Translate this page into:
Multiple Osteolytic Lesions
Address for correspondence: Dr. Divya Vinayachandran, No: 95, 4th Avenue, 3rd Cross Street, Sundar Nagar, Ekkatuthangal, Chennai - 600 032, Tamil Nadu, India. E-mail: drdivyavc@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Several systemic diseases initially present with various oral manifestations. Investigation of these oral symptoms may at times lead to the diagnosis of grave underlying life-threatening conditions. We present one such case, where the patient manifested with gross enlargement of the mandible, along with lesions in the lower limbs. These lesions were the initial manifestation and on further investigations the patient was diagnosed with multiple myeloma.
Keywords
Multiple myeloma
osteolytic lesions
maxillofacial lesions
INTRODUCTION

Gammopathy refers to an increased production of one or more classes of immunoglobulins.[1] A monoclonal gammopathy is often a cause for concern, since it signifies an underlying hematological malignancy. Multiple myeloma refers to a malignant proliferation of plasma cells (derived from B-lymphocytes), which produce immunoglobulin with a single heavy and a light chain, a monoclonal protein, referred to as a para-protein. Multiple myeloma accounts for 10% of all hematologic malignancies, and 1% of all cancers and is the most common primary bone tumor.[2]
A 72-year-old male patient presents to the department with a 10-month history of swelling in the mandible. The swelling had gradually increased in size over time with progressive loss of teeth. No associated tenderness was present. He also had a tender swelling in the left lower leg, for the past 6 months. His medical history was unremarkable. On extra-oral examination, a solitary well-defined swelling measuring approximately 9 × 8 cm, was present extending across the midline, in the body of the mandible [Figure 1]. On palpation, it was non-tender and hard. There were no palpable lymph nodes. Intraoral examination revealed multiple mobile teeth in the lower arch, missing lower left canine, and a diffuse swelling was present extending from the left lower second molar to the right lower first molar region, obliterating the buccal and the lingual vestibule [Figure 2]. The surface of the swelling was irregular and lobulated, showing multiple dilated vessels. On palpation, it was nontender, soft to firm in consistency. Another solitary swelling approximately measuring 8 × 5 cm was present in the left lower leg. On palpation, it was nontender, hard, and was not mobile.

- 72-year-old male with a swelling in the mandible and the left lower leg, diagnosed with multiple myeloma. Clinical extraoral view from the front, shows a solitary, well-defined swelling measuring 9 cm × 8 cm in size in the body of the mandible (arrowhead).
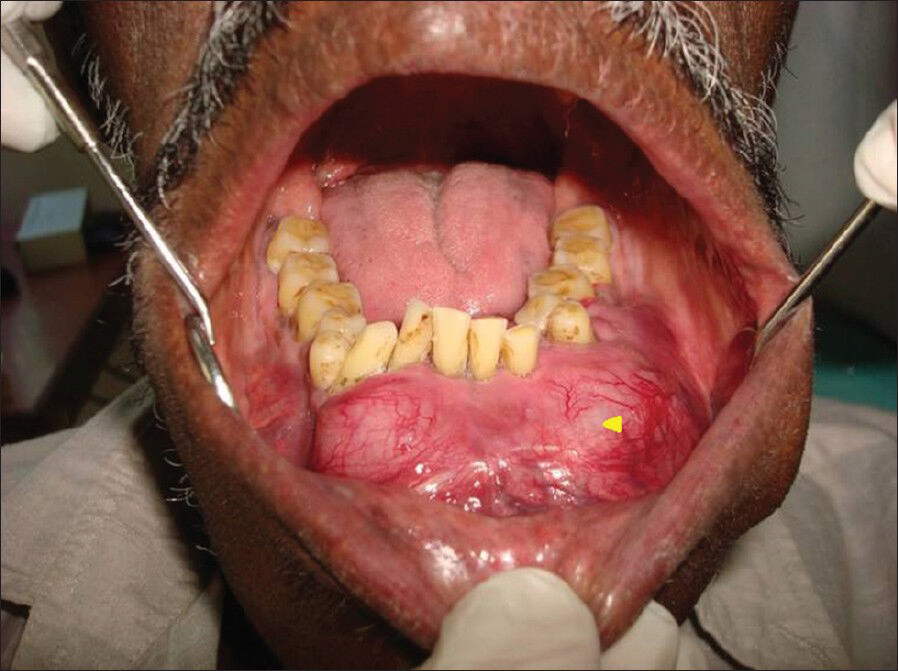
- 72-year-old male with a swelling in the mandible and the left lower leg, diagnosed with multiple myeloma. Clinical intraoral view from the front, shows diffuse swelling extending from the left lower second molar to the right lower first molar region, obliterating the buccal and the lingual vestibule (arrowhead).
RADIOLOGICAL FEATURES
Mandibular cross-sectional occlusal radiograph revealed radiating bony spicules perpendicular to the lower dental arch, missing left canine, and displaced first premolars, and right canine [Figure 3]. The buccal and lingual cortical plates were not visible due to the bony expansion. Panoramic radiography revealed a multilocular radiolucency extending from 4 cm short of the right and left angle of the mandible, across the midline and a missing lower left canine [Figure 4]. Displacement of teeth and resorption of the roots was present. The inferior border of the mandible was thinner, but intact. Computed tomography, axial section revealed a heterogenous lesion in the anterior mandibular body, discontinuity of the buccal cortical plate with radiating bony spicules, suggesting periosteal bone reaction [Figure 5]. There was no expansion or breach in the lingual cortical plate. Conventional radiograph of the lower legs revealed lytic lesions in the left fibula and the right tibia [Figure 6].
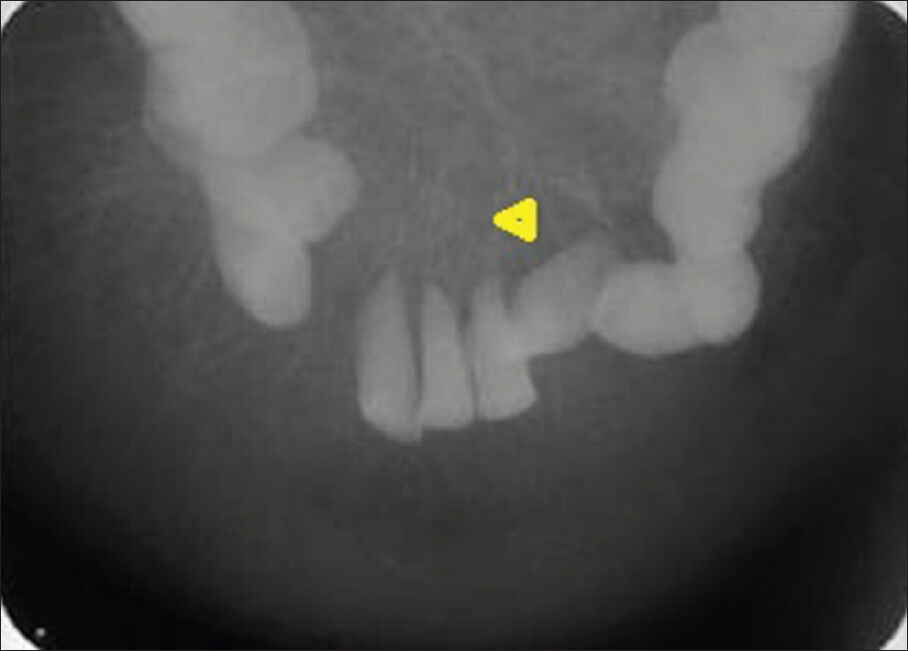
- 72-year-old male with a swelling in the mandible and the left lower leg, diagnosed with multiple myeloma. Conventional mandibular cross-sectional occlusal radiograph reveals radiating bony spicules (arrowhead) perpendicular to the lower dental arch, missing left canine, and displaced first premolars and right canine.
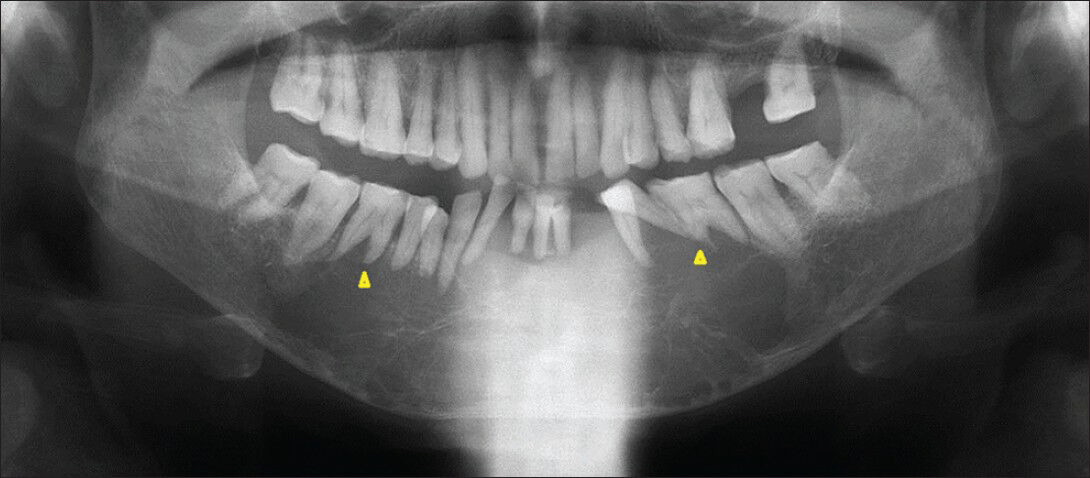
- 72-year-old male with a swelling in the mandible and the left lower leg, diagnosed with multiple myeloma. Conventional panoramic radiography reveals a multilocular radiolucency extending from 4 cm short of the right and the left angle of the mandible, across the midline, missing lower left canine, displacement of teeth, and resorption of the roots (arrowheads).
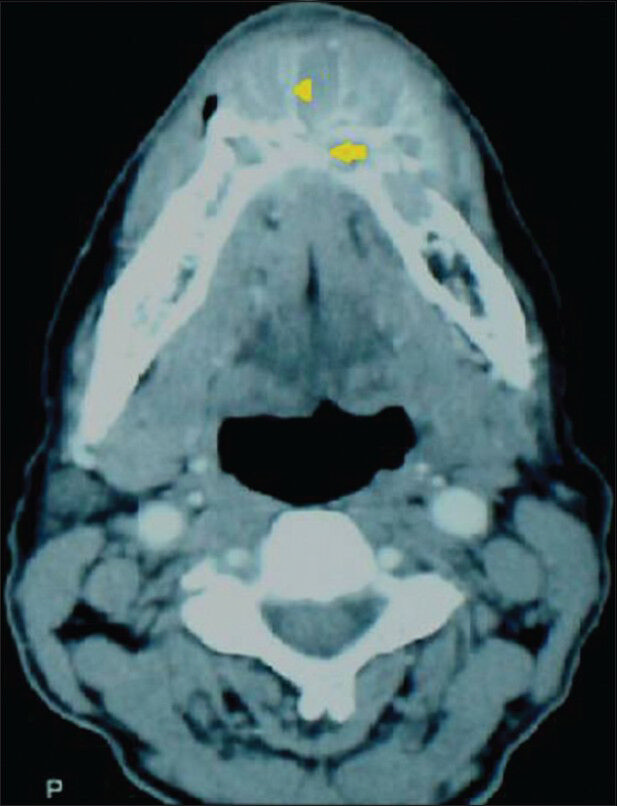
- 72-year-old male with a swelling in the mandible and the left lower leg, diagnosed with multiple myeloma. Computed tomography image, axial section reveals a heterogenous lesion (arrow) in the anterior mandibular body, discontinuity of the buccal cortical plate with radiating bony spicules (arrowhead).

- 72-year-old male with a swelling in the mandible and the left lower leg, diagnosed with multiple myeloma. Conventional radiograph show lytic lesions in the left fibula and the right tibia (arrowheads).
PATHOLOGICAL FEATURES
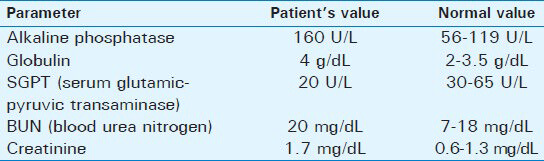
Hematological investigation revealed that with the exception of the parameters listed in Table 1, there were no significant abnormalities.
Histopathological examination following incisional biopsy of the swelling in the left fibula, revealed cellular neoplasm composed of plasma cells [Figure 7a]. Occasional binucleate forms were also seen. Surrounding fibro-fatty and fibrotendinous tissue were also seen along with bone trabeculae. The presence of an abnormal number of plasma cells was suggestive of plasma cell neoplasm. Immunohistochemistry of the bone sample was done to verify the presence and nature of gammopathy. The decalcified sections of bone were taken on slides, which were immersed in 4% chromic acid and coated with aminopropyl ethoxy silane. Sections were deparafinized and subjected to antigen retrieval in ion citrate acid buffer solution, followed by boiling in a microwave oven for 5 min. The solution was allowed to cool to room temperature and washed with tris-buffered saline. Sections were stained with 3,3’-diaminobenzidine substrate chromogen. Immunohistochemistry was positive for CD138 (cluster differentiation) and lambda chain and negative for kappa [Figure 7b and c] chain. This confirmed plasma cell neoplasm with predominance of lambda light chain.
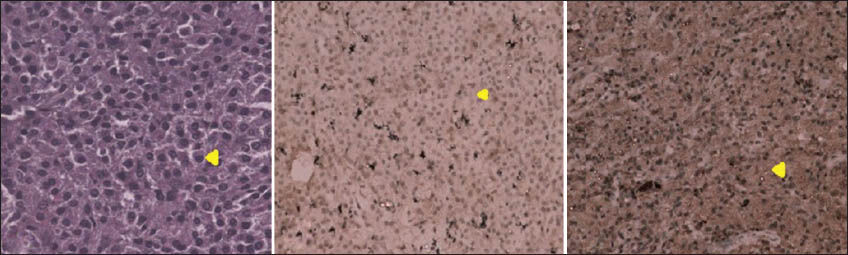
- 72-year-old male with a swelling in the mandible and the left lower leg, diagnosed with multiple myeloma. (a) Hematoxylin and eosin stained section, ×40 view shows cellular neoplasm composed of plasma cells (arrowhead). (b) Immunohistochemistry test shows no kappa light chains (arrowhead). (c) Immunohistochemistry test shows presence of lambda light chains (arrowhead).
On correlating the clinical features and the radiological, hematological, and histopathological findings, the final diagnosis was multiple myeloma. The patient was advised management with chemotherapy.
DISCUSSION
Multiple myeloma is a plasma cell neoplasm, showing a male predilection and the median age of diagnosis is between 60 and 70 years of age.[1] The exact etiology is unknown.[2] Proposed risk factors include old age, male gender, African Americans, radioactivity, positive family history, occupational exposure (e.g., to petroleum products), and obesity. The pathogenesis responsible for different manifestations of the disease spectrum, include neoplastic proliferation of plasma cells within the bone marrow replacing normal cells causing anemia and immunological alterations leading to recurrent infections.[23] There is an increased production of an osteoclast stimulating factor causing bone destruction and fracture, bone pain, and hypercalcemia. Increased para-protein production causes hyperviscosity leading to end-organ damage.
The typical clinical features of multiple myeloma can be summarized by the acronym, CRAB which represents, hypercalcemia, renal insufficiency, anemia, and bone lesions.[4] Other manifestations include, recurrent infections, hyperviscosity induced arterial infarctions and venous thrombosis, neurological impairment, nephrotic syndrome, extramedullary involvement of various organs, concomitant amyloidosis with gastrointestinal symptoms, and soft tissue or solitary bone masses (plasmacytomas).[34]
Oral and maxillofacial features may be the result of local manifestation of a multifocal disseminated disease (multiple myeloma) or a solitary bone plasmacytoma or an extramedullary plasmacytoma.[5] The incidence of oral lesions vary from less than 2% to as high as 70%.[6] Literature review reveals cases presenting with oral manifestations as the initial feature of multiple myeloma with an incidence of 8-15%.[56] Clinical manifestations include swelling, soft tissue masses, mucosal ulceration, jaw pain, tooth ache, tooth mobility and migration, paresthesia following nerve compression, gingival bleeding, pathological fracture, macroglossia due to amyloid deposition, and atypical facial pain.[5678] Burning sensation of the oral mucosa as the only initial manifestation has been reported.[7]
Osseous manifestations constitute an important aspect of multiple myeloma.[8] The skeletal sites most commonly involved are pelvis, skull, spine, ribs, femoral, and humeral shafts. Radiological manifestations in the orofacial region include multiple punched-out radiolucencies, bone expansion causing pathological fractures, periodontal destruction, and dental root resorption.[5] Osteolytic lesions are more common in the mandible, especially in the posterior teeth region, ramus, and condyle, probably due to the increased hematopoietic activity in these areas.[6] They are classified into four types, from Type I to Type IV, ranging from a solitary type, central, or peripheral multiple lytic lesions without marginal sclerosis, diffuse osteoporosis with generalised involvement to diffuse osteosclerosis.[8] Radiological differential diagnosis includes osteomyelitis, metastatic carcinoma, leukemia, lymphoma, and Langerhan's cell histiocytosis.[5] Primary osteosclerosis is a rare entity with an incidence of 3% and is classified into diffuse, focal, and bony spiculation on the surface of the bone and sclerotic reaction along the rim of lytic lesions.[8] A sun-burst appearance, reported in very few cases is considered a rarity, which is seen in the present case. Sun-burst radiographic appearance is also seen in osteosarcoma, chondrosarcoma, Ewing's sarcoma, hemangioma, sickle cell anemia, metastatic tumors, odontogenic myxoma, and thalassemia. An increase in bone density or spicule formation can be explained as a cause, considering that any malignant cell has the potential to induce new bone formation.
Investigations mandatory for a patient suspected to have multiple myeloma include a complete blood count, measuring levels of urea, creatinine, albumin, calcium, electrophoresis of serum and concentrated urine, quantification of nonisotypic immunoglobulins, bone marrow aspiration, immunofixation of serum and urine, and radiographic survey for bone lesions.[9] Conventional plain film radiography of the skeleton are indispensable to assess the extent of bone lesions. Advanced imaging, like positron emission tomography-computed tomography (PET-CT) and magnetic resonance imaging (MRI) are more sensitive for delineating the presence and true extent of the lesion.[10] The diagnostic criteria for multiple myeloma has been given by the International Myeloma Working Group in 2003.[910] The proposed criteria include, presence of a biopsy proven plasmacytoma or clonal bone marrow plasma cells (10% or more), M protein equal to or more than 1 g/dL in the serum and/or equal to or more than 200 mg/day in the urine, myeloma related organ or tissue impairment depicted by bone lesions or hypercalcemia (serum calcium of 11.5 mg/dL or more), renal insufficiency (serum creatinine levels more than 2 mg/dL or estimated creatinine clearance less than 40 mL/min), normocytic normochromic anemia with a hemoglobin value more than 2 g/dL below the normal lower limit or a hemoglobin value of less than 10 g/dL.
Chemotherapy has been indicated only for symptomatic cases and some of the agents used include bortezomib, lenalidomide, thalidomide, melphalan, cyclophosphamide, bisphosphonates, and doxorubicin. Corticosteroids, usually dexamethasone or prednisone, alone or combined with other agents are popularly used.[5] In case of severe disease, multidrug combination chemotherapy have been used.[10] Induction therapy based on dexamethasone, such as VAD (vincristine, doxorubicin and dexamethasone) have been advocated prior to high dose therapy with novel agents. This helps to achieve rapid, high remission rates with minimal toxicity, and preservation of hematopoietic stem cell function.[9] Autologous stem cell transplant has been indicated for improvement in progression free survival following induction therapy. Local radiotherapy has been found to be beneficial in pain control. A dosage of 8 gray (Gy) single fraction is recommended.
Several new treatment options are under development, showing hopeful signs in clinical trials. This includes pomalidomide, carfilzomib, bendamustine, target specific compounds such as fibroblast growth factor receptor 3 and interleukin-6 inhibitors, histone deacetylase inhibitors, and demethylating agents.
Despite various advancements in treatment options, cures for multiple myeloma are rare, with a median survival of approximately 4 years.[9] The probability of complete eradication of the myeloma cells is low, yet cases with stem cell transplantation may survive longer than 10 years.
CONCLUSION
Early diagnosis may facilitate in improving the prognosis of multiple myeloma. As clinical manifestations may often be subtle, meticulous examination and radiological investigation is indispensable. Osteolytic lesions including oral and maxillofacial lesions need to be examined carefully, both radiologically and pathologically, to identify cases of multiple myeloma.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/2/6/117460
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Blood disorders. In: Haslett C, Chilvers ER, Boon NA, Colledge NR, eds. Davidson's Principles and Practice of Medicine (19th ed). Amsterdam: Elsevier; 2002. p. :889-956.
- [Google Scholar]
- Early onset multiple myeloma: An illustrative case report. J Manipulative Physiol Ther. 2007;30:543-9.
- [Google Scholar]
- Beyond the CRAB Symptoms: A study of presenting clinical manifestations of multiple myeloma. Clin Lymphoma Myeloma Leuk. 2010;10:464-8.
- [Google Scholar]
- Medical management update: Multiple myeloma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:599-609.
- [Google Scholar]
- Multiple myeloma presenting as gingival mass. J Maxillofac Oral Surg. 2010;9:209-12.
- [Google Scholar]
- Burning mouth syndrome as the initial sign of multiple myeloma. Oral Oncol Extra. 2004;40:13-5.
- [Google Scholar]
- Abnormal radiological features in a multiple myeloma patient: A case report and radiological review of myelomas. Dentomaxillofac Radiol. 2011;40:513-8.
- [Google Scholar]
- Haemato-oncology Task Force of British Committee for Standards in Haematology (BCSH) and UK Myeloma Forum. Guidelines for the diagnosis and management of multiple myeloma 2011. Br J Haematol. 2011;154:32-75.
- [Google Scholar]
- Multiple myeloma: 2012 update on diagnosis, risk-stratification and management. Am J Hematol. 2012;87:79-88.
- [Google Scholar]






