Translate this page into:
Isolated Partial Anomalous Pulmonary Venous Connection: Development of Volume Overload and Elevated Estimated Pulmonary Pressure in Adults

*Corresponding author: Satvik Cholenahalli Manjunath,Department of Cardiology, Sri Jayadeva Institute of Cardiovascular Sciences and Research, Phase 3, Jayanagar 9th Block, Bengaluru, Karnataka-560 069, India. satvikacademic@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Hegde M, Manjunath SC, Usha MK. Isolated partial anomalous pulmonary venous connection: development of volume overload and elevated estimated pulmonary pressure in adults. J Clin Imaging Sci 2019;9:29.
Abstract
Objective
Partial anomalous pulmonary venous connection (PAPVC) is one of the rare congenital cardiac diseases with a prevalence of 0.4–0.7% of autopsies. The prevalence of a partial anomalous pulmonary venous connection is 0.2% in computed tomography (CT) among adults. We chose to study the association between isolated PAPVC and volume overload, estimated systolic pulmonary artery pressure in a tertiary care center for cardiovascular diseases.
Methods
CT report database was searched for keywords of partial anomalous pulmonary venous connection, pulmonary hypertension, dilated right atrium (RA), and right ventricle (RV). Both pediatric and adult population were considered. All the dedicated studies of non-coronary cardiac evaluation, pulmonary arteries, and thorax were included in the study. Echocardiography was performed in all the subjects. In adults, abnormalities searched were features of volume overload of RA and RV and estimated systolic pulmonary pressure of 45 mmHg. Biphasic studies were performed, and upper abdomen was included in the CT studies.
Results
Among the 110 subjects, 54 (49%) had isolated PAPVC. Of 54, 26 patients had volume overload of RA/RV or elevated estimated systolic pulmonary artery pressure. There is a significant association between drainage of anomalous veins to superior vena cava (SVC) and age >18 years (Chi-squared test P = 0.003). Among patients with isolated PAPVC, 18 had anomalous drainage to the SVC. Among isolated PAPVC cases, 38 were of the age >18 years. We found statistically significant association (P = 0.02) between isolated PAPVC in adults and pulmonary hypertension.
Conclusion
Isolated PAPVC has association with the development of pulmonary hypertension in adults, approaching statistically significant p value. Because isolated PAPVC is a clinically significant independent risk factor, it should be actively treated to prevent the development of pulmonary hypertension later in life, which may result in severe clinical consequences.
Keywords
Partial anomalous pulmonary venous connection
Right heart volume overload
Congenital heart disease
INTRODUCTION
Partial anomalous pulmonary venous connection (PAPVC) is a rare congenital cardiac disease with a prevalence of 0.4%–0.7% in autopsies.[1,2] The prevalence of PAPVC in adults was 0.2% on computed tomography (CT) scans.[3] Occasionally, pulmonary hypertension due to PAPVC is misdiagnosed as primary/idiopathic pulmonary arterial hypertension (PAH).[4] In many instances, PAPVC manifests as an incidental finding in adults. PAPVC is one of the common causes of treatable PAH. Moreover, the associations of PAH with many other congenital cardiovascular diseases are well known. However, the natural history of isolated PAPVC remains unestablished. In the present study, we examined the association between isolated PAPVC and volume overload and estimated systolic pulmonary artery pressure in a tertiary care center for cardiovascular diseases.
We hypothesized that isolated PAPVC involving vein drainage in a single lobe of the lung parenchyma is not a risk factor for volume overload on the right-sided cardiac chambers and increased estimated systolic pulmonary artery pressure.
PATIENTS AND METHODS
This study was approved by the institutional review board. A CT database was searched for the following keywords: “Partial anomalous pulmonary venous connections,” “pulmonary hypertension,” “dilated right atrium (RA),” and “right ventricle (RV).” Both pediatric and adult populations were considered. The inclusion criterion was the availability of CT images and medical charts. All studies on the non-coronary cardiac evaluation, pulmonary arteries, and thorax were included in the study. All 122 symptomatic patients in whom PAPVC was incidentally detected were included in the study. Of these 122 patients, 12 were excluded due to the presence of coexisting lung parenchymal diseases (six patients), suboptimal quality of imaging (three patients), and non-availability of contrast-enhanced studies (three patients). Finally, 110 patients were enrolled in this study.
In the pediatric population, electrocardiographic gating was not performed, except in cases where the main purpose of CT was to examine coronary arteries. Both adults who underwent and did not undergo electrocardiographic gating were included in the study. In patients whom PAPVC was suspected before performing CT, the coverage extended from the thoracic outlet to the superior portion of the abdomen. A power injector was used in patients of all age groups, including neonates, to ensure a uniform contrast. The dosage ranged from 1.0 to 1.5 mL/kg of body weight.
Echocardiography (ECG) was performed in all patients. In adults, the following abnormalities were searched: Volume overload of the RA and RV (chamber size in B mode) and an estimated systolic pulmonary pressure of 45 mmHg, derived from the tricuspid regurgitation jet. A right atrial short axis measurement of >45 mm in four chambers and a right ventricular basal short axis (diastolic) measurement of >45 mm were considered as indicators of volume overload.
CT studies were repeated in three patients due to suboptimal quality of the first CT imaging. Two of these three patients were children, and studies were rendered non-diagnostic due to the presence of movement artifacts. The third patient was an adult, and the study was considered suboptimal due to the presence of contrast-related artifacts in relation to superior vena cava (SVC). Biphasic studies were performed, and the upper abdomen was included in these studies. Associated abnormalities were detected, and isolated PAPVC cases were marked. Anomalous connections were analyzed in terms of their numbers, number of lobes, and segments of lungs involved and the site of the abnormal connection. Patients’ age; age at the onset of symptoms, if any; and age when concerned findings were detected on ECG were documented. Patent foramen ovale was observed in three patients. However, it was ignored because its size was <3 mm. A CT scan was obtained using the bolus-tracking technique. Volumetric data were obtained from vessels in the axial plane and were reconstructed in sagittal and coronal planes.
CT studies were reviewed for the location, size, and drainage site of the anomalous vein; presence or absence of a pulmonary vein in the normal location; cardiac size and configuration; and pulmonary arteries. Clinical charts were reviewed for evidence of pulmonary and cardiovascular diseases, history of congenital heart disease, and results of other cardiac imaging studies.[3]
RESULTS
Of 110 patients, 88 had anomalous vein draining from the right upper lobe segments. Of 22 patients who had anomalous connections only on the left side, 4 had left upper lobe pulmonary vein involvement and 18 had left lower lobe involvement. The atrial septal defect was associated in 18 (16.3%) patients. Of these 18 patients, 2 had abnormal drainage from the left lower lobe and the remaining 16 had anomalous right pulmonary vein drainage.
Among 110 patients, 54 (49%) had isolated PAPVC. Of these 54 patients, 26 had volume overload of the RA or RV or elevated estimated systolic pulmonary artery pressure. Of these 26 patients, 11 had anomalous pulmonary venous drainage involving only one lobe. Among these 110 patients, 70 (63.6%) were aged >18 years. A significant association was found between the drainage of anomalous veins to the SVC and patients’ age of >18 years (Chi-square test P = 0.003). 18 patients with isolated PAPVC had anomalous drainages only to the SVC. The remaining patients with isolated PAPVC had either a mixed pattern (supracardiac and cardiac) or pure cardiac drainage pattern. Among patients with isolated PAPVC, 38 were aged >18 years and 2 were infants. Among 38 adults who had isolated PAPVC, 14 had dilated main pulmonary artery. Among all patients who had PAPVC, six were infants and two of them did not have any associated abnormality. Two patients developed symptoms at the age of 17 years. We found a statistically significant association (P = 0.02) between isolated PAPVC involving vein drainage in a single lobe of the lung parenchyma in adults and volume overload on the right cardiac chambers.
Correlation between age and number of lobes:
A moderate downhill correlation (r = -0.43) was observed between age and the number of lobes in all patients with isolated PAPVC.
An approaching severe downhill correlation (r = -0.52) was observed between age and the number of lobes in isolated PAPVC patients with volume overload.
A weak downhill correlation (r = -0.14) was observed between age and the number of lobes in PAPVC patients with other congenital cardiovascular abnormalities.
A weak downhill correlation (r = -0.23) was observed between age and the number of lobes in all patients with PAPVC, including those with isolated PAPVC and those with other congenital cardiovascular anomalies.
Statistical methods
R Version 3.3.1 software and Microsoft Excel were used to analyze data. The Chi-square test was used to examine the association between patients with isolated PAPVC and volume overload and between volume overload and the site of drainage. Pearson’s correlation coefficient was used to examine the correlation between age (in years) and the number of lobes. Microsoft Excel was used to draw a scatter plot.
DISCUSSION
In a previous case series on this uncommon cardiovascular condition, 9% of cases were reported to have isolated PAPVC, and the mean age of the pediatric population was 5 years.[5] Considering the low prevalence of PAPVC, our sample size of 38 patients with isolated PAPVC is one of the largest presented thus far. PAPVC is a rare cause of volume overload in adults.
The right-sided cardiac volume overload due to PAPVC can manifest from early childhood to late adulthood with a varying spectrum of severity. Isolated PAPVC is very rare, and 97% of patients with isolated PAPVC have a right upper lobe PAPVC to the SVC.[6] In our study, 62 of 110 patients with PAPVC and 28 of 54 patients with isolated PAPVC were women. Among 110 patients, 76 (69.1%) had right-sided involvement, 22 (20%) had left anomalous vein drainage, and 12 (10.9%) had bilateral involvement. Among 54 patients with isolated PAPVC, 32 (59.2%) had right unilateral involvement [Figures 1 and 2a, b], 12 (22%) had left unilateral involvement [Figures 2c and 3], and 10 (18.6%) had bilateral involvement.
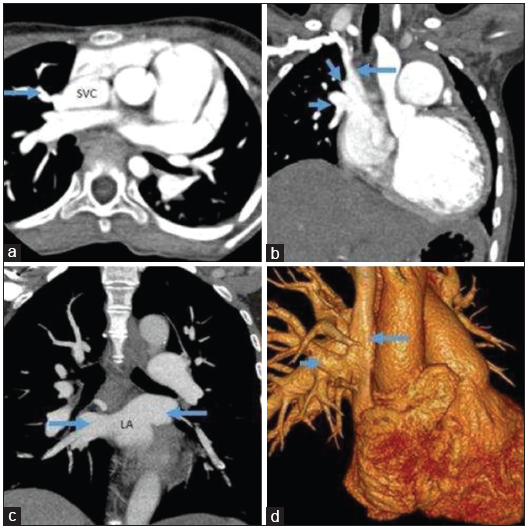
- (a) Right upper lobe pulmonary vein (arrow) draining into the right lateral aspect of the SVC. (b) Right upper and middle lobe pulmonary veins (short arrows) draining into the lower aspect of the SVC (long arrow). (c) Right middle and lower and left pulmonary veins (arrows) draining normally into the left atrium (different patient). (d) VR image showing a right upper lobe vein (short arrow) draining into the SVC (long arrow) in the same patient as in Figure 1c.
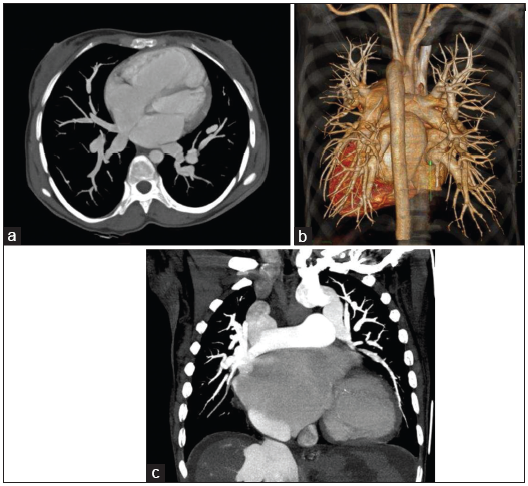
- (a and b) Right middle and lower pulmonary vein anomalously draining into the RA. (c) Left anomalous veins draining into the ascending vertical vein that joins the left innominate vein (different patient).
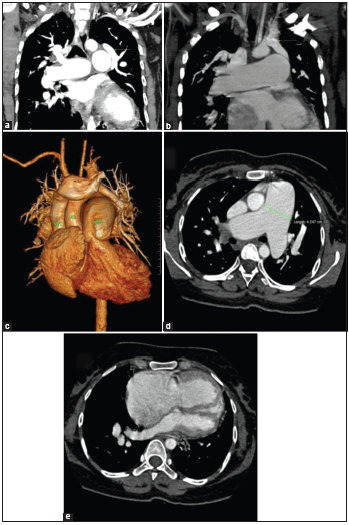
- Left anomalous pulmonary vein draining into a left innominate vein (a-c) with dilated MPA (d) and dilated RA and RV (e).
Unilobar, bilobar, and trilobar involvement were observed in 25.9%, 51.8%, and 18.6% of patients with PAPVC, respectively, and 42.3%, 34.6%, and 23.1% of patients with isolated PAPVC, respectively. Unilobar involvement was the most common pattern among patients who had dilated right-sided cardiac chambers or elevated estimated pulmonary artery pressure. In our study, 11 (78.5%) of 14 patients who had a unilobar pattern, 9 (64%) of 14 patients who had a bilobar pattern, and 6 (60%) of 10 patients who had a trilobar pattern had dilated right heart chambers or elevated estimated pulmonary arterial pressure [Tables 1 and 2]. This finding indicates that a simple linear relationship does not exist between the number of pulmonary lobes involved and the development of right-sided cardiac volume overload and the subsequent development of PAH. The right upper lobar involvement was the most common pattern in our study.
| Number of lobes | Number of patients | With volume overload/elevated estimated systolic pulmonary artery pressure (side of the involved segment) | Without volume overload/elevated estimated systolic pulmonary artery pressure (side of involvement) |
|---|---|---|---|
| 1 lobe | 14/38 (36.8%) | 11 (7-R,4-L) | 3 (3-L) |
| 2 lobes | 14/38 (36.8%) | 9 (7-R, 2-Both) | 5 (4-R, 1-L) |
| 3 lobes | 10/38 (26.6%) | 6 (2-R, 4-Both) | 4 (2-R, 2-Both) |
| Type | Right | Left | Right + Left | Total |
|---|---|---|---|---|
| Overall PAPVC patients | 76 (69.1%) | 22 (20%) | 12 (10.9%) | 110 |
| Isolated PAPVC patients | 32 (59.2%) | 12 (22.2%) | 10 (18.6%) | 54 |
| PAPVC patients in association with other cardiac anomalies | 44 (78.6%) | 10 (17.8%) | 2 (3.6%) | 56 |
| Isolated PAPVC patients with volume overload/elevated estimated systolic pulmonary artery pressure | 16 (61.5%) | 4 (15.4%) | 6 (23.1%) | 26 |
| Isolated PAPVC patients without volume overload/elevated estimated systolic pulmonary artery pressure | 16 (57.1%) | 8 (28.6%) | 4 (14.3%) | 28 |
In some patients, pulmonary hypertension can develop in childhood and adolescence.[7,8] In our study, no isolated PAPVC patients with volume overload belonged to the pediatric age group.
The average age at the time of PAPVC detection was 44.8 and 19.8 years in patients with isolated PAPVC and PAPVC patients with other associated anomalies, respectively. The mean age at detection was 50.8, 44.3, and 34.6 years in patients with unilobar, bilobar, and trilobar anomalous vein involvement, respectively. These findings indicate an association between age at onset of pulmonary hypertension and the number of anomalous veins involved.
In our study, age at onset of symptoms was determined based on associated medical conditions. None of our patients had any serious medical comorbidity. However, we did not consider systemic hypertension in our study, which can be a limiting factor. In patients with isolated PAPVC, 14 had SVC as the site of drainage, 2 had RA drainage, and 6 had innominate vein drainage. None of our patients had an obstruction in anomalous veins.
The most important factor that determines the onset of signs and symptoms is the number of anomalous veins.[9] However, we found only a moderate association between the number of abnormal veins and age at detection, indicating the presence of many other factors that affect volume overload.[10] We believe that additional molecular mechanisms (endothelin mediated) also contribute considerably to the development of pulmonary hypertension, in addition to the volume of shunted blood. A future study on the histopathological characteristics of the lung parenchymal tissue may throw more light on cellular components, leading to the development of pulmonary hypertension.
Another factor is the specific type of lobes involved. In general, in an upright position, blood pools in the right middle and lower lobes and the left lower lobe. Hence, anomalous veins involving these lobes tend to shunt more blood volume and thus have a high tendency to cause pulmonary hypertension. However, in our study, we observed that anomalous venous drainage in the right upper lobe was the most common pattern associated with the development of volume overload. We found a significant association between isolated PAPVC and right-sided volume overload (P = 0.02).
A single-center study including 43 adult patients reported that PAPVC involving a single pulmonary vein has a benign course and does not require surgical intervention.[11] In our study, all patients who developed signs of volume overload or elevated estimated pulmonary arterial pressure were adults. Studies have suggested that surgery should be considered when a significant left-to-right shunt (Qp: Qs of approximately 2:1 or more) is present or when an entire lung anomalously drains.[9,12]
Majdalany et al. suggested that PAH increases with aging in cases of isolated PAPVC.[11] Saalouke et al. were the first to report the presence of PAH in isolated PAPVC because two of their five patients with this congenital heart condition had PAH with markedly increased pulmonary vascular resistance.[13]
Sogomonian et al. reported a case of supracardiac PAPVC that caused right heart failure.[14] Sahay et al. concluded that patients with PAPVC had normal pulmonary artery pressure unless at least two pulmonary veins had an anomalous return.[15] They found no statistical difference in the right ventricular systolic pressure before and after corrective surgery. Babb et al. reported a possible association of PAPVC with an intact atrial septum and development of pulmonary hypertension.[16]
With the increased use of CT and magnetic resonance in cardiothoracic imaging, the diagnosis rate of isolated partial anomalous pulmonary venous drainage involving a single lung parenchymal lobe has increased.[10] This adds additional responsibility on radiologists to determine the likelihood of developing clinically significant hemodynamic changes. Patients with this anomaly should be followed at regular intervals so that timely therapeutic intervention can be administered and unwarranted ones can be avoided.[17]
Limitations
The findings of CT were not compared with those of catheter angiography or peroperative findings. Long-term follow-up data were not available. The intrinsic limitations of a retrospective study form the second set of limitations. True and false negatives (patients with negative CT scans) were not considered in the study. The findings of this study do not represent the clinical characteristics of the general population because the cohort size is not adequate to extrapolate the findings to the general population, although PAPVC is a rare disease.
CONCLUSION AND CLINICAL IMPLICATION
Isolated PAPVC involving a single pulmonary lobe can cause right-sided cardiac volume overload and development of pulmonary hypertension in adults. The presence of a partial anomalous venous connection should be actively searched through cross-sectional imaging, such as CT, and follow-ups at regular intervals. The number of pulmonary lobes involved and the source of shunted blood among these lobes have only a moderate association with age at the development of the right cardiac chamber overload, indicating the importance of other possible unknown factors contributing to the development of pulmonary hypertension.
Acknowledgment
Authors thank Dr. C. N. Manjunath for his guidance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Drainage of pulmonary veins into the right side of the heart. Arch Pathol. 1942;33:221-40.
- [Google Scholar]
- An anatomic survey of anomalous pulmonary veins: Their clinical significance. J Thorac Surg. 1952;23:433-4.
- [Google Scholar]
- Computed tomography of partial anomalous pulmonary venous connection in adults. J Comput Assist Tomogr. 2003;27:743-9.
- [CrossRef] [PubMed] [Google Scholar]
- Role of pulmonary angiography in congenital heart diseases among children. Natl J Med Res Print. 2013;3:332-7.
- [Google Scholar]
- Dual-source 256-MDCT for diagnosis of anomalous pulmonary venous drainage in pediatric population. AJR Am J Roentgenol. 2013;200:W163-9.
- [CrossRef] [PubMed] [Google Scholar]
- MDCT of partial anomalous pulmonary venous return (PAPVR) in adults. J Thorac Imaging. 2009;24:89-95.
- [CrossRef] [PubMed] [Google Scholar]
- Partial anomalous pulmonary venous return presenting with adult-onset pulmonary hypertension. Pulm Circ. 2012;2:250-5.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated left-sided partial anomalous pulmonary venous connection in a child. Turk Kardiyol Dern Ars. 2017;45:545-8.
- [CrossRef] [PubMed] [Google Scholar]
- Partial Anomalous Pulmonary Venous Connection. Available from https://www.emedicine.medscape.com/article/897686-overview (accessed )
- Anomalous pulmonary veins return In: Moodie DS, ed. Clinical Management of Congenital Heart Disease from Infancy to Adulthood (1st ed). Minneapolis: Cardiotext Publishing; 2013. In:
- [Google Scholar]
- Isolated partial anomalous pulmonary venous connections in adults: Twenty-year experience. Congenit Heart Dis. 2010;5:537-45.
- [CrossRef] [PubMed] [Google Scholar]
- Left-sided partial anomalous pulmonary venous connection should diagnosis lead to surgery? Interact Cardiovasc Thorac Surg. 2010;11:847-8.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated partial anomalous pulmonary venous drainage associated with pulmonary vascular obstructive disease. Am J Cardiol. 1977;39:439-44.
- [CrossRef] [Google Scholar]
- Id: 5: Isolated supra-cardiac partial anomalous pulmonary venous connection causing right heart failure. J Invest Med. 2016;64:918-9.
- [CrossRef] [Google Scholar]
- Partial anomalous pulmonary venous connection and pulmonary arterial hypertension. Respirology. 2012;17:957-63.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated partial anomalous venous connection: A congenital defect with late and serious complications. Ann Thorac Surg. 1981;31:540-1.
- [CrossRef] [Google Scholar]
- CRT-800.50 natural history of isolated partial anomalous pulmonary venous connection with intact inter-atrial septum. JACC Cardiovasc Interv. 2017;10:S77.
- [CrossRef] [Google Scholar]






