Translate this page into:
Pancreaticoportal Fistula Formation as a Consequence of Recurrent Acute Pancreatitis: Clinical and Imaging Considerations
Address for correspondence: Dr. Mina S Makary, Department of Radiology, The Ohio State University Wexner Medical Center, 395 W 12th Avenue, Columbus 43210, Ohio, USA. E-mail: mina.makary@osumc.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A pancreatic-portal vein fistula (PPVF) is an extremely rare complication of pancreatitis. In this report, we present a patient with a PPVF in the setting of recurrent pancreatitis and portal vein thrombosis diagnosed by cross-sectional imaging and endoscopic retrograde cholangio-pancreatography, who responded to medical management and anticoagulation. A critical review of this disease process is explored to highlight pathology, imaging characteristics, and essential alternative diagnostic considerations. We also discuss potential complications and current treatment strategies. PPVFs pose a unique diagnostic challenge and awareness of its clinical presentation can further improve patient outcomes.
Keywords
Complications
pancreaticoportal fistula
pancreatitis
portal vein
pseudocyst

INTRODUCTION
Acute pancreatitis occurs when there is inflammation of the pancreas that leads to a cascade of inflammatory markers and systemic inflammation. Acute pancreatitis can have a variety of inflammatory and vascular complications with varying severity.[1] While pseudocyst formation, portal vein thrombosis and arterial pseudoaneurysms are relatively well described and routinely diagnosed complications of pancreatitis occurring in up to 20% of the cases, the formation of a pancreatic-portal vein fistula (PPVF), in which a fistulous tract develops between the portal vein and pancreatic duct, is an extremely rare entity with only 18 cases reported in the literature till date.[234] In this report, we present a patient with recurrent episodes of acute pancreatitis due to a hereditary mutation in PRSS1, complicated by the development of a PPVF. This case study presents a diagnostic approach based on clinical, laboratory, and imaging characteristics, as well as shed some light on the response to therapy and disease evolution.
CASE REPORT
A 75-year-old woman with a medical history significant for hereditary pancreatitis and type II diabetes mellitus presented with an episode of acute pancreatitis and recent weight loss. The patient suffered recurrent episodes of pancreatitis sporadically for the past 30 years, which were generally mild and resolved with bowel rest, pain management, and hydration. The PRSS1 mutation was present in this patient. Similarly, multiple members of the patient's family tested positive for the hereditary pancreatitis mutation PRSS1 and had repeated pancreatitis necessitating pancreatectomy.
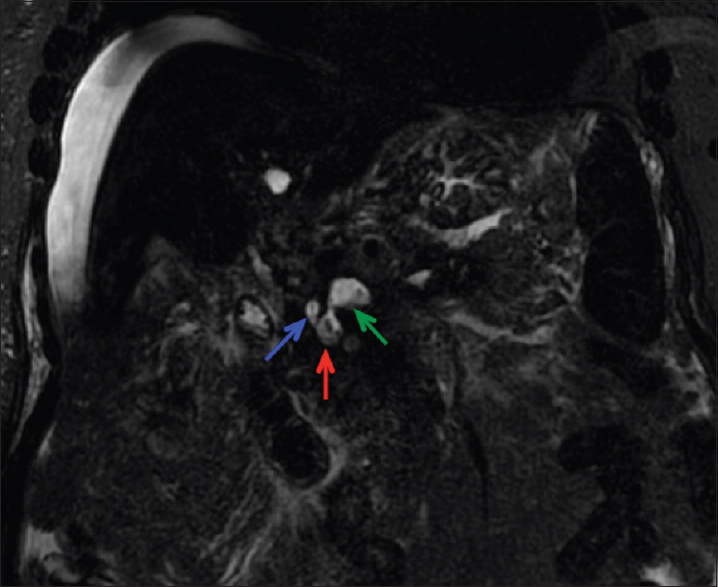
Laboratory workup revealed an elevated lipase of 973 (NL: 0–160 U/L). Computed tomography (CT) imaging demonstrated findings of acute pancreatitis, including an edematous pancreas, peripancreatic edema, and fat stranding [Figure 1]. Pancreatic parenchymal calcifications which would be expected with a chronic process were absent. Abdominal magnetic resonance imaging (MRI) showed a dilated pancreatic duct as well as thrombosis of the portal vein, splenic vein, superior mesenteric vein, and the majority of the intrahepatic portal vein branches [Figure 2]. Magnetic resonance cholangiopancreatography (MRCP) further demonstrated abnormal fluid signal intensity in the portal vein and splenoportal confluence. An adjacent fluid collection was also noted consistent with a pseudocyst, with the suggestion of fistulous communication between the pseudocyst, the portal vein, and the main pancreatic duct at the head region raising suspicion for a PPVF [Figure 3].
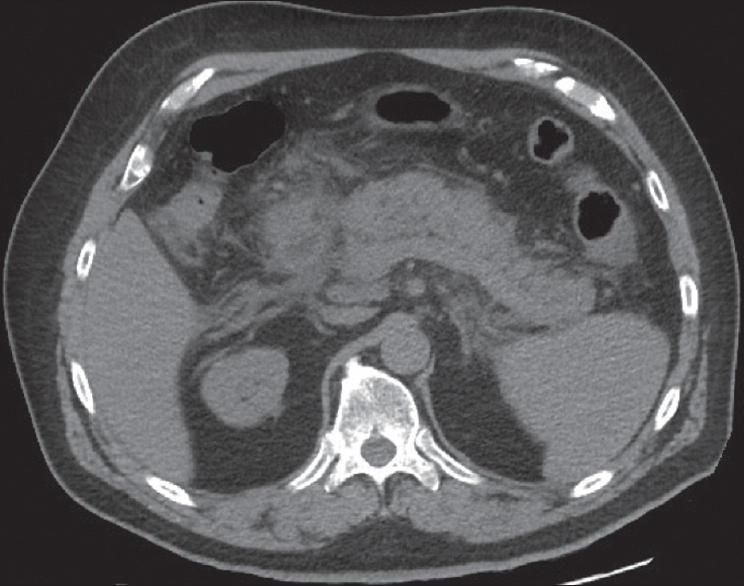
- Noncontrast axial computed tomography of the abdomen demonstrating characteristic findings of acute pancreatitis, including indistinct pancreatic margins, edema, and fat stranding.
![(a) Axial fat-suppressed T2-weighted image demonstrating a dilated fluid-filled pancreatic duct (blue arrow) anterior to a T2-hyperintense tubular structure [red arrow] which on the axial fat-saturated postcontrast T1-weighted image (b) corresponds to an expanded portal confluence lacking normal enhancement and containing a filling defect consistent with portal venous thrombosis (green arrow).](/content/12/2018/8/1/img/JCIS-8-4-g003.png)
- (a) Axial fat-suppressed T2-weighted image demonstrating a dilated fluid-filled pancreatic duct (blue arrow) anterior to a T2-hyperintense tubular structure [red arrow] which on the axial fat-saturated postcontrast T1-weighted image (b) corresponds to an expanded portal confluence lacking normal enhancement and containing a filling defect consistent with portal venous thrombosis (green arrow).
- Coronal magnetic resonance cholangiopancreatography image demonstrating fistulization between the portal vein (green arrow), pseudocyst (red arrow), and pancreatic duct (blue arrow).
Endoscopic retrograde cholangiopancreatography (ERCP) was subsequently performed to evaluate the pancreatic duct. A pancreatic duct leak was identified, but the guidewire could not be passed to traverse the leak, and therefore, no intervention was performed. The ERCP revealed contrast filling the small collection after cannulation of the main pancreatic duct at the ampulla. However, there was also opacification of the portal vein in the same injection of contrast, confirming the MRI suspicion of a PPVF [Figure 4].
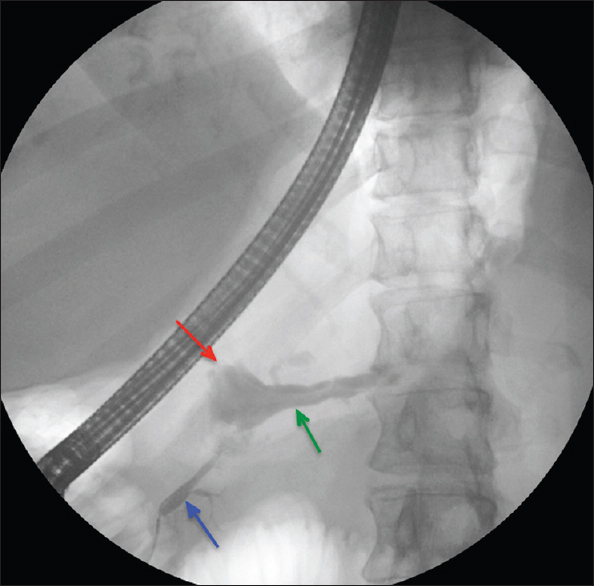
- Endoscopic retrograde cholangiopancreatography fluoroscopic image demonstrating cannulation of the pancreatic duct (blue arrow) with abnormal contrast passage into the portal vein (green arrow) and associated intervening pseudocyst (red arrow) confirming the presence of the pancreatic-portal vein fistula.
The patient underwent supportive medical management for symptom control and anticoagulation for the portal thrombosis for 2 months. The anticoagulant used was Warfarin 4 mg daily which was titrated appropriately to achieve a therapeutic international normalized ratio (2-3). Over the next 4 months, the patient's symptoms improved and anticoagulation was subsequently stopped once collateral circulation was identified on follow-up imaging [Figure 5].
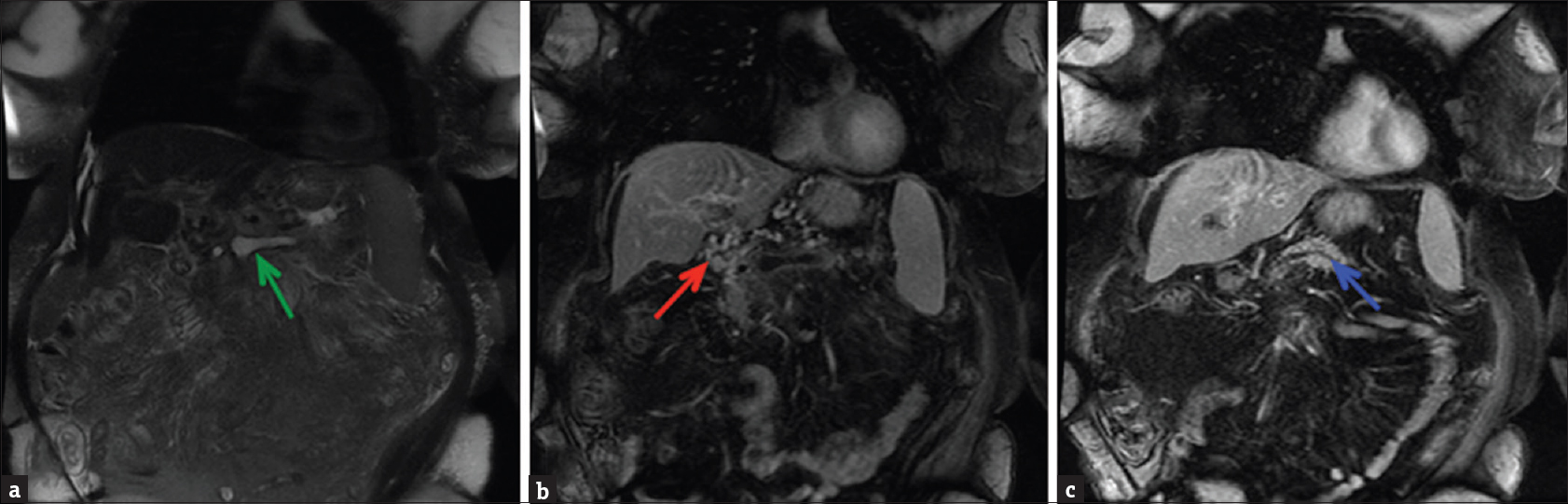
- (a) Coronal fat-suppressed T2-weighted image demonstrating hyperintense fluid signal in the splenoportal confluence (green arrow) (b) Coronal fat-suppressed post-contrast T1-weighted image demonstrating nonenhancement of the portal venous confluence, consistent with thrombosis. Numerous enhancing collaterals (red arrow) are present in the porta hepatis region confirming the chronic nature of the thrombus and cavernous transformation of the portal vein. (c) A more posterior coronal fat-suppressed postcontrast T1-weighted image revealing a prominent pancreatic duct (blue arrow).
DISCUSSION
PPVF formation is a rare complication of pancreatitis which is reported more commonly in men than in women, and the etiology of the contributing pancreatitis is almost always alcohol-related.[4] No clear consensus on the mechanism for the formation of the fistulous tract has been reached, and there are diverging theories of the temporality of fistula formation and associated portal venous thrombosis, which is usually present.[4] Some authors suggested that the primary pathogenesis is related to the portal vein thrombosis acting as nidus for fistula formation.[35] Others, however, like Dawson et al. reported a PPVF that existed before portal vein thrombosis, suggesting that it is uninhibited pancreatic enzymes within a pseudocyst causing erosion of the portal venous wall and subsequent fistula formation.[67] It is important to note, however, that not all PPVFs are associated with pancreatic pseudocysts.[5]
Definitive diagnosis of PPVFs in the setting of pancreatitis has proven to be a diagnostic challenge. A review by Rasmussen et al. demonstrated that ERCP was successfully used 14 times for the diagnosis of PPVFs, while cross-sectional imaging was only diagnostic in 4/33 cases.[4] However, this analysis included cases from as early as 1964, before the availability of modern noninvasive imaging techniques such as high-resolution CT and state-of-the-art MRI scans with the availability of heavily T2-weighted MRCP imaging. In a recent retrospective study of 8 cases, Alessandrino et al. demonstrated that all four cases that underwent initial MRCP imaging were correctly diagnosed with PPVFs, while the other four cases which were evaluated initially with CT imaging were diagnosed only with portal vein thrombosis.[3] In 3 of the 4 initially misdiagnosed cases, the PPVF diagnosis was eventually correctly made with MRCP, whereas the remaining fourth case was correctly diagnosed on a follow-up CT.
The characteristic imaging finding of PPVF is a fluid-attenuated portal vein on CT with possible periportal collateral vessels and surrounding pseudocysts.[3] These findings should particularly raise suspicion in patients with additional findings or history of pancreatitis. On MRI including MRCP, a corresponding hyperintense portal vein with the fluid signal within it is often demonstrated on T2-weighted sequences. Direct visualization of a T2-hyperintense fistulous tract may be seen and can be highlighted by the use of three-dimensional rendering techniques.[5] However, not all fistulous communications may be seen by MRI. Ultrasound evaluation likewise demonstrates complex fluid within the portal vein with absent flow on Doppler interrogation.
It is important to recognize potential imaging pitfalls differentiating bland portal vein thrombosis secondary to hypercoagulable state, or extrinsic compression by tumor or lymphadenopathy. Despite the utility of modern noninvasive diagnostic imaging techniques, invasive approaches including ERCP, percutaneous hepatic portography, and operative exploration can establish the diagnosis in cases of diagnostic uncertainty.[35]
Prompt diagnosis and the management of PPVF are of great importance given the severity of potential complications, including portal hypertension due to thrombosis, septic shock, lipolysis, hemorrhage, and death.[389] Systemic lipolysis, hypothesized to be due to the release of pancreatic contents into the systemic circulation through the PPVF, portends a particularly poor prognosis.[9] Due to the relative paucity of reported cases, treatment of a PPVF is generally occurs on a case-by-case basis, which can include strictly supportive medical management, surgical or endoscopic drainage of associated pseudocysts, fistula embolization, or partial pancreatectomy.[345] Surgical intervention can be risky, due to extensive collateralization, with one case report of a patient who underwent a technically successful cystogastrostomy for a large pseudocyst, but arrested postoperatively from massive hemorrhage into the stomach postoperatively thought to be due to elevated portal venous pressures shunting blood through the PPVF.[9]
CONCLUSION
We present a patient with the PPVF in the setting of portal vein thrombosis following an episode of acute on chronic pancreatitis. The diagnosis was established by MRCP and ERCP, and the patient responded to medical management and anticoagulation. While pancreatitis associated PPVF is a very rare entity, it behooves the clinician to remain vigilant in the cases of concurrent pancreatitis and portal vein thrombosis as serious complications can ensue. If portal vein thrombosis is suspected on cross-sectional imaging, MRCP is a reasonable diagnostic next-step for confirmation, followed by ERCP if findings remain equivocal. Treatment decisions should be made on a case-by-case basis with careful consideration of other comorbidities, particularly if surgical intervention is considered.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/4/224247.
REFERENCES
- The management of acute and chronic pancreatitis. Gastroenterol Hepatol (N Y). 2010;6:1-6.
- [Google Scholar]
- Acute pancreatic pseudocyst: Incidence, risk factors, and clinical outcomes. Pancreas. 2012;41:577-81.
- [Google Scholar]
- Clinical and cross-sectional imaging features of spontaneous pancreatic pseudocyst-portal vein fistula. Clin Imaging. 2017;44:22-6.
- [Google Scholar]
- Biliary pancreatic portal fistula as a complication of chronic pancreatitis: A case report with review of the literature. Ups J Med Sci. 2006;111:329-38.
- [Google Scholar]
- Diagnosis of pancreatic duct-portal vein fistula; a case report and review of the literature. J Radiol Case Rep. 2014;8:31-8.
- [Google Scholar]
- Spontaneous pancreatic pseudocyst-portal vein fistula: A rare and potentially life-threatening complication of pancreatitis. Ann R Coll Surg Engl. 2013;95:e7-9.
- [Google Scholar]
- Spontaneous rupture of a pancreatic pseudocyst into the portal vein. Can J Surg. 1995;38:459-63.
- [Google Scholar]
- Massive pancreatic pseudocyst with portal vein fistula: Case report and proposed treatment algorithm. Pancreatology. 2015;15:88-93.
- [Google Scholar]






