Translate this page into:
Intramedullary Neurocysticercosis Mimicking Cord Tumor

*Corresponding author: Kamlesh Jobanputra, Department of Radiology, University of Texas Southwestern Medical Center, Dallas, Texas, United States. Kamlesh.Jobanputra@UTSouthwestern.edu
-
Received: ,
Accepted: ,
How to cite this article: Jobanputra K, Raj K, Yu F, Agarwal A. Intramedullary neurocysticercosis mimicking cord tumor. J Clin Imaging Sci 2020;10:7.
Abstract
Isolated spinal intramedullary involvement by neurocysticercosis is extremely rare. We report a case of a Hispanic female with right-sided weakness, magnetic resonance imaging showing cervical intramedullary lesion. Surgery was performed due to the progressive nature of symptoms. The cervical cord lesion was completely removed; pathology was consistent with degenerated cysticercosis. Progressive clinical improvement with physiotherapy was achieved. Although rare, especially in the absence of intracranial lesions, the diagnosis should be considered in appropriate patient population as it usually presents a peripherally enhancing cystic lesion.
Keywords
Spinal intramedullary neurocysticercosis
Peripherally enhancing cyst
Ependymoma
Scolex
Vesicular
Colloid vesicular
Vesicular nodular
Nodular calcified
INTRODUCTION
Neurocysticercosis (NCC) is the most common parasitic central nervous system (CNS) infection, endemic in developing countries such as Mexico, Central and South America, parts of Africa, and the Indian subcontinent; however, spinal involvement is rarely seen and accounts for about 1.2–5.8% of all cases.[1] Intramedullary cysticerci are even more uncommon.[2] We report a case of isolated intramedullary cysticercosis mimicking a primary cord neoplasm requiring surgery for the progressive nature of the symptoms.
CASE REPORT
A previously healthy 44-year-old Hispanic woman, with a remote surgical history relevant for excision of thigh lipoma was seen in the outpatient department with right upper limb pain and hand numbness consistent with myelopathy which prompted magnetic resonance (MR) evaluation of the cervical spine which revealed an intramedullary expansile lobulated partially cystic intramedullary lesion at C5-C7 measuring 9 mm × 11 mm × 20 mm eccentrically located on the right side with surrounding non-enhancing edema around the lesion extending superiorly up to foramen magnum and inferiorly to the level of T1-T2. No enhancing nodule was noted. An inferior lobulated portion of lesion showed a peripheral hypointense rim on T2-w images [Figures 1 and 2]. The imaging characteristics were consistent with a primary neoplasm such as an ependymoma. The patient was referred to neurosurgery for evaluation. A complete MR evaluation of the craniospinal axis showed no additional lesions. About a month later, the patient presented to emergency department with worsening pain and myelopathy and the patient underwent C5-C7 laminectomy with complete resection of the lesion [Figure 3]. It was well encapsulated with well- defined planes. It expressed some yellowish content that appeared mucinous. Histopathology was consistent with a degenerated cysticercal cyst. The myelopathy improved with physiotherapy.
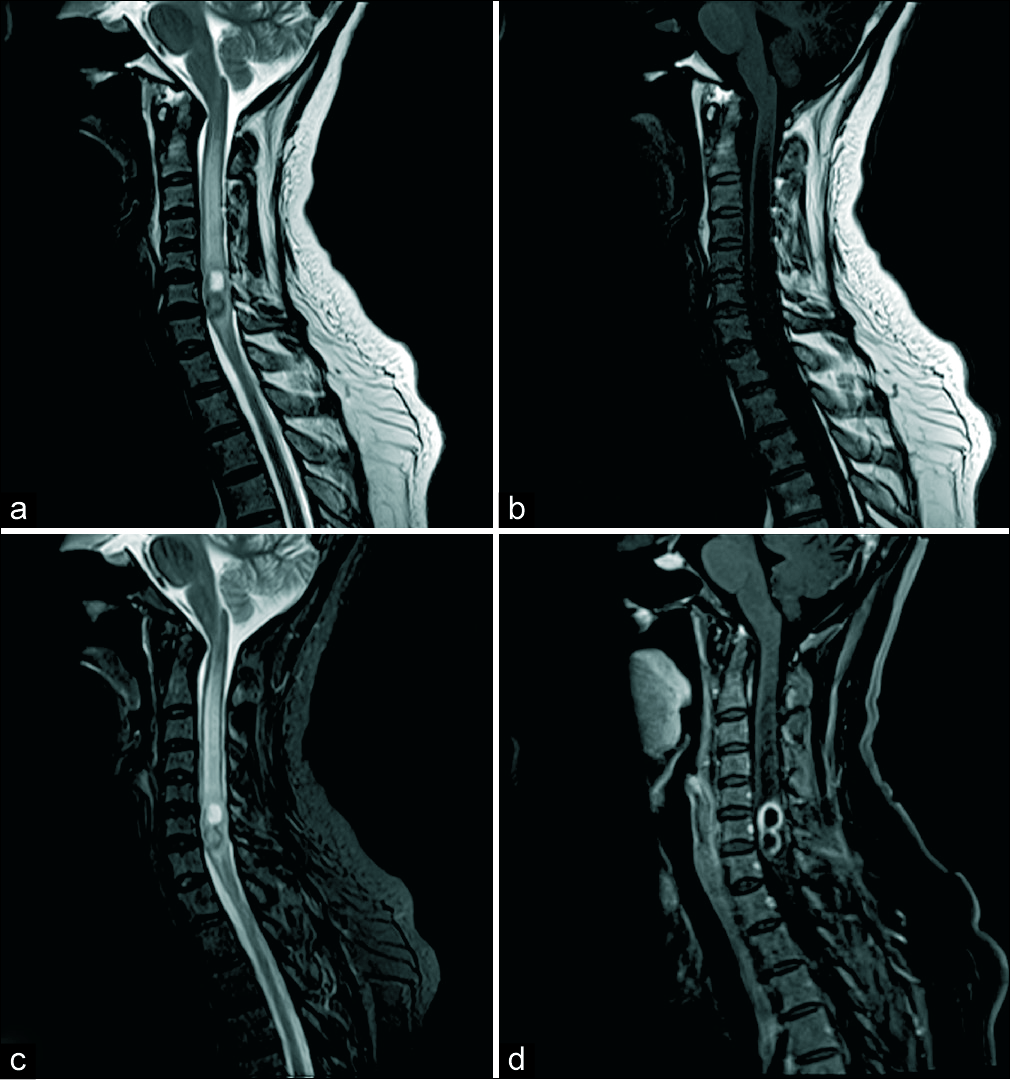
- (a) Sagittal T2 turbo spin-echo (TSE) image showing intramedullary lesion at C5, C6 with extensive surrounding cervical cord hyperintense signal. The lesion appears lobulated with the superior component appearing hyperintense and lower component showing an intense hypointense rim, (b) sagittal T1 TSE image showing the superior component hypointense and the lower component isointense to the cord parenchyma, (c) sagittal T2 FS image, and (d) post-contrast sagittal FS image showing peripheral rim enhancement of the lobulated lesion.

- (a) T2 turbo spin-echo axial images through the superior component and (b) through the inferior component show findings similar to sagittal images, the inferior component shows thicker hypointense rim; (c and d) axial T1 FS post-contrast images showing peripheral rim enhancement.
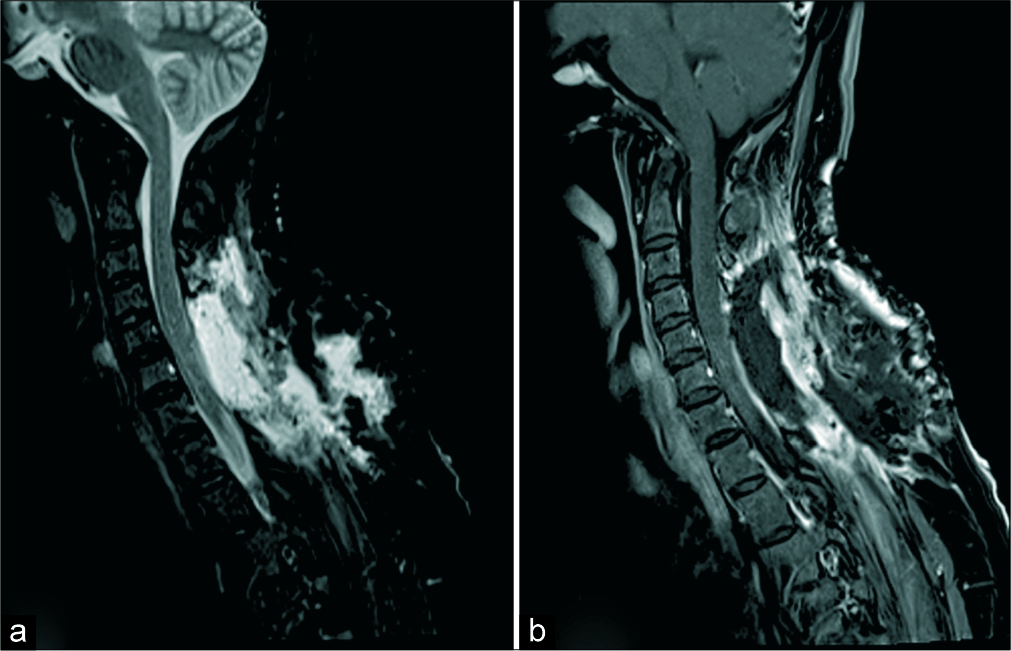
- Post-operative T2 FS (a) and sagittal T1 FS (b) images. Post-surgical changes in the cervical region. No intramedullary lesion is seen. The cord signal has improved.
DISCUSSION
Cysticercosis is a parasitic infection caused by cestode Taenia solium (pork tapeworm), the humans being intermediate dead-end hosts. It affects approximately 50 million people worldwide and has a prevalence of 3–6% in endemic regions including Central and South America, Eastern Europe, Africa, and the Indian subcontinent.[3] It is increasingly seen in the United States due to influx of immigrants from endemic regions.[2,4,5]
Cysticercal infection occurs after ingestion of eggs by humans (undercooked pork and unclean vegetables). Embryos released in the small intestines invade the bowel wall to reach the vascular system and then lodge preferentially in the subcutaneous tissues, skeletal muscles, ocular globes, and neural tissues. In the CNS, the oncospheres develop into secondary larval form called cysticerci. The larval stage may disseminate throughout all CNS compartments. Cysticerci cellulosae which has a scolex characteristically seen in brain parenchymal and rarely spinal intramedullary lesions while the racemose variety usually lacking a scolex grows as grape- like clusters of thin-walled cysts in the subarachnoid space, the latter may become large and reach more than 10 cm in size.[2]
Spinal extradural lesions are extremely rare. Leptomeningeal involvement is 6–8 times more common than the intramedullary form and is presumably due to larval migration from the intracranial compartment to the spinal subarachnoid space.[3] Intramedullary forms like brain parenchymal lesions typically arise from hematogenous dissemination, usually in the thoracic spinal cord and are reported in 1.2–5.8% of patients with NCC.[3]
The clinical features of cysticercosis are often nonspecific depending on the location, number and inflammation associated with the cysts. Inflammation usually ensues larval degeneration causing perilesional edema and mass effect, leptomeningitis, and vascular compromise and resulting focal neurological symptoms.[2]
While scolex can usually be seen in the parenchymal lesions with high resolution T2-w images like CISS, MR imaging of intramedullary cysticercosis is nonspecific in the absence of scolex.[2,3] Concomitant intracranial lesions can help establish a diagnosis. The diagnosis of isolated intramedullary lesions can be challenging, and the differentials include variety of cysts and neoplastic, inflammatory, demyelinating, vascular, and granulomatous lesions.[3] While there are many case reports of intramedullary cysticercosis in various locations Qazi et al.,[5] Qi et al.[6] describing it in dorsal cord, Guedes-Corrêa et al. in the conus region,[7] Singh and Sahai in the cervicodorsal region,[8] and Torabi et al. describing multilevel intramedullary lesions,[1] all the case reports describe lesions as cysts with cerebrospinal fluid (CSF) intensity and thin enhancing peripheral wall consistent with cyst degeneration. Our case is different, in that it has a more pronounced T2 hypointense component showing peripheral enhancement mimicking tumor, classically an ependymoma [Figures 1 and 2]. The T2 hypointense signal could be due to the lower component of the lesion in a more advanced stage of NCC with coarse mineralized granules [Figure 4]. Although the chronic nodular calcified lesions do not usually enhance, the peripheral enhancement of this component possibly represents an intermediate stage in the cyst evolution between granular nodular and nodular calcified. Various stages of intracranial NCC have previously been described and classically represent vesicular, colloid cystic, granular nodular, and nodular calcified stages;[2] however, these have not been described in spinal intramedullary lesions. Typically, in the colloid vesicular stage the cyst may show T1 signal that is hyperintense to CSF and a rim of T2 hypointensity which enhances. As inflammation increases, the cyst contents become opaque. A granuloma forms around the cyst, first as a cellular infiltrate within the cyst and then fully formed with an inner epithelioid cellular layer. Over time, the cyst becomes more disorganized with varying degrees of cyst remnants including recognizable cyst membranes and/or membranous-like ribbons, characteristic calcareous corpuscles, and varying degree of inflammatory reaction.[9]
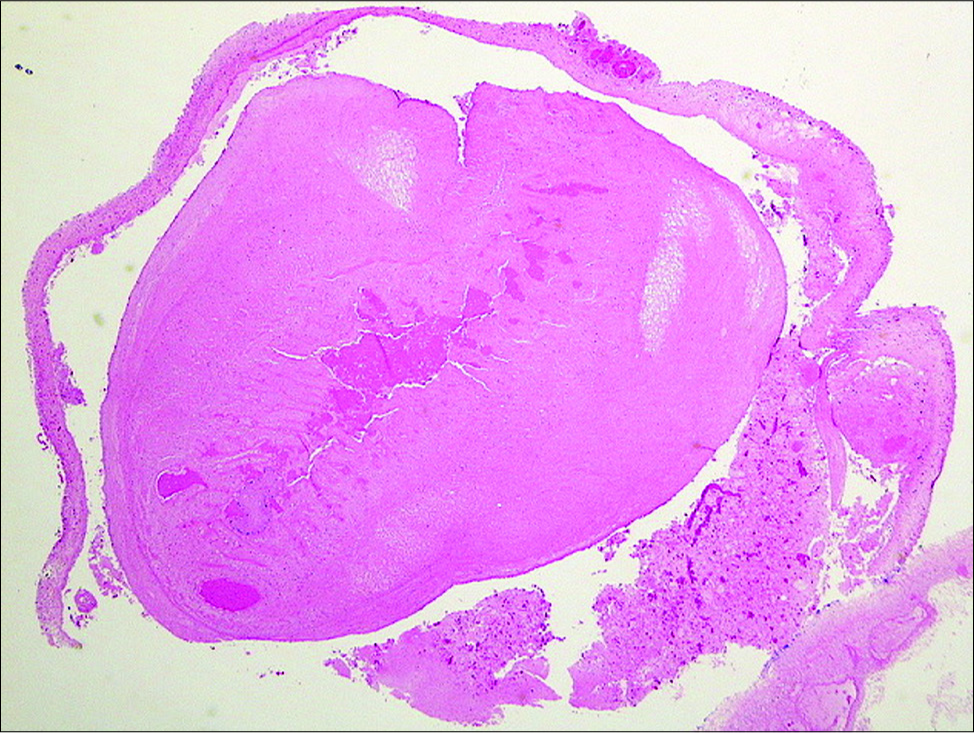
- Hematoxylin and eosin stain showing degenerated cysticercus. The superior component in the early stage of degeneration, the scolex shows hyaline degeneration. The lower component is a more advanced stage, the wall is thickened and the scolex is transformed in coarse mineralized granules.
The therapeutic options for spinal NCC depend on the neurological status. Due to the limited size of the spinal canal, the mass effect and cord edema from the cyst are not well tolerated and clinically the consequences could be devastating. Medical therapy is considered in patients with stable and non-progressive symptoms when the diagnosis is made by CSF, serum immunoelectric antibody assay, or concomitant intracranial lesions. However, severe symptoms, progressive deterioration, missed or uncertain diagnosis, and failed medical therapy should be treated with surgery which not only helps confirm the diagnosis but also prevents permanent damage.[10] Our patient successfully underwent cyst excision and the myelopathy improved with physiotherapy.
CONCLUSION
Although rare, NCC should be considered in patients with isolated spinal intramedullary lesions in appropriate patient population. While imaging features of spinal NCC are not specific and tend to follow intracranial lesions, atypical features have not been well described in the literature and can closely mimic neoplasms. Our case is an excellent example of such a lesion which was treated with a successful outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Multilevel intramedullary spinal neurocysticercosis with eosinophilic meningitis. Arch Neurol. 2004;61:770-2.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of neurocysticercosis. Neuroimaging Clin N Am. 2012;22:659-76.
- [CrossRef] [PubMed] [Google Scholar]
- Neurocysticercosis: evaluation with advanced magnetic resonance techniques and atypical forms. Top Magn Reson Imaging. 2005;16:127-44.
- [CrossRef] [PubMed] [Google Scholar]
- Neurologic parasitic infections in immigrants and travelers. Semin Neurol. 2011;31:231-44.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated intramedullary spinal cord cysticercosis. J Neurosci Rural Pract. 2014;5:S66-8.
- [Google Scholar]
- Spinal intramedullary cysticercosis: A case report and literature review. Int J Med Sci. 2011;8:420-3.
- [CrossRef] [PubMed] [Google Scholar]
- Intramedullary spinal cysticercosis simulating a conus medullaris tumor: case report. Arq Neuropsiquiatr. 2006;64:149-52.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of neurocysticercosis. Nat Rev Neurol. 2011;7:584-94.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of neurocysticercosis: 2017 clinical practice guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH) Clin Infect Dis. 2018;66:e49-e75.
- [CrossRef] [PubMed] [Google Scholar]






