Translate this page into:
One Year Primary Patency of Infrapopliteal Angioplasty Using Drug- Eluting Balloons: Single Center Experience at King Hussein Medical Center
Address for correspondence: Dr. Sizeph Edward Haddad, Department of Interventional Radiology, King Hussein Medical Center, Amman, Jordan. E-mail: sizephed@yahoo.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
Conventional percutaneous transluminal angioplasty (PTA) for long lesions in the below-the-knee (BTK) arteries in patients presenting with critical limb ischemia (CLI) has high restenosis rates at 1 year. Our goal is to evaluate whether paclitaxel drug-eluting balloons (DEB) have higher 1 year primary patency rates compared to conventional PTA.
Methods:
This is a single-center, prospective, randomized trial that was conducted from June 2013 to December 2015. The aim of the study was to compare 1 year primary patency rates of DEB and PTA in BTK arteries in CLI patients. Inclusion criteria were patients presenting with CLI (Rutherford class 4 or greater), stenosis or occlusion ≥30 mm of at least one tibial artery, and agreement to 12-month evaluation. Exclusion criteria were life expectancy <1 year, allergy to paclitaxel, and contraindication to combined antiplatelet treatment. Follow-up was performed by clinical assessment, ankle brachial pressure index, Doppler ultrasound imaging, and conventional angiogram if indicated. Primary end point was 1 year primary patency, and secondary end points were target lesion revascularization (TLR) and major amputation. Statistical analysis was performed using Fischer's exact test.
Results:
Ninety-three patients with 106 lesions in the BTK arteries were enrolled in this study. One year primary patency was achieved in 26 (65%) and seven (17%) in the DEB and PTA groups (P = 0.006), respectively. TLR was performed in nine lesions (23%) and 29 lesions (71%) in DEB and PTA groups (P = 0.009), respectively. Major amputations occurred in one limb (2%) and two limbs (4%) in DEB and PTA groups (P = 0.6), respectively.
Conclusion:
Paclitaxel DEB has significantly higher 1 year primary patency rate associated with significantly less TLR than conventional PTA, following endovascular recanalization of BTK arteries in patients presenting with CLI.
Keywords
Balloon angioplasty
critical limb ischemia
peripheral vascular disease

INTRODUCTION
Peripheral arterial disease is a commonly encountered pathology in our practice. In its most advanced stages, patients present with critical limb ischemia (CLI), manifested as ischemic rest pain or tissue loss.[1] CLI is associated with high morbidity and mortality.[23] Mortality rates as high as 20% within 6 months from diagnosis and exceeding 50% at 5 years have been reported for CLI. Below-the-knee (BTK) vessels are commonly involved with extensive atherosclerotic disease in CLI.[2]
Treatment of BTK vascular disease presenting with CLI has progressed over the recent years. The unsatisfactory outcome of medical therapy[4] and the invasive nature of distal bypass surgery resulted in percutaneous revascularization being considered as a first-line strategy in many centers.[56] The aim of such interventions is to increase blood flow to the foot which in turn increases cutaneous oxygen pressure promoting infection clearance and ulcer granulation at a crucial time point.[7]
Percutaneous transluminal angioplasty (PTA) used for recanalization of BTK vessels is limited by the high 12-month restenosis or occlusion rates.[8] The complex pattern of BTK atherosclerosis, characterized by long, calcific steno-occlusive lesions, limits the widespread use of drug eluting stents, which are currently rarely used as a bailout option.[910]
More recently, the introduction of drug-eluting balloons (DEB), used to deliver paclitaxel to target lesions in femoropopliteal vascular disease, has shown promising results, with significant reduction in restenosis rates.[11] Similarly, in the BTK vascular disease, a reduction in restenosis rate has been observed compared with historical controls treated with PTA in different studies.[12]
Our study is a prospective, randomized trial comparing 1 year primary patency rate of DEB (Luminor 14, iVascular, Barcelona, Spain) with conventional PTA (Oceanus 35, iVascular, Barcelona, Spain) in patients with long atherosclerotic lesions of the BTK area presenting with CLI.
METHODS
This study is a single-center, prospective, randomized trial comparing 1 year primary patency rate of DEB (Luminor 14, iVascular, Barcelona, Spain) with standard PTA (Oceanus 35, iVascular, Barcelona, Spain) in patients with CLI treated by endovascular BTK vessels recanalization. The study was carried out after obtaining approval from the medical ethics committee at our institution. The procedure was explained to all patients, as well as the possible complications, and written informed consents were obtained.
During the period from June 2013 to December 2014, all patients presenting with CLI who were planned to undergo angioplasty of at least one BTK vessel, either alone or in addition to a more proximal endovascular recanalization procedure, were assessed for enrollment in our study. Inclusion criteria were patients presenting with CLI (Rutherford class 4 or greater), stenosis or occlusion ≥30 mm of at least one tibial artery, and agreement to 12-month evaluation. Study duration was until December 2015 when the last patient finished his 12 months’ follow-up period.
Exclusion criteria were life expectancy <1 year, allergy to paclitaxel, and contraindication to combined antiplatelet treatment.
Assignment of patients to one of the two study arms was carried out randomly following the angiogram and successful passage of a guidewire across the target lesion.
Contralateral common femoral artery access, with cross-over technique using a 6 Fr sheath, was used in the majority of cases. Ipsilateral antegrade access was only used in few cases where the retrograde technique was contraindicated or failed.
In the DEB group, predilatation of the target lesion with standard balloon (s) was always performed before dilatation with a DEB.
Balloons used in the study ranged in dimensions between 2.5–3.5 mm in diameter and 50–150 mm in length. The appropriate dimensions of balloons were selected to ensure a minimum coverage of at least five mm both proximal and distal to the lesion and a proper ratio of balloon to vessel diameter of 1:1. Inflation time was at least 2 min for both the DEB and PTA arms. In case of flow-limiting dissection or residual stenosis of >30%, a second prolonged dilation of up to three minutes was performed.
Technical success was defined as restoration of direct flow in the target vessel with runoff to the foot and a residual stenosis of 30%.
All hemodynamically significant inflow lesions were treated by standard techniques during the same session before performing the BTK intervention.
In case of bilateral lesions, the contralateral lesions were treated in a separate session to reduce the risk of contrast-induced nephropathy and radiation exposure, maintaining the same randomization arm.
All patients were started on aspirin 100 mg and clopidogrel 75 mg daily for 1 week before the procedure. After sheath insertion, 70 IU/kg heparin was administered through intravenous route. Postintervention dual antiplatelet therapy was continued for at least 12 weeks, followed by 100 mg aspirin daily thereafter.
All patients were scheduled to visit the vascular surgery clinic once every 2 weeks for the first 2 months after their discharge and then every 4 weeks. In these follow-up visits, the patients underwent proper clinical examination, ankle brachial pressure index (ABPI) measurement, and Doppler ultrasound (DUS) imaging.
In case of significant drop in the ABPI ≥0.15, or evidence of significant restenosis or occlusion in the treated segment by DUS that is associated with clinical CLI recurrence, target lesion revascularization (TLR) was performed within 1 week from presentation. TLR was performed initially by angiography and repeat endovascular recanalization and secondarily by surgical bypass procedure if the endovascular procedure failed. Otherwise the patients were not subjected to a new angiogram or TLR.
One year primary patency was achieved whenever significant flow-limiting restenosis or occlusion did not develop. Significant restenosis was defined according to the imaging modality used either by angiography as a reduction in the luminal diameter >50% according to the worst angiographic view within the treated lesion or by DUS as peak systolic velocity ratio ≥2.5 with change of signal character from triphasic proximal to the lesion to monophasic distal to it.
Relevant clinical information was obtained for all patients. Primary end point was 1 year primary patency, and secondary end points were TLR and major amputation. Fischer's exact test was used to compare the preintervention clinical and angiographic characteristics of the patients in both arms of the study and to compare the end points of the study between the two groups. Statistical software package used is SPSS version 20 (IBM, Armonk, NY, USA).
RESULTS
A total of 107 patients were screened for enrollment in the study. Patients who met the inclusion criteria (93 patients) were randomized; 48 patients (54 Lesions) to DEB arm and 45 patients (52 lesions) to PTA arm. The preintervention clinical and angiographic characteristics for patients in both arms of the study were comparable with non-significant differences [Table 1].
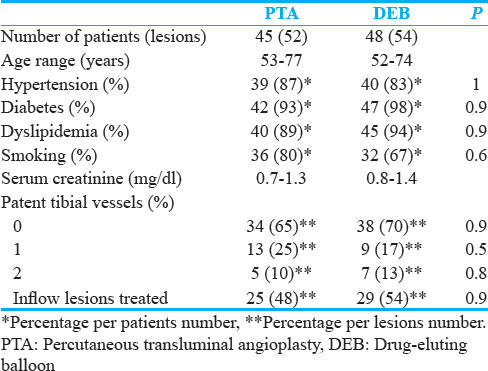
Technical success was encountered in all patients in both groups. The majority of patients had one or no patent tibial arteries at baseline. The most frequently treated vessel was the anterior tibial artery (ATA) in both groups. Almost half of the patients in both study arms underwent inflow lesions treatment. Technical success in the treatment of inflow lesions was achieved in all cases without any complications. During follow-up, there were two inflow lesions in each arm that developed restenosis but were successfully retreated by endovascular means.
Three patients suffered from small groin hematoma which was treated conservatively. No major adverse events occurred during primary hospitalization. Sixteen patients died during follow-up. Causes of death included myocardial infarction (n = 8), stroke (n = 5), and sepsis (n = 3). Major amputations requiring prosthesis for standing and walking occurred in one limb (2%) and two limbs (4%) in DEB and PTA groups (P = 0.6), respectively. None of the remaining 74 patients (37 patients with 40 lesions in the DEB group, and 37 patients with 41 lesions in the PTA group) was lost to follow-up. Clinical and imaging (angiographic or duplex ultrasound) characteristics for patients’ follow-up in both arms of the study are presented in Table 2.

TLR was performed in nine lesions (23%) and 29 lesions (71%) in DEB and PTA groups (P = 0.009), respectively.
One year primary patency rate was achieved in 26 (65%) and seven (17%) lesions in the DEB and PTA groups (P = 0.006), respectively.
With our dual antiplatelet therapy for 12 weeks, no acute thrombosis occurred in both arms of our study.
Angiographic images of one of the patients before and after endovascular recanalization of ATA using DEB are shown in Figures 1 and 2.
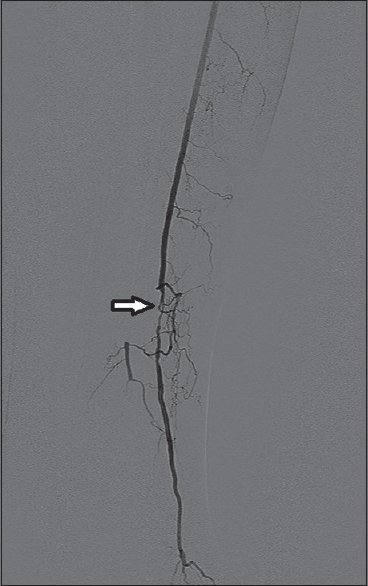
- A 63-year-old male who presented with left lower limb critical ischemia (big toe gangrene). Digital subtraction angiogram image of the left leg showing anterior tibial artery as single arterial run-off below the knee with tight stenosis at its midpart (white arrow).
![Digital subtraction angiogram image of the left leg showing the same anterior tibial artery lesion of [Figure 1] after being successfully dilated using Paclitaxel DEB (white arrow).](/content/12/2017/7/1/img/JCIS-7-31-g005.png)
- Digital subtraction angiogram image of the left leg showing the same anterior tibial artery lesion of [Figure 1] after being successfully dilated using Paclitaxel DEB (white arrow).
DISCUSSION
CLI is classically a disease with grave prognosis. The systemic atherosclerotic burden associated with CLI is reflected by the high mortality rates exceeding those for every other form of occlusive cardiovascular disease, including symptomatic coronary artery disease (CAD).[1314] Besides poor survival rates, prognosis with respect to limb preservation in CLI patients is poor.[15]
Over the past two decades, prognosis with respect to limb salvage and survival in CLI patients has improved, with data showing a decrease in major amputation rates in the CLI population.[1617181920212223] Studies also showed a trend toward more endovascular as compared to surgical revascularization procedures[161820212223] and suggested a potential causal relationship between the increased number of endovascular procedures, especially in the high surgical risk patients, and reduced amputation rates.[1622]
Different endovascular treatment modalities have been used for peripheral vascular recanalization. In the BTK vessels, PTA remained the most widely used method for recanalization but was significantly limited by the high restenosis or occlusion rates.[8]
More recently, DEB has emerged as an effective endovascular modality which is used for recanalization in BTK vessels, with presumably higher patency rates on the long-term. Apart from single-center experiences, there are few organized studies in literature properly assessing this presumption.
In this randomized study, we evaluated the efficacy in terms of 1 year primary patency rate of DEB versus standard PTA in CLI patients undergoing revascularization for BTK arteries.
The results show that DEB achieved significantly higher 1 year primary patency than conventional PTA. Our findings are in concordance with those previously reported in both; a single-center registry[12] that evaluated 3 months’ restenosis in unselected CLI patients treated with the same DEB platform as in our study and those reported in the drug-eluting balloon in peripheral intervention for below the knee angioplasty evaluation study.[24]
TLR is a reflection of early failure of endovascular recanalization and since this failure was found to predict limb loss and poor prognosis[25] and since repeat interventions are harmful in those sick patients with frequent life-threatening comorbidities, thus TLR is an important prognostic factor in CLI patients. In our study, clinically driven TLR was significantly lower in DEB group adding to its advantages.
Major amputation rate was low in both arms in our study due to the dedicated continuous surveillance of the vessel patency and clinical status of the limb associated with rapid reintervention when clinically needed. This emphasizes the long-term benefit of an integrated multidisciplinary framework in those high-risk patients.
Despite higher 1 year primary patency in DEB, there was no significant difference in major amputation rates between the two groups in our study due to the low rate in both groups as mentioned. Besides, vessel patency alone is considered not sufficient to guarantee amputation free-survival.[26]
CONCLUSION
Paclitaxel DEB has significantly higher 1 year primary patency rate associated with significantly less need for TLR than conventional PTA, following endovascular recanalization of BTK arteries in patients presenting with CLI. Larger multicenter randomized trials are needed to assess whether this higher patency will reflect positively on limb salvage which could not be assessed in our study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/31/212075
REFERENCES
- Surgical treatment of peripheral circulation disorders. Helv Chir Acta. 1954;21:499-533.
- [Google Scholar]
- Current state of diagnosis and management of critical limb ischemia. Curr Cardiol Rep. 2012;14:160-70.
- [Google Scholar]
- Long term prognosis of diabetic patients with critical limb ischemia: A population-based cohort study. Diabetes Care. 2009;32:822-7.
- [Google Scholar]
- TASC II document on the management of peripheral arterial disease. Eur J Vasc Endovasc Surg. 2007;33:1-2.
- [Google Scholar]
- Results of the “endovascular treatment first” policy for infrapopliteal disease. J Cardiovasc Surg (Torino). 2012;53(1 Suppl 1):179-88.
- [Google Scholar]
- Endovascular therapy as the primary approach for limb salvage in patients with critical limb ischemia: Experience with 443 infrapopliteal procedures. Vascular. 2006;14:63-9.
- [Google Scholar]
- Superiority of transcutaneous oxygen tension measurements in predicting limb salvage after below-the-knee angioplasty: A prospective trial in diabetic patients with critical limb ischemia. Cardiovasc Intervent Radiol. 2011;34:271-9.
- [Google Scholar]
- Angiographic patency and clinical outcome after balloon-angioplasty for extensive infrapopliteal arterial disease. Catheter Cardiovasc Interv. 2010;76:1047-54.
- [Google Scholar]
- A prospective randomized multicenter comparison of balloon angioplasty and infrapopliteal stenting with the sirolimus-eluting stent in patients with ischemic peripheral arterial disease: 1-year results from the ACHILLES trial. J Am Coll Cardiol. 2012;60:2290-5.
- [Google Scholar]
- Sirolimus-eluting stents for treatment of infrapopliteal arteries reduce clinical event rate compared to bare metal stents: Long-term results from a randomized trial. J Am Coll Cardiol. 2012;60:587-91.
- [Google Scholar]
- Paclitaxel-coated versus uncoated balloon angioplasty reduces target lesion revascularization in patients with femoropopliteal arterial disease: A meta-analysis of randomized trials. Circ Cardiovasc Interv. 2012;5:582-9.
- [Google Scholar]
- First experience with drug-eluting balloons in infrapopliteal arteries: Restenosis rate and clinical outcome. J Am Coll Cardiol. 2011;58:1105-9.
- [Google Scholar]
- One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197-206.
- [Google Scholar]
- The morbidity and mortality following a diagnosis of peripheral arterial disease: Long-term follow-up of a large database. BMC Cardiovasc Disord. 2005;5:14.
- [Google Scholar]
- Suggested objective performance goals and clinical trial design for evaluating catheter-based treatment of critical limb ischemia. J Vasc Surg. 2009;50:1462-73.e1-3.
- [Google Scholar]
- An analysis of the outcomes of a decade of experience with lower extremity revascularization including limb salvage, lengths of stay, and safety. J Vasc Surg. 2010;51:878-885.e1.
- [Google Scholar]
- Outcome of revascularization procedures for peripheral arterial occlusive disease in Ontario between 1991 and 1998: A population-based study. J Vasc Surg. 2003;38:279-88.
- [Google Scholar]
- Trends, complications, and mortality in peripheral vascular surgery. J Vasc Surg. 2006;43:205-16.
- [Google Scholar]
- Major amputation incidence decreases both in non-diabetic and in diabetic patients in Helsinki. Scand J Surg. 2006;95:185-9.
- [Google Scholar]
- National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. 2009;50:54-60.
- [Google Scholar]
- Patterns of treatment for peripheral arterial disease in the United States: 1996 2005. J Vasc Surg. 2009;49:910-7.
- [Google Scholar]
- Emerging national trends in the management and outcomes of lower extremity peripheral arterial disease. Ann Vasc Surg. 2011;25:44-54.
- [Google Scholar]
- Temporal trends and geographic variation of lower extremity amputation in patients with peripheral artery disease: Results from U.S. Medicare 2000-2008. J Am Coll Cardiol. 2012;60:2230-6.
- [Google Scholar]
- Drug-eluting balloon in peripheral intervention for below the knee angioplasty evaluation (DEBATE-BTK): A randomized trial in diabetic patients with critical limb ischemia. Circulation. 2013;128:615-21.
- [Google Scholar]
- Results of second time angioplasty and stenting for femoropopliteal occlusive disease and factors affecting outcomes. J Vasc Surg. 2011;53:651-7.
- [Google Scholar]
- Decreasing incidence of major amputation in diabetic patients: A consequence of a multidisciplinary foot care team approach? Diabet Med. 1995;12:770-6.
- [Google Scholar]






