Translate this page into:
Integrating Ultrasound Teaching into Preclinical Problem-based Learning
Address for correspondence: Dr. Eli Tumba Tshibwabwa, Department of Clinical Medicine, College of Medicine, American University of Antigua, University Park, Jabberwock Beach Road, Coolidge, Antigua, Barbuda. E-mail: etumba@auamed.net
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
The aim is to provide students in the preclinical with ultrasound image interpretation skills. Research question: Are students in smaller groups with access to a combination of lectures and hands-on patient contact most likely to have better ultrasound image interpretation skills, than students in larger groups with only interactive didactic lectures?
Methodology:
First-year students at the preclinical Program of the College of Medicine, participated in two 2-h introductory interactive ultrasound sessions. The study comprised two cohorts: 2012/2013 students, who were offered large group teaching (LGT) sessions (control group), and 2013/2014 students, who received the intervention in small group learning problem-based learning (PBL) sessions (experimental group). The overall learning objectives were identical for both groups. The success of the module was evaluated using pre- and post-tests as well as students’ feedback.
Results:
The students in the experimental group showed significantly higher scores in interpretations of images than those in the control group. The experimental group showed achievement of learning outcomes along with higher levels of satisfaction with the module compared to the latter.
Conclusion:
Posttest knowledge of the basics of ultrasound improved significantly over the pretest in the experimental group. In addition, students’ overall satisfaction of the ultrasound module was shown to be higher for the PBL compared to the LGT groups. Small groups in an interactive and PBL setting along with opportunities for hands-on practice and simultaneous visualization of findings on a high definition screen should enhance preclinical student learning of the basics of ultrasound. Despite the potential of ultrasound as a clinical, teaching and learning tool for students in the preclinical years, standardized recommendations have yet to be created regarding its integration into the curricula within academic institutions and clinical medicine. The interactive and PBL is here to stay at the college of medicine. Further research would be carried out to see if this trend persists in the upcoming vertical system-based curriculum of the college of medicine.
Keywords
Diagnostic radiology
education and administration
problem-based learning
ultrasound teaching
undergraduate medical program

INTRODUCTION
Internationally, there is heightened interest in integrating ultrasonography into medical education in the preclinical years, with a particular focus on training standards, knowledge, and experience.[123456789101112131415] However, its place in the preclinical curriculum is currently very diverse.[1357810111213161718] For example, the University of Ottawa began exploring ways to integrate ultrasound into its undergraduate medical program.[16] Further, the First World Congress on ultrasound in medical education hosted by the University of South Carolina,[17] and the American Academy of Emergency Medicine[18] recommended the integration of ultrasound into the core undergraduate medical school curriculum. Accordingly, the Alliance of Medical Students Educators in Radiology (AMSER) has outlined goals and objectives for both preclinical and clinical years.[319]
Joining this trend, in winter 2012, the College of Medicine offered an introduction to ultrasound module in its introduction to the clinical medicine-2 course, which is taught in the second semester of the 1st year. This course was first offered as a large group teaching (LGT) event, then a student-centered, problem-based, small group learning approach was introduced in fall 2013.
The aim of the current study, conducted between fall 2012 and winter 2014, was to help medical students of a modified problem-based learning (PBL) system develop basic ultrasound image interpretation skills for abdomen and cardiac regions with a focus on basic principles, terminology, and clinical applications. PBL can be defined best “as the learning that results from the process of working toward the understanding or resolution of a problem. The problem is encountered first in the learning process”[20,p.1]. Furthermore “ In PBL, students work in small collaborative groups and learn what they need to know in order to solve a problem”[21,p.235]. Indeed “PBL is intended to equip students with hands-on learning strategies to help them meet their future responsibilities”[22,p.1].
Few studies have assessed the impact of a preclinical integrated ultrasound teaching in PBL on the acquisition of basic ultrasound knowledge by undergraduate medical students. The research question guiding this study was: Are students in smaller groups with access to a combination of lectures and hands-on patient contact most likely to have better ultrasound image interpretation skills, than students in larger groups with only interactive didactic lectures?
METHODOLOGY
Ethics
The Research Council of the college of medicine approved the study.
Study setting and population
Participants were students from the college of medicine who enrolled in the introduction to clinical medicine-2 course during the study [Table 1]. Their age ranged from 19 to 24 years.
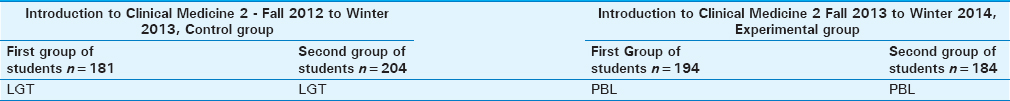
The control group
It consisted of students taking the course in the previous year, who were taught introductory ultrasound within the setting of traditional LGT, 181 (82 males and 99 females) and 204 (83 males and 121 females) in the 2012 fall and 2013 winter semesters, respectively.
Furthermore, having attended during their first semester a mandatory introductory 1-h LGT by the first author on the fundamental principles of radiology, all the participants had had prior exposure to the same amount of information on basic imaging (i.e., how plain films, computerized tomography, magnetic resonance imaging, and ultrasound images are formed, what are the factors contributing to image appearances of each of these techniques?). It was the authors’ expectation that, at the start of this study, the students would relate their ultrasound experience to their prior knowledge of the imaging techniques listed above, so as to enhance and accelerate their understanding of the ultrasound module.
To assist students in determining where to start for the upcoming session the following resources were suggested:
-
Ultrasound anatomy – an imaging resource published by the first author for medical students in their journey throughout the medical foundations. This brochure introduces the students to the basics of ultrasound, physics and device, how to use a portable equipment to acquire basic anatomy, demonstration of abdominal, pelvic and vascular anatomy and small parts, along with images of normal and pathologies specific to structures and vascular flow as well as to the Focused Assessment with Ultrasound in Trauma (FAST)
-
An accompanying PowerPoint presentation on introductory ultrasound, which was prepared by the first author (with integrated interactive elements). Furthermore, PowerPoint included the learning objectives of the ultrasound module [Table 2].
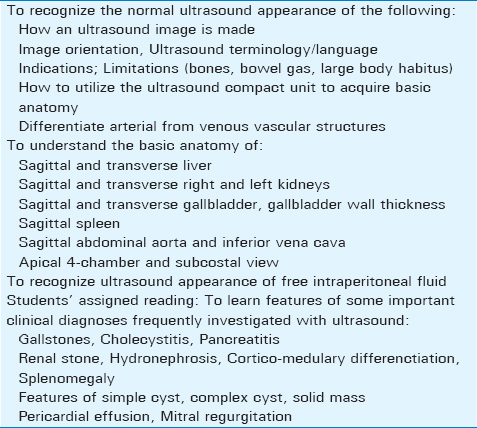
The overall goals and objectives are consistent with the AMSER National Medical Student Curriculum in Radiology for preclinical years.[319]
One radiologist-educator – the first author with ultrasound teaching as his area of subspecialty interest and with prior PBL involvement served as the single instructor and lecturer for all the large group and small group sessions. Branstetter et al.,[23] Tshibwabwa et al.,[1213] have demonstrated in earlier studies involving undergraduate medical students that one radiologist suffices for conducting these types of ultrasound sessions. Therefore, one radiologist educator was felt adequate for initiating the ultrasound module.
Students in all large groups were constantly challenged with relevant questions so as to support learning, and provide equal opportunity to all for enhancing their understanding of the core material. Each group participated in 2 × 2-h interactive sessions on separate days within the setting of LGT.
Whenever the students were presented with a probable or desirable variety of pathologies [Table 2], they would take advantage of this opportunity to make links with their knowledge of normal, for example, different echogenicities in the identification of abnormal aspects, thickened gallbladder wall in cholecystitis, renal stones, corticomedullary differentiation, and splenomegaly. During LGT the faculty used PowerPoint presentation to demonstrate normal ultrasound anatomy of specific abdominal structures as a stimulus for discussion and demonstration and discussion of some important clinical diagnoses frequently investigated with ultrasound.
The session-relevant learning materials were disseminated through the school's learning management system (blackboard: elearning.auamed.net). In preparation for interactive sessions, the students were advised to review the learning materials on introduction to ultrasound, ahead of the LGT.
The experimental group
It consisted of students taking the course when the ultrasound module was first integrated into a PBL setting, 194 (101 males and 93 females) and 184 (81 males and 103 females) in the 2013 fall and 2014 winter semesters, respectively. Unlike the students in the control group, the students in the intervention group were split up into smaller groups of size 6 or 7.
Intervention
The PBL students had access to the same preparatory materials as the control group.
Furthermore, the local objectives for hands-on were also consistent with the overall learning objectives for the introductory ultrasound module, i.e., identification of organ structures and insights into the normal appearances of kidneys, liver, spleen, gallbladder, aorta, and inferior vena cava as well as identification of blood flow in aorta, renal vessels. Allowing the students in these PBL to work along the same overall learning objectives for ultrasound module [Table 2] enabled consistency and comparison of the groups.
Moreover, for the PBL, each 2-h session was divided into:
-
Ten minutes for the case presentation
-
Sixty minutes of hands-on ultrasound examination of a normal subject
-
Fifty minutes for review of the PowerPoint presentation and discussion.
Therefore with the facilitation of the faculty, each student in the small groups was expected to scan the abdomen focusing on the renal, liver, gallbladder, spleen, subcostal regions plus major abdominal vessels, and pattern of blood flow. In addition, the student scanned the cardiac region noting chamber and valvular morphology and activity as per ultrasound module [Table 2].
Due to the absence of healthy volunteers, students scanned each other, and this pattern would continue for 1 h with every student scanning a live model and peers participating in the discussion. The ultrasound machine was located in a smaller classroom, and images obtained were shown on the ultrasound's unit monitor and also on a large high-definition television display. The classroom was adequately lighted. Displaying on a high definition screen allowed for all students in the group to view the ultrasound images obtained by their peers, and to effectively participate in the discussion. An ideal subject, i.e., a student with a slim body habitus, could at times replace a student with a larger habitus. To maintain consistency of the anatomic structures on displayed images, each participant had to scan specific focused abdominal and cardiac regions (upper right quadrant, right and left flanks, subcostal, apical for the demonstration of structures of interest).
The duration to impart theoretical knowledge for both groups was identical, i.e., the experimental and control group had two theory sessions, each session lasting for 2 h. The experimental group had two additional hands-on sessions, each session lasting 50 min.
The ultrasound unit used was the Sonosite Micromaxx portable ultrasound (SonoSite, Inc. 21919 30th Drive SE, Bothell, WA 98021, USA) that was provided with a 13–6 MHz linear array transducer for musculoskeletal scans, a C60e curved transducer for abdominal scans, and a P17 transducer for cardiac scans [Figure 1].
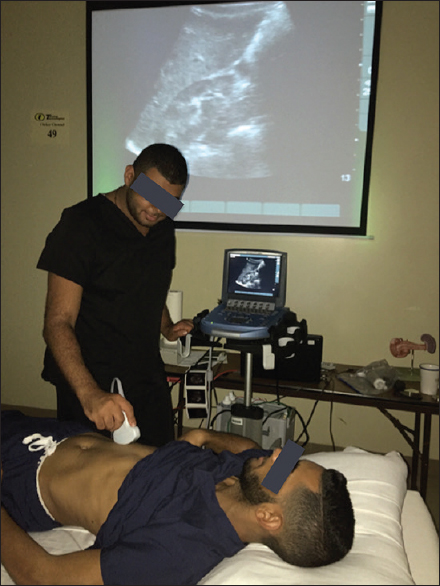
- Ultrasound room conditions during small group teaching. Images obtained during hands-on are simultaneously displayed on the screen of the compact micromax unit and the larger screen in the laboratory room allowing for all the students in the laboratory to view at the same time, and encouraging for team work. This student is scanning the right flank of his fellow along sagittal and transverse planes. Both screens are displaying the right kidney with its normal corticomedullary echotexture differentiation.
Evaluation
To this end, pre- or post-tests were used for testing knowledge. Sample questions are provided in Appendix 1. At the beginning of each session, a pretest including 10 identical multiple-choice questions was done to ascertain a baseline knowledge level of the participating students for both the LGT and PBL. The questions were identical for both groups, (even if the order of the topics varied). They were logically arranged with ascending complexity to test cumulative knowledge of the students in the following key areas of introductory ultrasound:
-
Orientation of the ultrasound probe with regard to the monitor of the ultrasound machine (two questions)
-
Scanning planes (two questions)
-
Ultrasound terminology (two questions)
-
Identification of organ structures and blood flow (two questions)
-
Clinical applications (two questions).
At the conclusion of LGT and PBL, a posttest study including again 10 different questions, identical for all large and small groups (with the varied order of topics) was performed to test the students in the same key areas of the module, i.e., principles, terminology, anatomy, clinical application. Students’ answers were scored for a maximum total of 10 points. Evaluation of the differences between pre- and post-test students’ scores/results was made with a paired t-test.
The validity of tests item was referenced to the goals and objectives of the ultrasound module with items referring to similar areas as in cases and clinical vignettes used for LGT, PBL and PowerPoint presentation. All multiple choice questions for the formative and summative assessment were set by the first author and were similar in scope, and complexity for all the topics within the introduction to clinical medicine-2 block. The multiple choice questions aimed at testing students’ knowledge of ultrasound basics.
The practical aspects of ultrasound of the abdominal and/or cardiac regions were still tested on a 5-point Likert scale (5 = excellent; 4 = very good; 3 = good; 2 = fair; and 1 = poor), even though these had been taught for a short duration. Here again, pre- and post-test were done.
Regarding the objective criteria for excellent scanning, etc., students were evaluated by following assessments: Be able to:
-
Identify the organ of interest by showing its normal echotexture
-
Show sagittal and transverse scanning planes
-
Describe the organ echotexture (using ultrasound terminology).
Data collection and student's participation
In all LGT and PBL classrooms at the college of medicine, the students were issued a response card (RF Audience Response device) henceforth referred to as a “clicker.” The clicker interfaced with the software Turning Point (Turning Technologies Headquarters, 255 West Federal Street, Youngstown, Ohio 44503, USA) and Microsoft PowerPoint to record the students’ selection of answers to various multiple-choice questions and to provide immediate feedback at the start and conclusion of the session. The clicker was chosen for data collection in this study because it has been deemed as an efficient method of collecting data within a classroom setting and at the same time allows students’ participation.
RESULTS
The age range of the students was quite narrow, and so the authors were sure about the complete and even “unfamiliarity” of the majority of the students to ultrasound imaging. Allowing the students to work along the same overall learning objectives for ultrasound session enabled consistency and comparability of the groups.
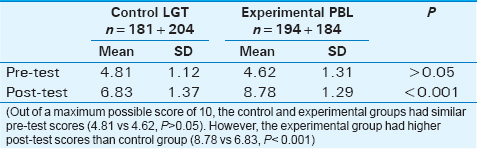
The results of all the sets of multiple-choice questions for both the LGT and PBL are summarized in Table 3. Out of a maximum possible score of 10, the control and experimental groups had similar pretest scores (4.81 vs. 4.62, P > 0.05). However, the experimental group had higher posttest scores than control group (8.78 vs. 6.83, P < 0.001).
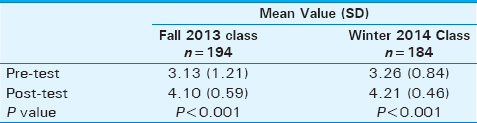
In addition, the results for the hands’ on examination are summarized in Table 4. The mean scores for the hands-on practice performed by the students on each other during the ultrasound PBL, for the fall 2013 and winter 2014 groups, were respectively 3.13 out of 5 and 3.26 out of 5 on the pretest study, and 4.10 out of 5 and 4.21 out of 5 on the posttest with (P < 0.001).
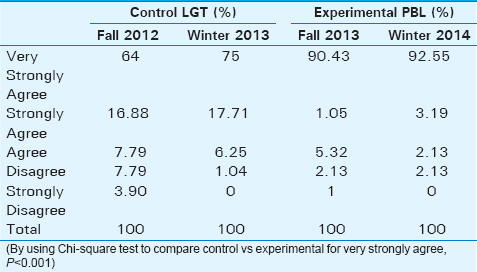
A larger percentage of students in the experimental group strongly agreed that the session was useful (91% in experimental vs. 70% in control, P < 0.001) [Table 5].
DISCUSSION
It is not surprising that students preferred smaller groups and hands-on patient contact as it is shown from the students’ opinions regarding their overall satisfaction with the ultrasound module [Table 5]. Furthermore, previous publications showing this trend are available.[125781213]
Although the first group did not have hands-on experience, the learning outcomes to be achieved by students in PBL and LGT are shown to be identical, and this again had allowed for comparison. Furthermore, to keep consistency, all large and small groups were taught by the same faculty radiologist. Of course, were PBL hands-on been offered at the beginning of this study, it would not have been surprising that all the students would have preferred smaller groups and hands-on patient contact.[1231213]
The 10 min × 2 were deemed enough for initial training for students who came prepared for the PBL session. A previous European study gave students about 10–15 min for ultrasound hands-on;[24] at a tertiary care academic medical center in Ohio, the students were given 15 min for FAST and pelvic scan and 8 min for vascular and cardiac hands-on.[25] Ultrasound devices have been referred to as “the stethoscopes of the 21st century”[26] and numerous studies tout the benefits of their use,[27282930] including “teaching physical examination in medical schools”[30,p.e58] and “an important role both in detecting DCIS (Ductal Carcinoma In Situ) and in evaluating histopathological features.”[31,p.54]
There was a significant improvement over time for PBL groups (P < 0.001). The exposure to combined hands-on experience and PBL might have helped the students in PBL enhance their acquired theoretical “knowledge” of images interpretation, i.e., basics of ultrasound and focused clinical application. Two previous studies looking at the inclusion of ultrasound in the undergraduate medical program at McMaster University showed the effectiveness of using ultrasound teaching to introduce related technology and enhance students’ learning of topographical and dynamic anatomy.[1213] However, in those studies, there was no control group, and the portable machines used may have been acceptable to gain a first glance but they were certainly not ideal (the screen was quite small and probably difficult for all students in the PBL to view at the same time, even if room surroundings were adequately lighted). In other studies with handheld ultrasonographic imaging devices for PBL,[251024] again laboratory room details were not detailed.
The strength of the current study lies in the definition of PBL approach and the inclusion of a control group that received an introduction to ultrasound in a traditional LGT setting. The room conditions are well detailed, and images obtained during hands-on performed by one student on another are displayed simultaneously on the small screen and a larger television [Figure 1]. Such room environment might allow for PBL to take its course as all the students in the PBL could view the findings at the same time and discuss them to facilitate student learning and enhance their own and group's understanding of the concepts at hand.
Integration of the ultrasound module into an introduction to clinical medicine-2 course reinforced the students’ understanding of case-based PBL in an innovative and active way. Dreher et al., found that students’ “interest and self-perceived experience, comfort, and confidence in ultrasound skills significantly increased (P < 0.001) as a result of this early introduction to ultrasonography.”[32,p. 231] From this study, it becomes clear that LGT in the second semester requires a commitment from one full-time radiologist faculty-the introduction to clinical medicine radiology theme coordinator of about 4–5 h for preparation of the educational material, i.e. lectures and questions for knowledge evaluation and exactly 2 h × 2 for the scheduled lectures; high definition digital displays in the classroom are necessary. However, PBL requires additional resource. For preclinical schools with annual students intake in the range of the semester 2 intake (i.e., approximately 200 students at the college of medicine) and interest in the integration of ultrasound into their program, more teaching radiologists, i.e., 3 or 4 will be needed to sustain a more vertically oriented ultrasound curriculum to guide simultaneously more small groups of students during hands-on training and confirm images interpretation sessions. To limit faculty involvement, sonographers, and local part-time radiologists along with ongoing workshops for faculty and groups of preclinical students with an interest in Radiology or Emergency Medicine and Obstetrics will reduce the time commitment of an individual teaching radiologist faculty. If additional teaching radiologists are available, the training of motivated faculty by the teaching radiologist or a visiting radiologist would be seen crucial to the sustainability of the project. Furthermore refurbished compact ultrasound units with 1-year warranty or the less expensive first generation of compact units are commercially available and shown to be reliable alternative to the new units.
With regard to limitations of this study, statistical analysis was restricted to a descriptive exploration. Furthermore, the survey results cannot be generalized because they were heavily based on the current curriculum at the college of medicine.
CONCLUSION
From the present study, we conclude that posttest knowledge of the basics of ultrasound improved significantly over the pretest in the experimental group. In addition, students’ overall satisfaction of the ultrasound module was shown to be higher for the PBL compared to the LGT groups. Further research would be carried out to see if this trend persists in the upcoming vertical system-based curriculum of the college of medicine.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/38/190897
REFERENCES
- Integrated medical school ultrasound: Development of an ultrasound vertical curriculum. Crit Ultrasound J. 2013;5:6.
- [Google Scholar]
- Bedside ultrasound education in Canadian medical schools: A national survey. Can Med Educ J. 2016;7:e78-86.
- [Google Scholar]
- Anatomy teaching with portable ultrasound to medical students. BMC Med Educ. 2012;12:99.
- [Google Scholar]
- A pilot study of comprehensive ultrasound education at the Wayne State University School of Medicine: A pioneer year review. J Ultrasound Med. 2008;27:745-9.
- [Google Scholar]
- The changing landscape of radiology: Ultrasound training for nonradiologists. Can Assoc Radiol J. 2014;65:1.
- [Google Scholar]
- Ultrasound-based teaching of cardiac anatomy and physiology to undergraduate medical students. Arch Cardiovasc Dis. 2013;106:487-91.
- [Google Scholar]
- An integrated ultrasound curriculum (iUSC) for medical students: 4-year experience. Crit Ultrasound J. 2011;3:1-12.
- [Google Scholar]
- Undergraduate student perceptions of the use of ultrasonography in the study of “living anatomy”. Anat Sci Educ. 2010;3:318-22.
- [Google Scholar]
- Ultrasonography in preclinical education: A pilot study. J Am Osteopath Assoc. 2008;108:601-5.
- [Google Scholar]
- Does ultrasound training boost year 1 medical student competence and confidence when learning abdominal examination? Med Educ. 2007;41:843-8.
- [Google Scholar]
- Integration of ultrasound in the education programme in anatomy. Med Educ. 2005;39:1148.
- [Google Scholar]
- Teaching musculoskeletal ultrasound in the undergraduate medical curriculum. Med Educ. 2007;41:517-8.
- [Google Scholar]
- Teaching cardiovascular anatomy to medical students by using a handheld ultrasound device. JAMA. 2002;288:1062-3.
- [Google Scholar]
- The utilisation of radiology for the teaching of anatomy in Canadian medical schools. Can Assoc Radiol J. 2012;63:160-4.
- [Google Scholar]
- Designing multi-disciplinary undergraduate medical school ultrasonography curriculum. UOJM. 2014;4:49-54.
- [Google Scholar]
- First World Congress on ultrasound in medical education hosted by the University of South Carolina School of Medicine. J S C Med Assoc. 2011;107:189-90.
- [Google Scholar]
- AAEM Clinical Practice Committee Statement: Ultrasound Should be Integrated into Undergraduate Medical Curriculum. Available from: http://www.aaem.org/UserFiles/UltrasoundCPCStatement.pdf
- [Google Scholar]
- AMSER National Medical Student Curriculum in Radiology. 2012. Available from: http://www.aur.org/Secondary-Alliances.aspx?id=141
- [Google Scholar]
- Problem-Based Learning: An Approach to Medical Education. New York: Springer; 1980.
- [Google Scholar]
- Preclinical medical student training in radiology: The effect of early exposure. AJR Am J Roentgenol. 2007;188:W9-14.
- [Google Scholar]
- The ultrasound challenge: A novel approach to medical student ultrasound education. J Ultrasound Med. 2012;31:2013-6.
- [Google Scholar]
- Portable bedside ultrasound: The visual stethoscope of the 21st century. Scand J Trauma Resusc Emerg Med. 2012;20:18.
- [Google Scholar]
- Sonographic physical diagnosis 101: Teaching senior medical students basic ultrasound scanning skills using a compact ultrasound system. Ultrasound Q. 2007;23:157-60.
- [Google Scholar]
- Teaching ultrasound in a curricular course according to certified EFSUMB standards during undergraduate medical education: A prospective study. BMC Med Educ. 2013;13:84.
- [Google Scholar]
- Medical educators’ perspectives of teaching physical examinations using ultrasonography at the undergraduate level. Can Med Educ J. 2013;4:e59-68.
- [Google Scholar]
- Diagnostic evaluation of ductal carcinoma in situ of the breast: Ultrasonographic, mammographic and histopathologic correlations. Ultrasound Med Biol. 2015;41:47-55.
- [Google Scholar]
APPENDIX 1. QUESTIONS FOR KNOWLEDGE TESTING
Multiple-Choice Questions. Choose the one alternative that best completes the statement or answers the probing question
Part A. Questions for testing familiarization with orientation planes, scanning, terminology, indications and normal anatomy
A 22-year old woman with unexplained persistent epigastric pain was seen at the gastroenterology clinic, and a referral for abdominal ultrasound and other imaging for pancreas was made. Correlative CT of the abdomen is provided for comparison. Which of the following statement most likely describe the plane of the cross-sectional imaging on both the ultrasound and CT scans?
Longitudinal Coronal Sagittal Transverse Para-sagittal A 29-year-old obese man presents to his family physician with colicky pain radiating to the hypochondrium for 3 days. An ultrasound scan showed a small hyperechoic structure with posterior shadow consistent with a renal stone. An arrow is pointing at the lesion in the affected organ. Which of the following best describes the anatomic plane of the ultrasound scan?
Sagittal Coronal Oblique Axial Transverse A 22-year old female with unexplained persistent epigastric pain was seen at the gastroenterology clinic, and a referral for abdominal ultrasound and other imaging for pancreas was made. Correlative CT of the abdomen is provided for comparison. Which of the following terms most likely describe the appearance of the pancreas indicated by the blue arrow on the abdominal ultrasound scan?
Isoechoic relative to adjacent liver Hypoechoic relative to adjacent liver Hyperintense Hyperechoic relative to the liver parenchyma Isodense relative to the liver A 50-year-old woman with abnormal blood renal function suggestive of acute renal function was seen at the nephrology clinic. Ultrasound of the kidneys showed gross hydronephrosis. Ultrasound scan(Sagittal) of the right kidney is attached for your reference. Which of the following statement is consistent with the upper limit of normal for the thickness of the renal parenchyma in this patient?
8-10 mm 6-8 mm 10-12 mm 4-6 mm 11- 13 mm A 26-year-old pregnant woman with acute left flank pain was seen in the Emergency Department. Diagnostic imaging was done, and findings were consistent with a small renal stone. Which modality is the most commonly used and the most effective modality for the assessment of the stone in pregnant women and children?
IVU (Intravenous Urography) Plain radiograph-Abdomen Ultrasound CT MRI
Part B. Questions for testing abnormal findings, e.g., characterization of masses: cystic, solid, complex; evaluation of right upper quadrant pain, flank pain, pericardial effusion
A 40-year-old man presents to his family physician with a scenario of “right upper quadrant (RUQ) pain? Gallstones”. An ultrasound scan of the abdomen was requested, and was reported as showing several small mobile structures in the gallbladder consistent with cholelithiasis (gallstones). Which of the following terms correctly describes the findings indicated by the arrow.
Hypoechoic relative to surrounding gallbladder wall Hyperechoic wihout posterior enhancement Anechoic with posterior enhancement Hyperechoic with posterior shadow Isoechoic relative to adjacent gallbladder wall A 37- year-old patient with right upper quadrant pain was seen at the hepatology clinic. Referral for ultrasound scan of the abdomen was done. Liver showed several solid masses scattered consistent with liver metastases. Which of the following term will most likely describe these lesions (red arrows) on this sagittal scan of the liver? A normal liver scan in the same plane is provided for comparison.
Isoechoic Hyperechoic Anechoic Hypoechoic Mixed pattern A 48-year-old woman presents to the nephrology clinic with symptoms and signs of acute renal failure. Hydronephrosis is suspected due to an enlarged fibroid uterus compressing the right ureter. Which type of radiologic imaging study is the most commonly used in the assessment of hydronephrosis?
Ultrasound CT scan of the pelvis MRI Plain abdominal film Fluoroscopy A 41-year-old man with known renal simple cyst presents to her family physician for follow-up of a large simple cyst in the upper pole of his right kidney. Kidneys ultrasound was done, and comparison with previous ultrasound images did not show any changes of the lesion. Which of the following will best describe the ultrasound appearances of the cystic lesion?
Anechoic with internal hyperechoic debris Hypoechoic Isoechoic Thin- walled anechoic without internal echoic debris Hyperechoic with posterior shadow A 31-year old man with right lower quadrant pain was seen at his Family Practice, and a request for abdominal imaging. Plain X-ray of the abdomen was inconclusive, and a subsequent abdominal ultrasound showed a small solid nodule in the peripheral area of the right liver lobe consistent with liver hemangioma. Which of the following will best describe the ultrasound appearances of this benign solid tumor?
Anechoic with internal hyperechoic debris Hypoechoic Isoechoic Thin- walled anechoic without internal echoic debris Hyperechoic without posterior shadow






