenous malformations In: Handbook of cerebrovascular disease and neurointerventional technique. Cham: Springer International Publishing; 2023. p. :761-803.
- [CrossRef] [Google Scholar]
- Head and neck arteriovenous malformations: University of Tennessee experience, 2012-2022. Neurosurg Focus. 2022;53:E17.
- [CrossRef] [PubMed] [Google Scholar]
- Overview of peripheral arteriovenous malformations: From diagnosis to treatment methods. J Interv Med. 2023;6:170-5.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular anomalies: Classification, imaging characteristics and implications for interventional radiology treatment approaches. Br J Radiol. 2014;87:20130392.
- [CrossRef] [PubMed] [Google Scholar]
- Management of extracranial arteriovenous malformations of the head and neck. Auris Nasus Larynx. 2020;47:181-90.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of extracranial arteriovenous malformations after multiple embolizations: Outcomes in a series of 31 patients. Plast Reconstr Surg. 2015;135:543-52.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term outcome of embolotherapy and surgery for high-flow extremity arteriovenous malformations. J Vasc Interv Radiol. 2000;11:1285-95.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular approach for arteriovenous limb malformations: A single center experience. Int Angiol. 2021;40:165-9.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular management of arteriovenous malformation-associated intracranial aneurysms: A systematic literature review. World Neurosurg. 2022;164:257-69.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment outcomes of embolization for peripheral arteriovenous malformations. J Vasc Interv Radiol. 2020;31:1801-9.
- [CrossRef] [PubMed] [Google Scholar]
- Intraosseous arteriovenous malformations in the extremities managed with coils and absolute ethanol treatment. Ann Vasc Surg. 2020;65:152-9.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of major complication following embolosclerotherapy for upper and lower extremity vascular malformations. Vascular. 2021;29:69-77.
- [CrossRef] [PubMed] [Google Scholar]
- Therapeutic outcomes of embolotherapy of extremity bone intraosseous arteriovenous malformation with ethanol, coils, and n-butyl cyanoacrylate. J Vasc Surg. 2021;73:2090-7.e5.
- [CrossRef] [PubMed] [Google Scholar]
- Successful embolization of an anterior chest wall arteriovenous malformation using combined transfemoral and transradial approaches with onyx. Radiol Case Rep. 2024;19:2151-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fatal pulmonary embolism of polyvinyl alcohol particles following therapeutic embolisation of a peripheral arteriovenous malformation. BMJ Case Rep. 2009;2009:bcr02.2009.1635.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective study of polytetrafluoroethylene-covered microplugs and detachable coils for embolization of pulmonary arteriovenous malformations: Technical results, procedure times, and costs. J Vasc Interv Radiol. 2024;35:362-9.
- [CrossRef] [PubMed] [Google Scholar]
- Polidocanol sclerotherapy combined with transarterial embolization using n-butyl cyanoacrylate for extracranial arteriovenous malformations. Cardiovasc Intervent Radiol. 2018;41:856-66.
- [CrossRef] [PubMed] [Google Scholar]
- Coil-protected technique for liquid embolization in neurovascular malformations. Korean J Radiol. 2019;20:1285-92.
- [CrossRef] [PubMed] [Google Scholar]
- Onyx transarterial embolization of dural arteriovenous fistula for failed N-butyl cyanoacrylate treatment: Case report. J Neuroendovasc Ther. 2009;3:174-80.
- [CrossRef] [Google Scholar]
- Arteriovenous malformations: Syndrome identification and vascular management. Curr Treat Options Cardiovasc Med. 2018;20:67.
- [CrossRef] [PubMed] [Google Scholar]
- Absolute ethanol embolization of infiltrating-diffuse extracranial arteriovenous malformations in the head and neck. Eur J Vasc Endovasc Surg. 2015;50:114-21.
- [CrossRef] [PubMed] [Google Scholar]
- Ethanolamine oleate sclerotherapy combined with transarterial embolization using n-butyl cyanoacrylate for extracranial arteriovenous malformations. Cardiovasc Intervent Radiol. 2014;37:371-80.
- [CrossRef] [PubMed] [Google Scholar]
- Management of scalp arteriovenous malformations: A rising trend towards percutaneous direct puncture embolization technique-our experience. Acta Radiol. 2023;64:2431-8.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous direct puncture embolization for superficial craniofacial arteriovenous malformation. Interv Neuroradiol. 2008;14(Suppl 2):19-22.
- [CrossRef] [PubMed] [Google Scholar]
- Venous vascular malformations of the craniofacial region: Pre-operative embolisation with direct percutaneous puncture and N-butyl cyanoacrylate. Br J Radiol. 2008;81:935-9.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous direct needle puncture and transcatheter N-butyl cyanoacrylate injection techniques for the embolization of pseudoaneurysms and aneurysms of arteries supplying the hepato-pancreato-biliary system and gastrointestinal tract. J Clin Imaging Sci. 2016;6:48.
- [CrossRef] [PubMed] [Google Scholar]
- Arteriovenous malformations of the body and extremities: analysis of therapeutic outcomes and approaches according to a modified angiographic classification. J Endovasc Ther. 2006;13:527-38.
- [CrossRef] [PubMed] [Google Scholar]
- Direct N-butyl-2-cyanoacrylate injections to the head and neck for percutaneous embolized devascularization. Surg Neurol Int. 2021;12:131.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular therapeutic embolisation: An overview of occluding agents and their effects on embolised tissues. Curr Vasc Pharmacol. 2009;7:250-63.
- [CrossRef] [PubMed] [Google Scholar]
- Advances in biomaterials and technologies for vascular embolization. Adv Mater. 2019;31:e1901071.
- [CrossRef] [PubMed] [Google Scholar]
- The use of cyanoacrylate adhesives in peripheral embolization. J Vasc Interv Radiol. 2001;12:907-13.
- [CrossRef] [PubMed] [Google Scholar]
- A case of venous anomaly of diploic origin successfully treated by preoperative direct puncture sclerotherapy. J Neuroendovasc Ther. 2018;12:341-7.
- [CrossRef] [Google Scholar]
- Safety and effectiveness of ethylene vinyl alcohol copolymer embolization of peripheral high-flow arteriovenous malformations: Results of a prospective study. J Vasc Interv Radiol. 2021;32:1644-53.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Stereotactic radiosurgery for arteriovenous malformations after onyx embolization: A case-control study. J Neurosurg. 2015;123:126-35.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of embolization in arteriovenous malformations of the extremities and head and neck: A retrospective study of 32 cases. Eur J Dermatol. 2015;25:52-6.
- [CrossRef] [PubMed] [Google Scholar]






