Magnetic Resonance Imaging of Neurosarcoidosis
Address for correspondence: Dr. Daniel T Ginat, 601 Elmwood Avenue, University of Rochester, Department of Imaging Sciences, Rochester, NY 14642, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Neurosarcoidosis is an uncommon condition with protean manifestations. Magnetic resonance imaging (MRI) is often used in the diagnostic evaluation and follow-up of patients with neurosarcoidosis. Therefore, familiarity with the variety of MRI appearances is important. In this pictorial essay, the range of possible patterns of involvement in neurosarcoidosis are depicted and discussed. These include intracranial and spine leptomeningeal involvement, cortical and cerebral white matter lesions, corpus callosum involvement, sellar and suprasellar involvement, periventricular involvement, cranial nerve involvement, cavernous sinus involvement, hydrocephalus, dural involvement, ischemic lesions, perivascular involvement, orbit lesions, osseous involvement, nerve root involvement, and spinal cord intramedullary involvement. Differential diagnoses for each pattern of involvement of neurosarcoidosis are also provided.
Keywords
Brain
MRI
neurosarcoidosis
orbit
skull
spine
INTRODUCTION
Neurosarcoidosis is apparent clinically in only about 5% of patients with sarcoidosis.[1] However, less than 1% of patients have isolated central nervous system involvement.[2] Cranial neuropathy, particularly facial nerve palsy, is the most common presentation. Other presentations of neurosarcoidosis include encephalopathy, peripheral neuropathy, meningitis, seizure, spinal cord dysfunction, and myopathy. Post treatment, up to 87% of neurosarcoidosis cases show resolution on imaging, which also parallels clinical improvement.[3] The goal of this pictorial essay is to present the spectrum of MRI features in biopsy confirmed neurosarcoidosis patients in a pattern-based approach. The differential diagnosis for each pattern of involvement of neurosarcoidosis will also be reviewed.
Leptomeningeal involvement
Leptomeningeal involvement occurs in 40% of patients with neurosarcoidosis.[2] The basilar meninges are most frequently involved. Gadolinium enhancement can be diffuse or nodular on post-contrast T1-weighted magnetic resonance imaging (MRI) [Figure 1].[4] Perivascular spread can be encountered, producing enhancing foci that are remote from the brain surface [Figure 2]. The MRI differential diagnosis includes the conditions listed in Table 1.
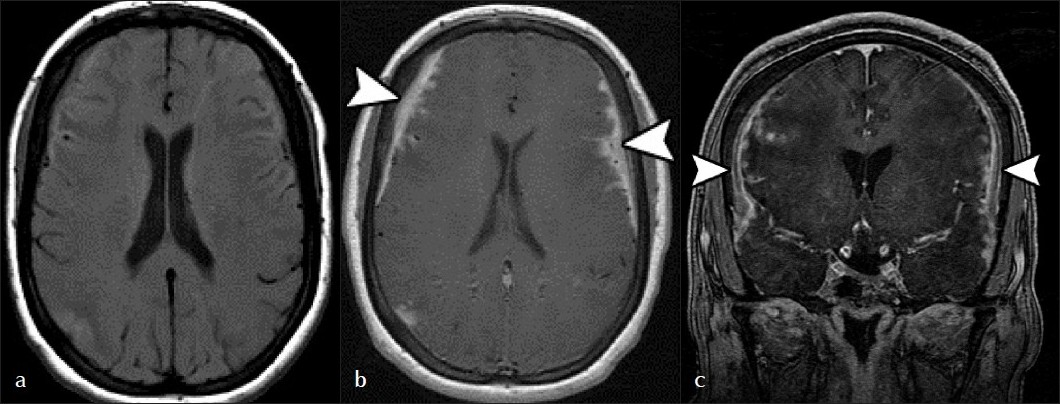
- Leptomeningeal Involvement. (a) Pre-contrast T1, and (b) post-contrast axial, and (c) coronal sequences show widespread leptomeningeal thickening and enhancement along the convexities of the brain (arrowheads). Both diffuse and nodular patterns are evident.

- Perivascular involvement. There are several enhancing foci in the right hemisphere along a perivascular distribution (arrows).

Intraparenchymal mass lesions
Parenchymal mass lesions or granulomas are a fairly common manifestation of neurosarcoidosis, with 35% of cases presenting as multiple supratentorial and/or infratentorial masses and 15% as solitary masses.[4] These lesions are often intimately associated with leptomeningeal involvement and may represent centripetal spread of the disease. Intraparenchymal masses typically show enhancement [Figure 3]. Initially, the lesions can be hypointense on T2,[5] but are otherwise hyperintense. Central necrosis is rare.[2] The MRI differential diagnosis includes the conditions listed in Table 2.

- (a) Axial T2 and (b) post-contrast T1sequences show numerous cortical and subcortical white matter lesions in the bilateral cerebral hemispheres, which are hyperintense on T2 (arrows) and demonstrate enhancement.

Pituitary and hypophyseal involvement
The pituitary gland, infundibulum, or hypothalamus are affected in 18% of patients with neurosarcoidosis.[6] Cystic masses, enhancing masses, or thickening and enhancement of the infundibulum can be encountered on imaging [Figure 4]. These findings may occur in isolation or in combination with basilar leptomeningeal involvement. The MRI differential diagnosis includes the conditions listed in Table 3.
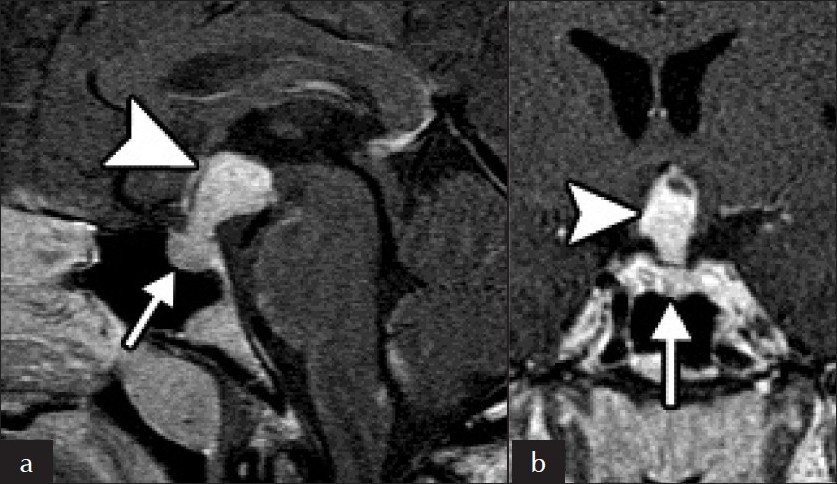
- (a) Sagittal and (b) coronal images of pituitary and hypothalamus Involvement. There is extensive enhancement of the pituitary gland (arrow) and stalk (arrowhead), which is markedly enlarged.

Cavernous sinus involvement
The cavernous sinus is rarely involved in neurosarcoidosis. These lesions can produce cavernous sinus syndrome, which include painful ophthalmoplegia.[7] Lesions enhance and may have a dural tail [Figure 5]. The MRI differential diagnosis includes the conditions listed in Table 4.

- Leptomeningeal Involvement. (a) Pre-contrast T1, and (b) post-contrast axial, and (c) coronal sequences show widespread leptomeningeal thickening and enhancement along the convexities of the brain (arrowheads). Both diffuse and nodular patterns are evident.

Hydrocephalus
Hydrocephalus occurs in 5% to 12% of patients with neurosarcoidosis.[2] The hydrocephalus is usually communicating secondary to leptomeningeal/dural involvement [Figure 6]. However, obstructive hydrocephalus can result secondary to ventricular system adhesions or loculations, which may cause trapped ventricles [Figure 7].[8] There may be altered signal intensities of the cerebrospinal fluid in the isolated ventricle due to elevated protein concentrations.
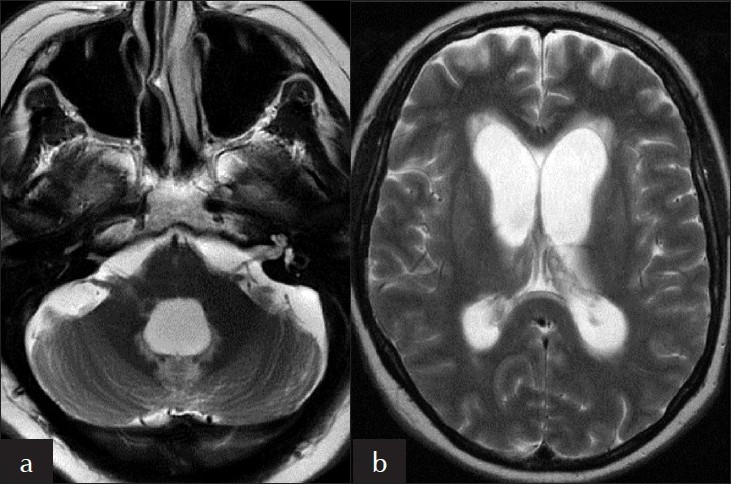
- Hydrocephalus. Axial T2-weighted sequences at the level of the (a) fourth ventricle and (b) lateral ventricles show dilatation of these structures.

- Perivascular involvement. There are several enhancing foci in the right hemisphere along a perivascular distribution (arrows).
Dural involvement
Dural involvement occurs in 34% of patients with neurosarcoidosis.[6] The posterior fossa is most commonly involved. Lesions are usually hypointense or isointense on T2 [Figure 8]. There can be strong enhancement of the thickened dura. The MRI differential diagnosis includes the conditions listed in Table 5.
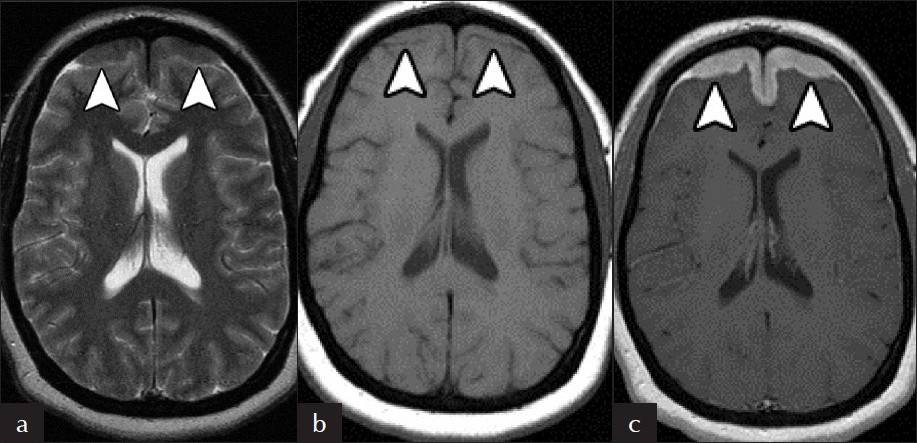
- Dural Involvement. There is (a) hypointense T2 and (b) isointense T1signal in the (c) symmetrically thickened frontal lobe dura, which avidly enhance on post-contrast T1 MRI (arrowheads).

Cranial nerve involvement
Cranial nerves are affected in up to 50% of patients with neurosarcoidosis.[4] There is poor correlation between imaging findings and clinical symptoms. While facial nerve deficits are most commonly found clinically, the optic nerve is the most common cranial nerve to appear abnormal on MRI.[9] Affected cranial nerves show enhancement and thickening with or without associated leptomeningeal involvement [Figure 9]. The MRI differential diagnosis includes the conditions listed in Table 6.
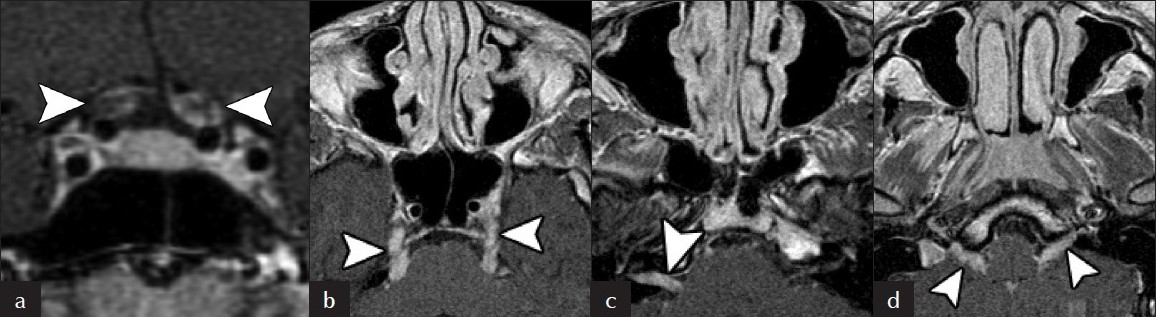
- Cranial nerve involvement. (a) Coronal post-contrast T1-weighted MRI shows peripheral enhancement of the bilateral cisternal segments of cranial nerve II. (b) Axial post-contrast T1-weighted sequences at the level of cranial nerve V, (c) cranial nerves VII and VIII, and (d) cranial nerve IX show thickening and enhancement of multiple cranial nerves (arrowheads).

Lacrimal gland involvement
The lacrimal gland is rarely involved in sarcoidosis. Imaging features on computed tomography (CT) scan include bilateral, asymmetric enlargement with intense enhancement of the lacrimal gland [Figure 10].[10] The gland maintains its anatomic configuration. A portion of the gland may extend medially along anterior border of the globe. MR demonstrates hypointense T1 and T2 signal within enlarged glands that also show intense enhancement. The MRI differential diagnosis includes the conditions listed in Table 7.

- Lacrimal gland involvement. Coronal post-contrast T1-weighted MRI shows bilateral intensely enhancing enlarge lacrimal glands (arrowheads).

Osseous involvement
Although osseous involvement occurs in up to 13% of patients, skull and vertebral involvement in neurosarcoidosis is very rare.[2] The intervertebral body disc spaces can also be affected. Lesions are usually lytic with a punched-out appearance, but can also be sclerotic.[11] The osseous lesions can also show increased activity on bone scans. On MRI, bone lesions are typically hyperintense on T2 and post-contrast T1 [Figure 11]. However, sclerotic lesions appear hypointense and may not enhance [Figure 12]. The MRI differential diagnosis includes the conditions listed in Table 8.
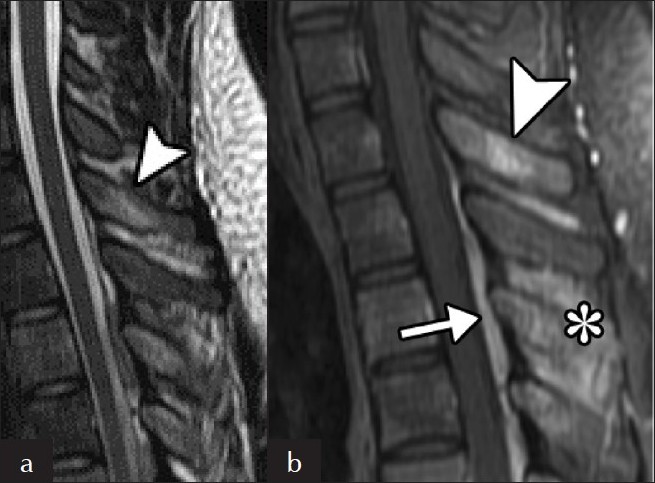
- Vertebral involvement. (a) Sagittal T2 and (b) post-contrast T1 sequences show a hyperintense, enhancing focus on the posterior elements of the thoracic spine (arrowhead). There is also enhancement of the interpinous ligaments (*) and posterior extradural enhancement (arrow).

- Skull Involvement. (a) Sagittal post-contrast T1-weigthed MRI shows multiple non-enhancing hypointense intraosseous skull lesions (arrowheads). (b) The corresponding axial CT image shows that the lesions are sclerotic (arrowheads).

Spine intramedullary involvement
Intramedullary involvement occurs in up to 25% patients with of neurosarcoidosis.[6] Lesions cause fusiform cord enlargement, mainly in the cervical and thoracic regions.[6] Typically, there is low T1 signal, high T2 signal, and patchy enhancement on MRI [Figure 13]. The MRI differential diagnosis includes the conditions listed in Table 9.

- Intramedullary spinal cord involvement. (a) Sagittal T2, (b) sagittal T1 and (c) sagittal post-contrast T1 sequences is high T2 signal within the spinal cord (arrowheads). A portion of the lesion demonstrates intense enhancement (arrowhead). The cord is mildly expanded.

Spine nerve root enhancement
Infiltration of spinal nerve roots is uncommon in neurosarcoidosis.[9] These lesions can cause polyneuropathies. On MRI, nodularity or diffuse thickening of the affected nerve roots can be encountered [Figure 14]. Nerve root enhancement is also a common feature. The MRI differential diagnosis includes the conditions listed in Table 10.

- Spine nerve root involvement. (a) Sagittal T2 and (b) post-contrast T1 sequences demonstrate high T2 signal within the spinal cord (arrowheads). A portion of the lesion demonstrates intense enhancement (arrowhead). The cord is mildly expanded.

Diagnostic Considerations
Although the base of the brain is characteristically involved in neurosarcoidosis, this pictorial essay demonstrates that the MRI manifestations of neurosacroidosis overlap with both benign and malignant entities. Thus, MRI findings of neurosarcoidosis are not sufficiently specific to render a diagnosis, especially when neurological involvement is the first or only finding with sarcoidosis.[1213] Rather, other parameters must be considered, including clinical presentation, other imaging studies, angiotensin-converting enzyme (ACE) assays, the Kveim test, and biopsy, if necessary. Since the majority of patients with neurosacroidosis have preexisting lung involvement, the presence of hilar and mediastinal adenopathy and/or parenchymal disease strongly supports the diagnosis. Serum ACE levels are elevated in up to 50% of neurosacroidosis cases.[7] Similarly, cerebrospinal fluid ACE levels tend to be elevated, although this is not specific for neurosarcoidosis since increased ACE levels can also be encountered with meningitis.[14] The Kveim test is a very sensitive and specific test for sarcoidosis, but is rarely used.[15] It involves intradermal injection of spleen or liver extract from a patient with known sarcoidosis. The test is considered positive if sarcoid granulomas form several weeks later at the injection site. Histopathology of sarcoid lesions classically reveals non-caseating granulomas. Finally, patients with neurosarcoidosis demonstrate improvement in their clinical symptoms when treated with high-dose steroids. Response to steroid treatment can be monitored with MRI [Figure 15].
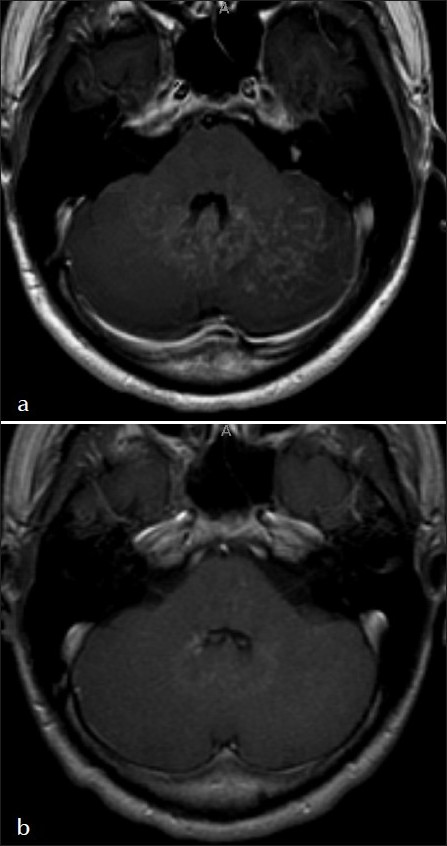
- Treatment response. Axial post-contrast T1 sequences (a) before and (b) after initiation of steroids shows near resolution of the serpiginous cerebellar hemisphere lesions within eight months.
Conclusion
Neurosarcoidosis has a wide spectrum of imaging features that mimic both benign and malignant conditions. Virtually any portion of the central nervous system and associated structures can be affected. MRI is highly sensitive for detecting neurosarcoidosis, but is not specific. Therefore, in the differential diagnosis of this entity the imaging patterns included in this pictorial essay should be considered. Finally, the diagnosis is made by exclusion of other entities using a combination of imaging, diagnostic testing, clinical presentation, and sometimes tissue sampling.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp? 2011/1/15/76693
REFERENCES
- MR of sarcoidosis in the head and spine: Spectrum of manifestations and radiographic response to steroid therapy. AJNR Am J Neuroradiol. 1994;15:973-82.
- [Google Scholar]
- Neurosarcoidosis: A review of its intracranial manifestation. J Neurol. 2001;248:363-72.
- [Google Scholar]
- Sarcoidosis presenting as an intra- or extra-cranial mass: report of two cases. Neuroradiology. 1997;39:516-9.
- [Google Scholar]
- Correlation of MR imaging findings and clinical manifestations in neurosarcoidosis. AJNR Am J Neuroradiol. 2009;30:953-61.
- [Google Scholar]
- Cavernous sinus syndrome due to sarcoidosis: A case report. Acta Neurol Taiwan. 2009;18:37-41.
- [Google Scholar]
- An isolated fourth ventricle in neurosarcoidosis: MRI findings. Eur Radiol. 2002;12:S1-3.
- [Google Scholar]
- MR of CNS sarcoidosis: Correlation of imaging features to clinical symptoms and response to treatment. AJNR Am J Neuroradiol. 1999;20:655-69.
- [Google Scholar]
- Radiologic manifestations of sarcoidosis in various organs. Radiographics. 2004;24:87-104.
- [Google Scholar]
- Sclerotic lesions of the cervical spine in sarcoidosis. Skeletal Radiol. 1998;27:702-4.
- [Google Scholar]
- Angiotensin I-converting enzyme in cerebrospinal fluid and neurosarcoidosis. Ann Biol Clin (Paris). 2005;63:475-80.
- [Google Scholar]
- Central nervous system sarcoidosis: Diagnosis and management. Q J Med. 1999;93:103-17.
- [Google Scholar]






