Translate this page into:
Intralobar Pulmonary Sequestratıon as an Unusual Cause of Recurrent Hemoptysis
Address for correspondence: Dr. Servet Kayhan, Department of Pulmonary Disease, Ondokuz Mayis University, School of Medicine, Samsun, Turkey. E-mail: kayhanservet@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pulmonary sequestration is an embryonic, cystic lung tissue that is supplied by systemic blood circulation. It is a nonfunctional lung parenchyma unconnected to normal tracheobronchial system. In cases of pulmonary sequestration, surgical interventions should be performed in order to prevent possible complications such as massive hemoptysis and infections. Preoperative imaging and treatment planning should be done carefully. We present an uncommon case of recurrent hemoptysis caused by intralobar pulmonary sequestration located in the left lower lobe.
Keywords
Bronchopulmonary sequestration
hemoptysis
thoracic surgery
INTRODUCTION

Pulmonary sequestration refers to malformation of the primitive embryonic nonfunctional cystic lung tissue that is supplied by aberrant systemic artery and not connected to the normal tracheobronchial tree. Selective angiography or computed tomographic angiography reveals the anomalous arterial supply and venous drainage of the sequestration. We report a pulmonary sequestration case as a very rare cause of recurrent hemoptysis.
CASE REPORT
A 26-year-old female patient admitted to our clinic with complaints of cough and mild shortness of breath had an 8-year history of recurrent hemoptysis. Physical examination was normal except for the coarse crackles heard in the lower regions of the left lung. There was no abnormality seen in the laboratory investigations. Pulmonary function tests showed forced vital capacity (FVC): 2.65 l (90% of predicted value), forced expiratory volume in 1 s (FEV1): 2.28 l (86.5% of predicted value), and FEV1/FVC: 96%. These were nearly normal spirometric values. Arterial blood gas analysis (at room air) parameter was found to be normal; pO2: 98.0 mmHg, pCO2: 37.6 mmHg, pH: 7.38, and SaO2: 98%. Contrast-enhanced spiral computed tomography (CT) of the thorax revealed an aberrant vascular structure extending from thoracic aorta to lower left lung and 5 mm in diameter [Figures 1 and 2]. We observed increased mucosal vascularization, micro-hemorrhagic foci, and secretions from left lower lobe (LLL) bronchus during fiber optic bronchoscopic examination. Thoracic aortography confirmed the pulmonary sequestration and aberrant arterial vessel from aorta to LLL and venous drainage from sequestrated area to the left atrium [Figure 3].
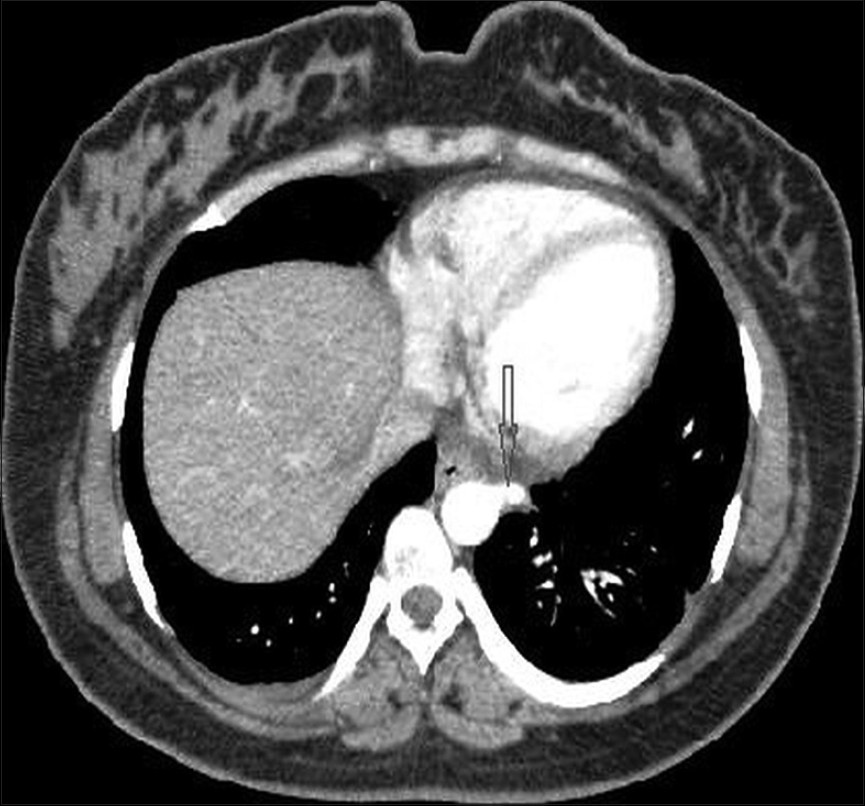
- Intralobar pulmonary sequestration. A 26-year-old woman with recurrent hemoptysis. Contrast-enhanced spiral computed tomography (CT) shows the aberrant artery (arrow) originated from thoracic aorta and introduced to lower left lobe of the lung.

- Computed tomography image of the lung shows small intralobar sequestrated area as bronchiectasis (arrow) in the left lower lobe (LLL).
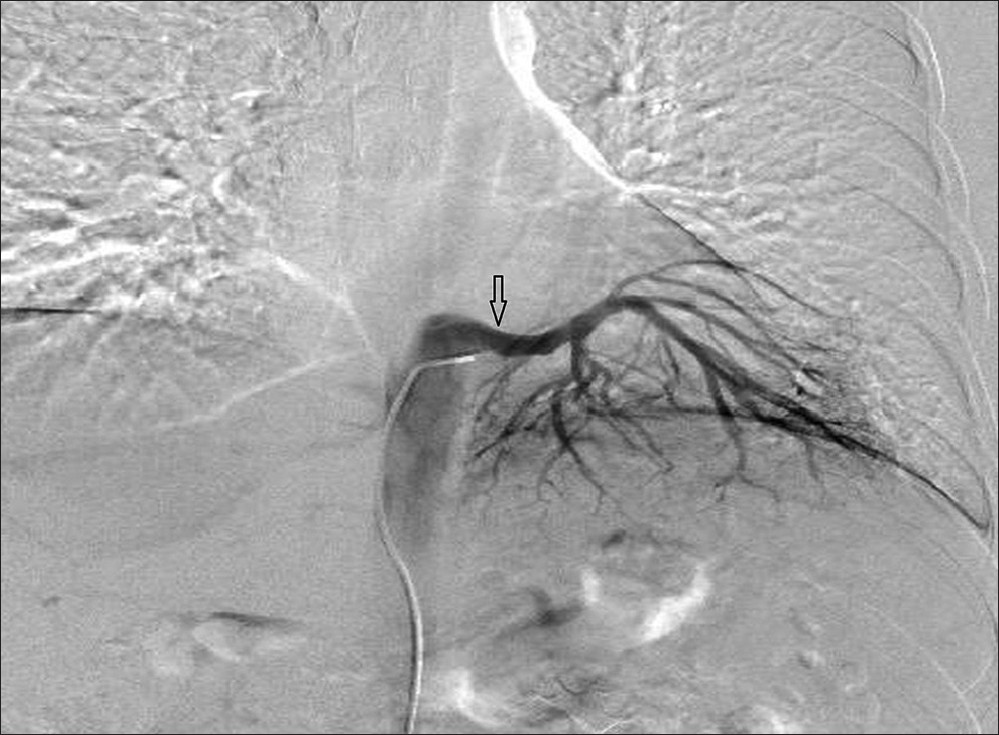
- Aortography image reveals the aberrant arteries (arrow). The anomalous artery originates from the distal part of the thoracic aorta and supplies the blood circulation of the sequestrated lung tissue.
The left posterolateral thoracotomy was performed and the sequestered tissue was found at the baseline of the LLL of the lung [Figure 4]. Dissection starting from the pulmonary ligament was done and aberrant systemic vascular structures were detected and ligatured with 3/0 prolene. Subsequently, the standard lower lobectomy was performed. Pathological examination of the lung tissue revealed intralobar (ILS) sequestrated lung with focal intra-alveolar hemorrhages (IAH), parenchymal hemorrhages (PH), and vascular congestions [Figure 5]. Postoperatively, the patient did not have any clinical and radiological problems and was discharged 7 days after surgery.
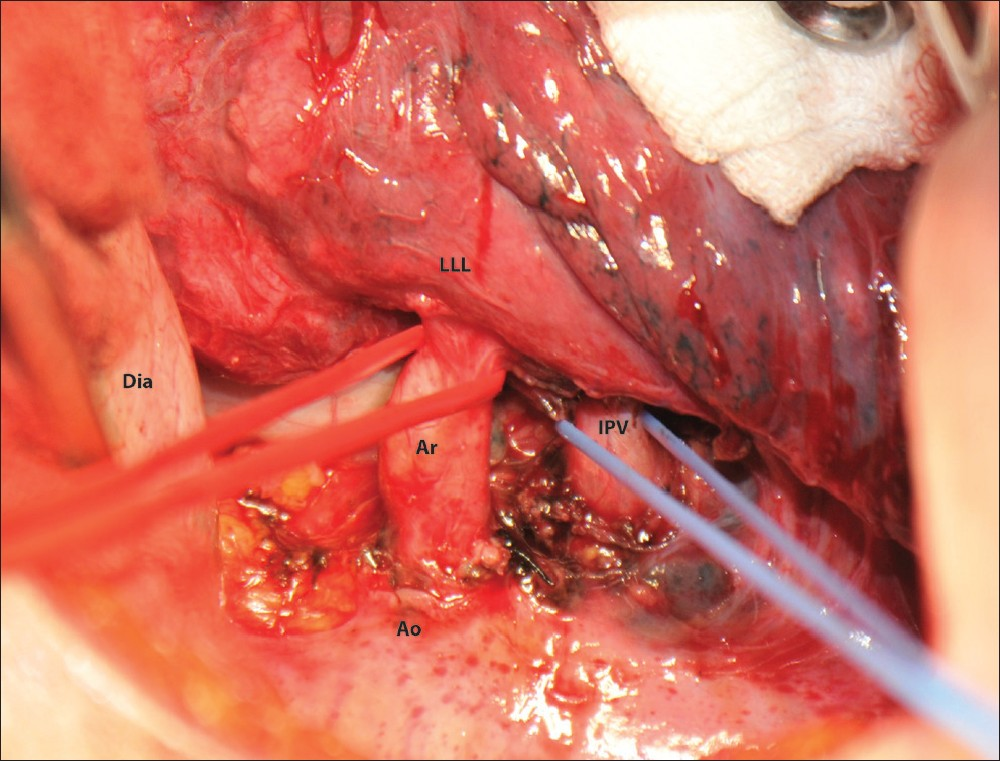
- Operative view of the patient. Dia: Diaphragm, Ao: Aorta, Ar: Aberrant artery, IPV: Inferior pulmonary vein, LLL: Left lower lobe.
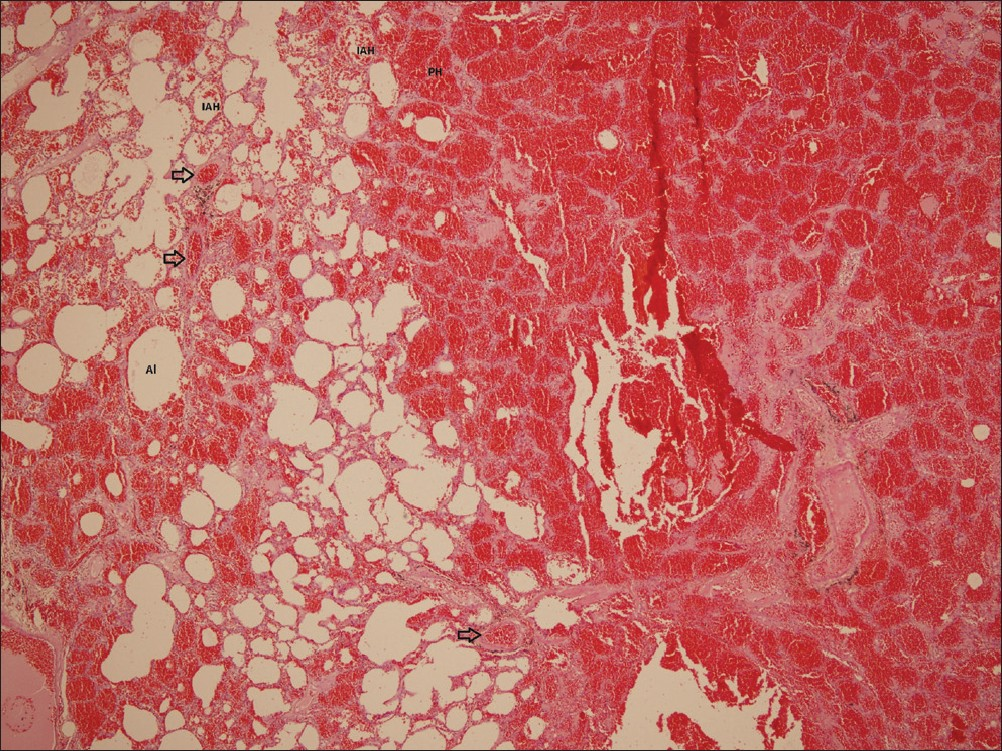
- H and E, ×40 magnification of the specimen reveals intra-alveolar hemorrhages (IAH), parenchymal hemorrhages (PH), and vascular congestions (arrow). Al: Alveolus.
DISCUSSION
The pathogenesis of pulmonary sequestration is controversial. Different theories have been proposed. It is reported that infections may have a role in occurrence of intrapulmonary sequestrations.[1] But congenital reasons cannot be excluded in etiology. Pulmonary sequestration is a remnant of ventral primitive foregut that migrates caudally. It occurs as a result of failure in obliteration of systemic vessels originating from early embryonic splanchnic vessels. Pulmonary sequestrations are usually asymptomatic and can be detected at any age, especially at the adolescence period of life. Hemoptysis and recurrent pulmonary infections may point to the diagnosis of sequestration. But these are similar to the symptoms of bronchiectasis. Particularly large aberrant arteries of sequestrations may cause some rare clinical manifestations like respiratory distress, congestive heart failure, nutritional deficiency, and back pain. In the present case, the patient did not have any characteristic history of illness during her childhood. But recurrent hemoptysis was the prominent symptom for 8 years without any specific diagnosis.
Pulmonary sequestration is the most common congenital abnormality of lung, accounting for 0.2-6.4% of all congenital pulmonary malformation.[2] Thoracic aorta is the most common source of systemic blood circulation for sequestrations. Abdominal aorta, intercostal artery, internal mammary artery, subclavian artery, and circumflex coronary artery can be the other rare sources. The common venous drainage is to the pulmonary vessels.[3] Pryce[4] first described and classified the pulmonary sequestration as intralobar (ILS) and extralobar (ELS) types. The major differences being location and venous drainage of sequestrated lung; typically, ILS is located within the normal visceral pleura with normal venous drainage to left atrium, whereas ELS has its own visceral pleura and anomalous venous drainage into systemic veins routing to the right atrium. ILS makes up 75% of all pulmonary sequestrations.[35] The most frequently involved lung tissue in pulmonary sequestration is the left basal segment with left superior segment spared, as we reported in this case. The present case was diagnosed as ILS during the operation.
Diagnosing pulmonary sequestration is based on imaging and identifying the systemic arterial supply. Arteriography is the method of choice to demonstrate the systemic vessels supplying the abnormal portion of the lung.[6] Several studies mainly consisting of case reports have shown that magnetic resonance imaging and multidetector CT angiography can be used to demonstrate the aberrant vasculature and the bronchial anatomy.[6–8] Chest radiography of ILS reveals an irregular-margined consolidation; sometimes, tortuous vessel-like structure can be visualized. Contrast-enhanced CT or CT angiography can clearly delineate the origin and course of the anomalous systemic artery. Sequestrated lung in ILS typically contains multiple cysts filled with fluid or thick mucus, and persistent mucus secreting into ectatic bronchi may also evolve to cystic change.[9] Pulmonary sequestration was diagnosed with the help of multidetector computed tomographic angiography and aortography in this case.
Surgical intervention should be performed to protect lung parenchyma and to prevent possible complications and infections when diagnosis is made early. Chest roentgenogram is generally not pathognomonic and may reveal a pulmonary consolidated lesion similar to what is seen in pneumonia, or a soft tissue mass with well-defined edges and air-fluid levels.[3] Morbidity and even mortality may occur as a result of massive hemorrhage because of infection due to the air transfer between the normal pulmonary parenchyma and sequestration area. Microscopic connections allow bacterial transfer leading to bacterial infections. ILS rarely causes problems during childhood and 15% of adult patients do not have any complaints when the sequestration is discovered.[2] ILS generally affects the basal segments of the lower pulmonary lobes and are located on the left side in most of the cases. The treatment of pulmonary sequestration is surgery. Attention must be paid to the pseudotumoral forms of sequestration because preoperative massive bleeding from the aberrant vessel may occur in cases of sub-diaphragmatic origin, the artery retracting into the abdomen cavity and causing fatal hemorrhage, as reported previously.[2]
Resection of sequestrated lung can be performed by thoracotomy or video-assisted thoracoscopic surgery (VATS).[10] It is reported that sequestrectomy (resection of the sequestered lobe) is frequently applied for ELS, whereas lobectomy or segmentectomy is preferred for ILS. VATS resection is preferred for a better cosmetic result and to reduce the risk of postoperative complications and the longer hospital stays. Para-aortic arterial structures must be controlled during the operation to avoid fatal hemorrhage. For this reason, we performed systemic arterial dissection very carefully during lower lobectomy in this case. The patient was discharged 7 days after the surgery. No complications or hemoptysis were detected in the patient 4 months following the operation.
CONCLUSION
Pulmonary sequestrations should be included in the differential diagnosis of recurrent hemoptysis and pulmonary infections. In order to prevent possible massive hemoptysis, surgical treatment should be carefully planned. Preoperative imaging avoids lethal complications during the operations of these patients.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/71/104304
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Intralobar pulmonary sequestration: A clinical and pathological spectrum. J Pediatr Surg. 1993;28:802-5.
- [Google Scholar]
- Lung sequestration: Report of seven cases and review of 540 published cases. Thorax. 1979;34:96-101.
- [Google Scholar]
- Diagnosis and surgical treatment of pulmonary sequestration. Thorac Cardiovasc Surg. 2008;56:154-7.
- [Google Scholar]
- Lower accessory pulmonary artery with intralobar sequestration of lung; a report of seven cases. J Pathol Bacteriol. 1946;58:457-67.
- [Google Scholar]
- Pulmonary sequestration: A single-institutional series composed of 27 cases. J Thorac Cardiovasc Surg. 2007;133:955-9.
- [Google Scholar]
- Computed tomography and magnetic resonance imaging: Past, present and future. Eur Respir J Suppl. 2002;35:3-12s.
- [Google Scholar]
- Multidetector CT angiography in pulmonary sequestration. J Comput Assist Tomogr. 2006;30:926-32.
- [Google Scholar]
- Intralobar sequestration: Radiologic-pathologic correlation. Radiographics. 1997;17:725-45.
- [Google Scholar]
- Thoracoscopic treatment of pulmonary sequestration. Eur J Cardiothorac Surg. 2006;29:815-8.
- [Google Scholar]






