Translate this page into:
Inflammatory Pseudotumor of the Kidney
Address for correspondence: Dr. Mehmet Ruhi Onur, Firat Universitesi Hastanesi Rektorluk kampusu 23119, Elazig, Turkey. ruhionur@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Inflammatory pseudotumor of the kidney is a rare benign condition with unknown etiology that can mimic malignancy. We report a case of inflammatory pseudotumor of the kidney. A 59-year-old male patient was admitted with a complaint of right flank pain and hematuria. Ultrasonography and magnetic resonance imaging of the patient revealed a 9 cm × 10 cm mass originating from the renal parenchyma with posterior extension. Operative findings revealed a mass adhering to the psoas muscle. Histopathologic examination demonstrated spindle-shaped fibroblast cells accompanying inflammatory cells. The pathological diagnosis was renal inflammatory pseudotumor. Repeated US and computed tomography revealed complete remission.
Keywords
Inflammatory pseudotumor
kidney
magnetic resonance imaging
ultrasonography
INTRODUCTION

Inflammatory pseudotumor (IPT) of the kidney is a rare benign condition with unknown etiology that can mimic malignancy.[1] IPT may develop at several anatomic sites including air passages, gastrointestinal tissues, soft tissues, orbit, spleen, liver, lymph nodes, and kidneys, but IPT occuring at the renal site is extremely rare.[2] The correct diagnosis can be established with histopathologic examination when the characteristic finding of an admixed inflammatory and fibroblastic infiltrate is recognized.[3] Ultrasonography (US) and computed tomography (CT) findings of IPT are nonspecific and do not include distinguishing features.[1] However, magnetic resonance imaging (MRI) may be useful in the diagnosis of IPT. In this report, we present US and MRI findings of inflammatory pseudotumor of the kidney.
CASE REPORT
A 59-year-old male patient was admitted to our hospital with complaints of right flank pain and hematuria. Increased neutrophil count with normal white blood cell level and high blood urea nitrogen (BUN) (82 mg/dL, normal range: 10-50 mg/dL) and creatinine (2.7 mg/dL, normal range: 0.6-1.2 mg/dL) levels were found on laboratory examination. A hypoechoic, heterogeneous, solid renal mass seen on US was attributed to renal malignancy [Figure 1]. T1 weighted MRI demonstrated a hypointense mass measuring 9 cm × 10 cm originating from the upper pole of the kidney. T2 weighted sequence revealed peripheral solid component to be hypointense and central cystic component to be bright. Other imaging features were invasion of the psoas muscle posteriorly and enhancement of the mass in the delayed phase after intravenous gadolinium injection [Figure 2]. On the basis of the clinical and radiological findings, a malignancy such as renal cell carcinoma (RCC) was suspected. The patient had exploratory surgery, since the mass was adhering to the psoas muscle, the surgeon did not resect the mass and the kidney. A large volume of tissue was obtained during the surgery for histopathology evaluation. Chronic inflammatory cells with vimentin positive myofibroblastic cells were seen in histopathologic examination with no evidence of malignancy.
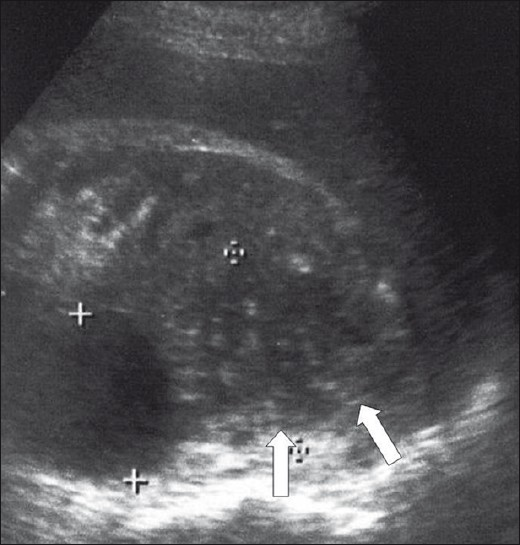
- Gray-scale longitudinal image of the right kidney shows a hypoechoic mass (arrows) measuring approximately 5 cm. There is an anechoic cortical cyst beside this lesion.
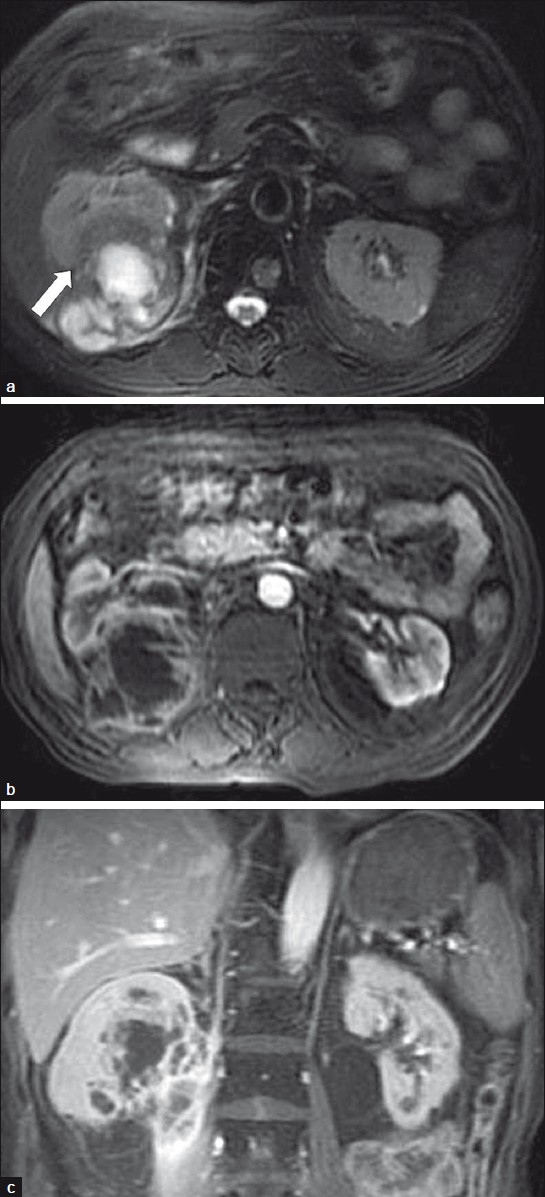
- (a) T2-weighted MRI reveals a right renal parenchymal mass (arrow) located posteriorly with peripheral hypointense solid and central hyperintense cystic component and extension to the paraspinal/pernephric region. (b) After gadolinium administration, axial image shows that peripheral solid component and septa formations of lesion enhance earlier but less than the surrounding renal parenchyma, suggesting malignancy. (c) Coronal image shows septal enhancement and extension of the right renal mass into the psoas muscle. There is no extension into the renal vein.
The patient had palliative medical treatment and the CT done 3 months later revealed significant regression in the size of the mass lesion with the relief of symptoms [Figure 3]. MRI of the patient performed 6 months after the operation showed complete regression of the lesion in the right kidney. The patient is currently free of disease, 1 year after the initial diagnosis.
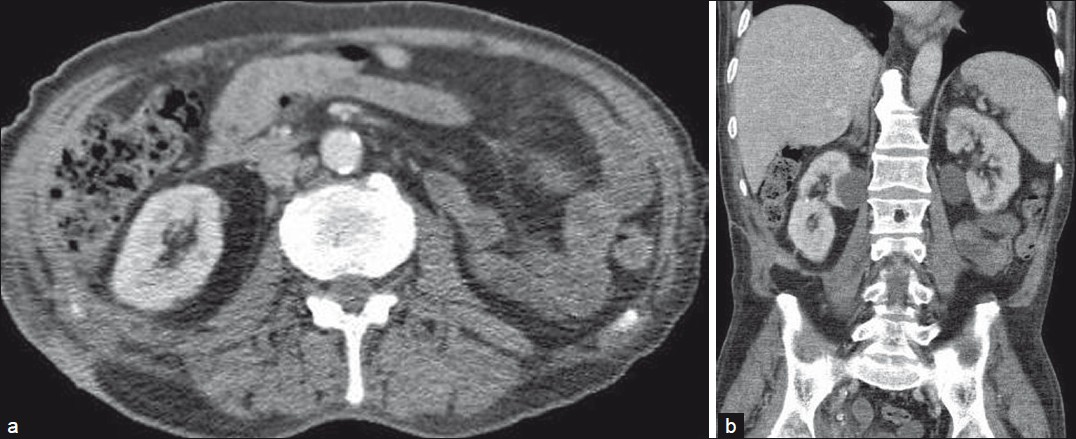
- Six months after the first presentation of the patient, the CT examination conducted after administration of iodinated contrast agent yielded complete resolution of the right renal mass on (a) axial and (b) coronal images.
DISCUSSION
Benign and malignant pathologies of the kidney sometimes mimic each other. Imaging findings are essential for correct medical evaluation and to prevent unnecessary invasive procedures.
Inflammatory pseudotumor of the kidney represents a benign disease of the kidney, characterized by proliferative myofibroblasts, fibroblasts, histiocytes, and plasma cells.[4] Most patients with IPT have nonspecific clinical presentation of pain, dysuria, hematuria, fever, and urinary tract infections.[1] Etiology of this entity is uncertain, but the lesion is generally regarded as reactive or postinfectious, originating from an inflammatory process. As in our patient, it may also occur without any known cause.[4] IPT in the kidney is a rare occurence and it is important to remember that misdiagnosis of this lesion as a renal malignancy is a possibility.
Even needle biopsies and operation findings would be inadequate for the diagnosis of IPT of the kidney. Diagnosis mainly depends on a combination of clinical and imaging findings and the presence of regression of lesion at follow-up imaging examinations of the patient, in addition to a histopathologic examination.
Imaging of these patients reveals renal mass lesions of varying sizes with variable imaging characteristics.[1] An IPT may present as a well-circumscribed, polypoid, locally aggressive, or infiltrating mass. US demonstrates a variable pattern of echogenicity, and the lesion has been described as hypo- or hyperechogenic with ill-defined or well-circumscribed margins. Immunohistochemical and ultrastructural studies confirm a myofibroblastic differentiation in IPT that could be the reason for its solid appearance on US.[2] Enhanced CT may demonstrate homo- or heterogeneity and hypo-, iso-, or hyperdensity. These variable radiologic findings may be attributed to varying degrees of fibrosis, cellular infiltration, and dynamic change occurring during the inflammatory process.[4] US of our patient showed a hypoechoic mass with undefined boundaries representing a solid mass. According to US findings, RCC was the most favorable diagnosis.
Imaging findings of IPT on MRI are not emphasized adequately in the literature. According to reports, IPT was seen hypointense on T2-weighted images.[5] MRI findings in our IPT case are similar to reported cases in literature [Figure 2a] Presence of enhancing septae within the central cystic component of the mass along with its extension to involve right psoas muscle led us to the diagnosis of cystic RCC. The differential diagnosis of IPT of the kidney includes renal cell carcinoma, mesenchymal sarcomas such as leiomyosarcoma, sarcomatoid carcinoma, xanthogranulomatous pyelonephritis, plasma cell granuloma, malignant fibrous histiocytoma, and urothelial carcinoma.[1] All of these may show imaging findings similar to IPT. However, renal sarcomas appear as expansile masses while rhabdomyosarcoma and angiosarcoma of the kidney display an infiltrative pattern.[6] Also, xanthogranulomatous pyelonephritis usually has a specific clinical history that indicates chronic inflammation. Differentiation between IPT and cystic RCC remains controversial. MRI may be useful for determining the cystic and infiltrative component of the IPT. Also, the infiltrative nature of IPT that is seen more easily on MRI may be an important distinctive feature for differentiation between RCC and IPT, since RCCs manifest as infiltrative lesions in only about 6% of cases.[7] Additionally, the enhancement pattern of IPT may distinguish these lesions from RCC, since the enhancement of IPT begins in the arterial phase but increases in the venous phase. Delayed enhancement of IPT is probably due to an accumulation of extravascular contrast media in the fibrotic component of the lesion.[8]
MRI and multidetector CT may help the radiologists by demonstrating the infiltrative nature and enhancement pattern of IPT in the kidney.
CONCLUSION
In this report, we have presented an IPT of the kidney, misdiagnosed on US and MRI as cystic RCC. Awareness of imaging findings in IPT will help the radiologists in the assessment of patients with atypical imaging features of renal masses. MRI may help the radiologists by showing the infiltrative nature and enhancement pattern of the lesion more clearly. Despite its rare occurrence, IPT should be used in differential diagnosis while evaluating renal masses.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/7/75252
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Inflammatory pseudotumor of the kidney: A case report. Int Urol Nephrol. 2004;36:137-40.
- [Google Scholar]
- Radiologic findings of renal inflammatory pseudotumor: A case report. Korean J Radiol. 2000;1:219-22.
- [Google Scholar]
- Inflammatory pseudotumor of the kidney with renal artery penetration. Radiat Med. 2007;25:541-7.
- [Google Scholar]
- From the archives of the AFIP.Infiltrative renal lesions: radiologic-pathologic correlation. Radiographics. 2000;20:215-43.
- [Google Scholar]
- Radiology in the diagnosis and staging of renal cell carcinoma. Crit Rev Diagn Imaging. 1990;31:81-115.
- [Google Scholar]
- Inflammatory pseudotumor (myoblastic tumor) of the genitourinary tract. AJR Am J Roentgenol. 2008;191:1255-62.
- [Google Scholar]






