Translate this page into:
Median Arcuate Ligament Compression of the Celiomesenteric Trunk
Address for correspondence: Dr. Vikram S. Dogra, Department of Imaging Sciences, University of Rochester Medical Center, 601 Elmwood Avenue, Box 648, Rochester, NY 14642-8648, USA. vikram_dogra@urmc.rochester.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Median arcuate ligament (MAL) syndrome is a controversial condition characterized by compression of the celiac trunk and symptoms of intestinal angina. We present a case of MAL compressing the celiomesenteric trunk, a rare variation. We report computed tomography (CT) angiography and three-dimensional reconstructions of this rare phenomenon.
Keywords
Celiomesenteric trunk
CT angiography
median arcuate ligament
INTRODUCTION

Extrinsic compression of the celiac trunk by the median arcuate ligament (MAL) occurs in 10-24% of patients.[1] Although this compression may lead to clinical manifestations of postprandial epigastric pain, nausea or vomiting, and weight loss, it is usually asymptomatic, presumably due to collateral supply from the superior mesenteric circulation.[12] We present a rare case of MAL compression of the celiomesenteric trunk (CMT) diagnosed by computed tomography (CT) angiography, in which a lack of collateral circulation (and subsequent ischemia) is the most likely cause of recurrent abdominal pain.
CASE REPORT
A 26-year-old male with no significant past medical history presented with a 1 year history of intermittent abdominal pain exacerbated by meals that led to an aversion to food and a 25-pound weight loss over the same time period. Main findings on abdominal CT with intravenous (IV) contrast were a segmental thickening and an inflammation of the ascending colon. The patient underwent colonoscopy, which showed a solitary, 2-cm ascending colon ulcer. Multiple biopsies failed to show a clear etiology. The symptoms did not improve with antibiotic administration and the patient was referred for further GI evaluation. A repeat colonoscopy showed no ulcers, but ultrasound and a subsequent CT angiogram (CTA) revealed compression of the celiac axis [Figure 1]. This was confirmed by sagittal [Figure 2] and three-dimensional reconstructions [Figure 3] that showed a common origin of the celiac axis and superior mesenteric artery (SMA) with approximately 70% narrowing, and post-stenotic dilation of the celiac axis and SMA. The patient was referred for vascular surgery and underwent lysis of the MAL, a retroperitoneal aorto-SMA bypass, and a retroperitoneal aorto-celiac bypass. Of note, the patient developed a post-op thrombotic occlusion of the celiac vascular graft [Figure 4]. The SMA graft remained patent and the blood flow was preserved in the distal vessels of the celiac axis. The patient has been advised to continue long term follow-up monitoring of symptoms.
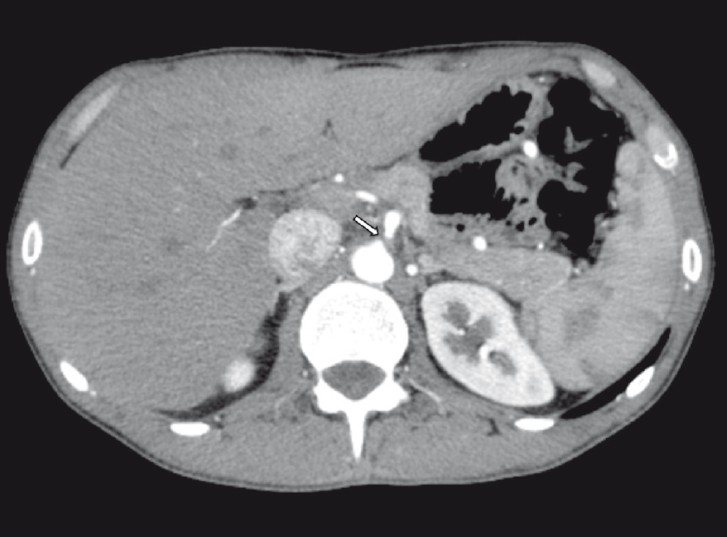
- Axial CTA shows compression of the celiac axis by the median arcuate ligament (arrow).
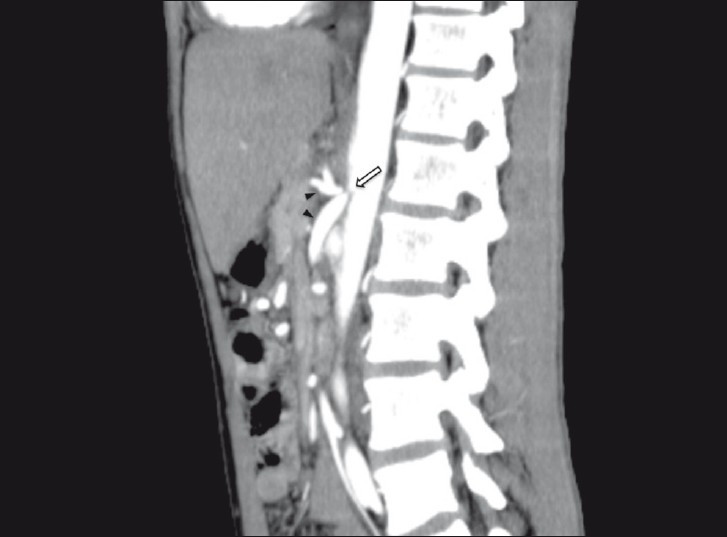
- Sagittal CTA shows compression (arrow) of the celiomesenteric trunk by the median arcuate ligament with post-stenotic dilatation of the celiac and superior mesenteric arteries (arrowheads).
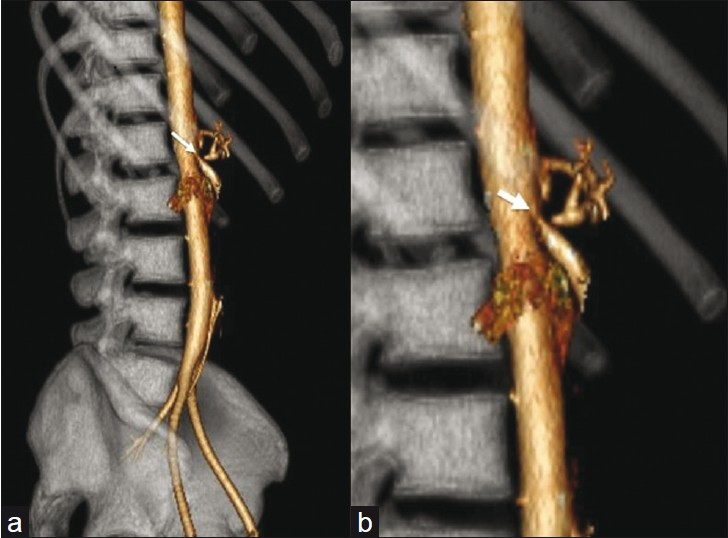
- (a) Sagittal oblique three-dimensional (3D) volume rendered (VR) image of the celiomesenteric trunk (arrow). (b) Magnified view of 3D VR image shows stenosis (arrow) at the origin of the celiomesenteric trunk.
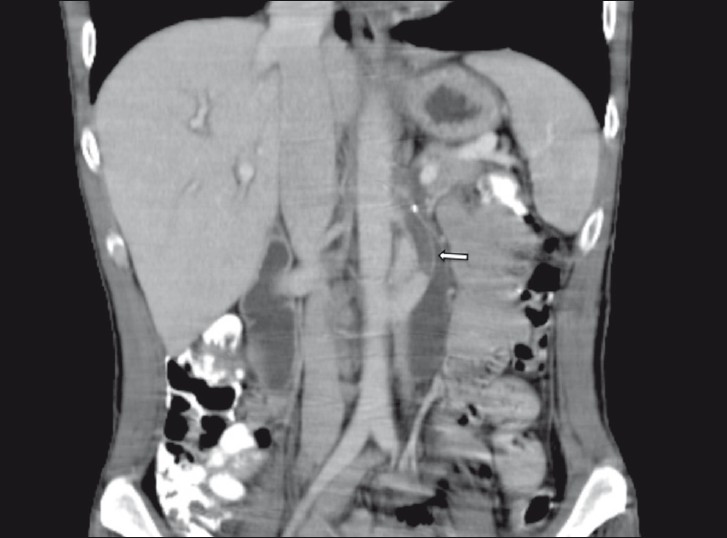
- Coronal CT abdomen with IV contrast (status post bypass surgery), shows thrombotic occlusion (arrow) of the celiac vascular graft.
DISCUSSION
The median arcuate ligament is a fibrous arch that unites the diaphragmatic crura on either side of the aortic hiatus and usually passes over the aorta, superior to the origin of the celiac axis.[1] In 10% to 24% of the population, the ligament may cross over the proximal portion of the celiac axis and cause a characteristic indentation that is usually asymptomatic.[13] Additionally, a small subset of this population may present with MAL syndrome, an anatomic and clinical entity in which extrinsic compression of the celiac axis leads to postprandial epigastric pain, nausea or vomiting, and weight loss (often related to "food fear" or fear of pain triggered by eating).[12] Symptoms are thought to arise from the compression of the celiac axis, resulting in a compromise of the blood flow.[1]
Although characterized several decades ago,[4] the existence of this syndrome is still challenged by several authors.[3] Most celiac compressions actually do not present with symptoms, presumably due to collateral supply from the SMA. Our patient presented with symptoms of chronic, intermittent abdominal pain and significant weight loss along with radiographic findings confirming a compression of the celiac axis by the MAL. Moreover, imaging studies revealed a common origin of the SMA and the celiac artery.
Common CMT is a rare occurrence, estimated to have an incidence of 0.25%[56] of all celiac axis abnormalities. When this anomaly is found, it has a wide-ranging implications. A patient with common CMT is deprived of some of the protective benefits of dual origin vessels with multiple mutually supporting anastomoses.[5] Occlusive disease of a CMT would logically produce symptoms of acute or chronic mesenteric ischemia: the redundancy between the celiac and superior mesenteric arterial circulation is nonexistent in the case of a CMT, and a proximal stenosis affecting this vessel would have serious ischemic consequences to the intestine.[6]
A disease involving the rarely encountered CMT anomaly is extremely uncommon; there is only one other reported case in the literature of symptomatic MAL compression of a CMT diagnosed with conventional angiography.[7]
The CT findings characteristic of MAL compression may not be appreciated on axial images alone. Sagittal plane in CTA is optimal for evaluating the focal narrowing of celiac axis. The focal narrowing has a characteristic hooked appearance that can help distinguish this condition from other causes of celiac artery narrowing, such as atherosclerotic disease. CT may also demonstrate post-stenotic dilation and prominent collateral vessels.[13]
Treatment of MAL syndrome is aimed at restoring normal blood flow in the celiac axis and eliminating neural irritation produced by the celiac ganglion fibers,[2] and has traditionally consisted of laparotomy through an upper abdominal incision, an open division of the MAL, and a resection of associated periarterial neural tissue comprising the celiac plexus or ganglion.[8] In a study by Reilley et al, patients treated with both splanchnic nerve decompression and vessel reconstruction experienced better symptom relief than patients treated with celiac decompression alone.[9] A stenosed or occluded celiac axis on angiography was noted in 75% of patients who presented with persistent symptoms.[89]
In summary, we report the CT findings of a rare case of MAL compression of the CMT, in which the anatomic findings indicate the most likely cause of recurrent abdominal pain and weight loss.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/8/75260
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Median arcuate ligament syndrome: Evaluation with CT angiography. Radiographics. 2005;25:1177-82.
- [Google Scholar]
- Management of median arcuate ligament syndrome: A new paradigm. Ann Vasc Surg. 2009;23:778-84.
- [Google Scholar]
- Ligamentous compression of the celiac axis: CT findings in five patients. AJR Am J Roentgenol. 1991;156:1101-3.
- [Google Scholar]
- A rare obstruction of the coeliac artery: Report of a case. Ann Chir Gynaecol Fenn. 1963;52:547-50.
- [Google Scholar]
- Celiomesenteric anomaly demonstration by multidetector CT and volume rendering. J Comput Assist Tomogr. 2001;25:802-4.
- [Google Scholar]
- Common celiacomesenteric trunk: Aneurysmal and occlusive disease. J Vasc Surg. 2004;40:1040-3.
- [Google Scholar]
- Aneurysm and stenosis of the celiomesenteric trunk: A rare anomaly. J Vasc Surg. 2003;37:679-82.
- [Google Scholar]
- Laparoscopic vs open celiac ganglionectomy in patients with median arcuate ligament syndrome. J Vasc Surg 2010 [In press]
- [Google Scholar]
- Late results following operative repair for celiac artery compression syndrome. J Vasc Surg. 1985;2:79-91.
- [Google Scholar]






